Abstract
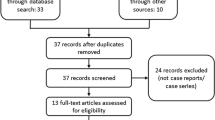
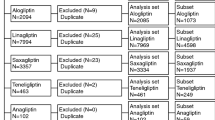
In the recent past, concerns have raised regarding the potential risk of acute pancreatitis among type 2 diabetic patients using incretin-based drugs such as glucagon-like peptide 1 (GLP-1) analogs and dipeptidyl peptidase 4 (DPP-4) inhibitors. The aim of this study is to investigate the association between exposure to incretin-based drugs and the occurrence of pancreatitis reported in the French Pharmacovigilance Database. The case/non-case method was performed from serious adverse drug reactions (ADRs) involving antihyperglycemic agents (except insulin alone) reported to the French pharmacovigilance system between March 2008 (first marketing of an incretin-based drug in France) and March 2013. Cases were defined as reports of pancreatitis, and all other serious ADRs were considered non-cases. Disproportionality was assessed by calculating reporting odds ratios (ROR) adjusted for age, gender, history of pancreatitis, other antihyperglycemic drugs and other drugs associated with a higher risk of pancreatitis. Among 3,109 serious ADRs, 147 (4.7 %) reports of pancreatitis were identified as cases and 2,962 reports (95.3 %) of other ADRs as non-cases. Among the cases, 122 (83.0 %) involved incretin-based drugs. Disproportionality was found for all incretin-based drugs (adjusted ROR: 15.7 [95 % CI 9.8–24.9]), all GLP-1 analogs (29.4 [16.0–53.8]), exenatide (28.3 [12.8–62.3]), liraglutide (30.4 [15.4–60.0]), all DPP-4 inhibitors (12.1 [7.3–20.0]), sitagliptin (12.4 [7.3–21.0]), saxagliptin (15.1 [4.3–52.7]), and vildagliptin (7.4 [3.1–17.6]). Temporal analysis found disproportionality for incretin-based drugs since their first year of marketing in France. Compared with other antihyperglycemic agents, use of incretin-based drugs is associated with an increased risk of reported pancreatitis in France.


Similar content being viewed by others
References
Information for Healthcare Professionals: Exenatide (marketed as Byetta)—8/2008 Update. Available from http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm124713.htm, accessed 11 May 2012
Elashoff M, Matveyenko AV, Gier B, Elashoff R, Butler PC (2011) Pancreatitis, pancreatic, and thyroid cancer with glucagon-like peptide-1-based therapies. Gastroenterology 141:150–156
Hawkes N (2011) Journal withdraws article after complaints from drug manufacturers. BMJ 342:d2335
Hauben M, Patadia V, Gerrits C, Walsh L, Reich L (2005) Data mining in pharmacovigilance: the need for a balanced perspective. Drug Saf 28:835–842
Raschi E, Piccinni C, Poluzzi E, Marchesini G, De Ponti F (2013) The association of pancreatitis with antidiabetic drug use: gaining insight through the FDA pharmacovigilance database. Acta Diabetol 50:569–577
Hauben M, Madigan D, Gerrits CM, Walsh L, Van Puijenbroek EP (2005) The role of data mining in pharmacovigilance. Expert Opin Drug Saf 4:929–948
Wilson AM, Thabane L, Holbrook A (2004) Application of data mining techniques in pharmacovigilance. Br J Clin Pharmacol 57:127–134
Bate A, Evans SJ (2009) Quantitative signal detection using spontaneous ADR reporting. Pharmacoepidemiol Drug Saf 18:427–436
Moore N, Kreft-Jais C, Haramburu F et al (1997) Reports of hypoglycaemia associated with the use of ACE inhibitors and other drugs: a case/non-case study in the French pharmacovigilance system database. Br J Clin Pharmacol 44:513–518
Balani AR, Grendell JH (2008) Drug-induced pancreatitis: incidence, management and prevention. Drug Saf 31:823–837
Pariente A, Gregoire F, Fourrier-Reglat A, Haramburu F, Moore N (2007) Impact of safety alerts on measures of disproportionality in spontaneous reporting databases: the notoriety bias. Drug Saf 30:891–898
Hazell L, Shakir SA (2006) Under-reporting of adverse drug reactions: a systematic review. Drug Saf 29:385–396
Cohen D (2013) Reports of pancreatitis are 20–30 times more likely with GLP-1 drugs, analysis finds. BMJ 346:f2607
Institute for Safe Medication Practices (2013) Perspectives on GLP-1 agents for diabetes. Available from http://www.ismp.org/QuarterWatch/pdfs/2012Q3.pdf
van der Heijden PG, van Puijenbroek EP, van Buuren S, van der Hofstede JW (2002) On the assessment of adverse drug reactions from spontaneous reporting systems: the influence of under-reporting on odds ratios. Stat Med 21:2027–2044
Galvus (vildagliptin) Summaries of Product Characteristics. EMA 2012. Available from http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000771/WC500020327.pdf
Onglyza (liraglutide) Summaries of Product Characteristics. EMA 2012. Available from http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/001026/WC500050017.pdf
Byetta (exenatide) Summaries of Product Characteristics. EMA 2012. Available from http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000698/WC500051845.pdf
Januvia (sitagliptin) Summaries of Product Characteristics. EMA 2012. Available from http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000722/WC500039054.pdf
Onglyza (saxagliptin) Summaries of Product Characteristics. EMA 2012. Available from http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/001039/WC500044316.pdf
Gonzalez-Perez A, Schlienger RG, Rodriguez LA (2010) Acute pancreatitis in association with type 2 diabetes and antidiabetic drugs: a population-based cohort study. Diabetes Care 33:2580–2585
Noel RA, Braun DK, Patterson RE, Bloomgren GL (2009) Increased risk of acute pancreatitis and biliary disease observed in patients with type 2 diabetes: a retrospective cohort study. Diabetes Care 32:834–838
Girman CJ, Kou TD, Cai B et al (2010) Patients with type 2 diabetes mellitus have higher risk for acute pancreatitis compared with those without diabetes. Diabetes Obes Metab 12:766–771
Montastruc JL, Sommet A, Bagheri H, Lapeyre-Mestre M (2011) Benefits and strengths of the disproportionality analysis for identification of adverse drug reactions in a pharmacovigilance database. Br J Clin Pharmacol 72:905–908
Sommet A, Grolleau S, Bagheri H, Lapeyre-Mestre M, Montastruc JL (2008) Was the thrombotic risk of rofecoxib predictable from the French Pharmacovigilance Database before 30 September 2004? Eur J Clin Pharmacol 64:829–834
Matveyenko AV, Dry S, Cox HI et al (2009) Beneficial endocrine but adverse exocrine effects of sitagliptin in the human islet amyloid polypeptide transgenic rat model of type 2 diabetes: interactions with metformin. Diabetes 58:1604–1615
Butler PC, Elashoff M, Elashoff R, Gale EA (2013) A critical analysis of the clinical use of incretin-based therapies: are the GLP-1 therapies safe? Diabetes Care 36:2118–2125
Butler AE, Campbell-Thompson M, Gurlo T, Dawson DW, Atkinson M, Butler PC (2013) Marked expansion of exocrine and endocrine pancreas with incretin therapy in humans with increased exocrine pancreas dysplasia and the potential for glucagon-producing neuroendocrine tumors. Diabetes 62:2595–2604
Nauck MA (2013) A critical analysis of the clinical use of incretin-based therapies: the benefits by far outweigh the potential risks. Diabetes Care 36:2126–2132
Kahn SE (2013) Incretin therapy and islet pathology: a time for caution. Diabetes 62:2178–2180
Drucker DJ (2013) Incretin action in the pancreas: potential promise, possible perils, and pathological pitfalls. Diabetes 62:3316–3323
Alves C, Batel-Marques F, Macedo AF (2012) A meta-analysis of serious adverse events reported with exenatide and liraglutide: acute pancreatitis and cancer. Diabetes Res Clin Pract 98:271–284
Engel SS, Round E, Golm GT, Kaufman KD, Goldstein BJ (2013) Safety and tolerability of sitagliptin in type 2 diabetes: pooled analysis of 25 clinical studies. Diabetes Ther 4:119–145
Scirica BM, Bhatt DL, Braunwald E et al (2013) Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med 369:1317–1326
White WB, Cannon CP, Heller SR et al (2013) Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med 369:1327–1335
Dore DD, Bloomgren GL, Wenten M et al (2011) A cohort study of acute pancreatitis in relation to exenatide use. Diabetes Obes Metab 13:559–566
Dore DD, Seeger JD, Arnold Chan K (2009) Use of a claims-based active drug safety surveillance system to assess the risk of acute pancreatitis with exenatide or sitagliptin compared to metformin or glyburide. Curr Med Res Opin 25:1019–1027
Garg R, Chen W, Pendergrass M (2010) Acute pancreatitis in type 2 diabetes treated with exenatide or sitagliptin: a retrospective observational pharmacy claims analysis. Diabetes Care 33:2349–2354
Romley JA, Goldman DP, Solomon M, McFadden D, Peters AL (2012) Exenatide therapy and the risk of pancreatitis and pancreatic cancer in a privately insured population. Diabetes Technol Ther 14:904–911
Wenten M, Gaebler JA, Hussein M et al (2012) Relative risk of acute pancreatitis in initiators of exenatide twice daily compared with other anti-diabetic medication: a follow-up study. Diabet Med 29:1412–1418
Singh S, Chang HY, Richards TM, Weiner JP, Clark JM, Segal JB (2013) Glucagonlike peptide 1-based therapies and risk of hospitalization for acute pancreatitis in type 2 diabetes mellitus: a population-based matched case–control study. JAMA Intern Med 173:534–539
Eurich DT, Simpson S, Senthilselvan A, Asche CV, Sandhu-Minhas JK, McAlister FA (2013) Comparative safety and effectiveness of sitagliptin in patients with type 2 diabetes: retrospective population based cohort study. BMJ 346:f2267
Acknowledgments
The authors thank the French Network of Pharmacovigilance Centres and Pascal Auriche (ANSM) for access and extraction of data from the French Pharmacovigilance Database. The authors assume responsibility for the content and conclusions of this article.
Conflict of interest
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Communicated by Massimo Porta.
Rights and permissions
About this article
Cite this article
Faillie, JL., Babai, S., Crépin, S. et al. Pancreatitis associated with the use of GLP-1 analogs and DPP-4 inhibitors: a case/non-case study from the French Pharmacovigilance Database. Acta Diabetol 51, 491–497 (2014). https://doi.org/10.1007/s00592-013-0544-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-013-0544-0