Abstract
Introduction
The photodynamic bone stabilization system (PBSS) was was developed in 2010, and in 2018 gained FDA approval in the United States. Given its relative novelty, our analysis sought to analyze the available literature exploring the indications, outcomes, and complications of the PBSS.
Methods
We performed a systematic review (PROSPERO registration of study protocol: CRD42022363065, October 8th, 2022). PubMed, EBSCOHost, and Google Scholar electronic databases were queried to identify articles evaluating PBSS in the treatment of pathologic or traumatic fractures between January 1 2010 and 15 October 2022. The quality of the included studies was assessed using the Methodological Index for Nonrandomized Studies tool.
Results
Our initial search yielded 326 publications, which were then screened for appropriate studies that aligned with the purpose of our review. A total of thirteen studies, comprising seven case series, four case reports, and two cohort studies. The total sample size of the included studies consisted of 345 patients, with 242 females (70%) and 103 males (30%). The implants were most commonly utilized in the humerus (41%), radius (12%), and metacarpal (12%). The most common complications were related to broken implants (5%) and dislocation (1%). Most studies reported complete fracture healing and return of full strength and range of motion.
Conclusion
Despite being a relatively novel technology, PBSS appears to be a viable option for fracture stabilization. Most studies included in our analysis reported complete fracture healing and return of function with minimal complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A photodynamic bone stabilization system (PBSS) was developed in 2010 for the treatment of fractures, especially pathologic, osteoporotic, and impending fractures [1, 2]. The system is based on a light curable monomer within a balloon catheter that can provide longitudinal and rotational stability by conforming to the shape of the intramedullary canal upon exposure to blue light to form a rigid implant in the target bone [3]. Currently, this technology has obtained approval from the United States Food and Drug Administration (FDA) for investigational device usage within the United States. Additionally, it is currently being utilized in clinical settings in several European countries, such as Germany, Austria, Switzerland, and Italy [2, 4,5,6].
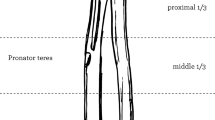
While traditional methods of fracture stabilization such as intramedullary nails and plate fixation are capable of providing sufficient stabilization in healthy bone, they are not specifically designed or suitable for addressing fragility fractures that arise due to weakened, osteoporotic bone. The PBSS offers several advantages in the treatment of fractures and impending fractures. It allows for minimally invasive surgery through a percutaneous incision with preservation of endosteal blood supply and decreases the disruption of muscular attachments [7]. The system employs a light-cured, on-demand polymerizing mechanism that, unlike bone cement that hardens rapidly, affords the surgeon the flexibility and adequate time to achieve the appropriate reduction of the fracture before polymerization takes place (Fig. 1). Several studies have found this system effective in treating fractures of the tibia, fibula, and humerus, exhibiting minimal complications and high rates of fracture healing [2, 7,8,9].
To better understand the current interventions and overall efficacy, we conducted a systematic review to evaluate the utilization, complications, patient-reported outcomes, and radiographic outcomes of PBSS.
Methods
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines (PRISMA) [10]. The study protocol was registered prospectively with PROSPERO registration of the study protocol was CRD42022363065, October 8th, 2022.
Literature search
The PubMed, EBSCO Host, and Google Scholar electronic databases were queried with the following keywords or MeSH terms in combination with ‘AND’ or ‘OR’ Boolean operators: ‘photodynamic bone stabilization [MeSH]’; ‘Illuminoss’; ‘bone stabilization system’; ‘intramedullary stabilization’; ‘intramedullary osteosynthesis’; ‘Fracture [MeSH]; ‘Osteolyses’; ‘Osteolysis’; ‘Indications’; ‘advantages’; ‘limitations;’ ‘limits;’ ‘outcomes’; ‘follow-up’; ‘management’; ‘safety’; ‘recovery’; and ‘treatment’ to identify all studies that evaluated PBSS in the treatment of pathologic or traumatic fractures between 1 January 2010 and 15 October 2022.
Articles were included if the following criteria were met: (1) full-text articles in English are available, (2) the study evaluated the PBSS in the treatment of a fracture(s), (3) the study used live human subjects, and (4) identified an outcome (e.g., survival, complications, radiologic outcomes, functional outcomes). Review articles, cadaver studies, and animal studies were excluded.
Study selection
Two reviewers independently assessed the eligibility of each article included in the review. In the case of disagreement, a third reviewer was consulted to reach consensus. The initial query yielded 326 publications, which were then screened for relevant studies for the purposes of our review. After removing duplicates and reviewing each abstract for relevancy 23 were selected for full text review. Of these, 13 fulfilled our inclusion and exclusion criteria. A thorough review of each reference’s list did not yield any additional studies. The selection process is shown in Fig. 2.
Data collection
A collaborative spreadsheet, arranged by two reviewers before starting, facilitated data extraction. Study characteristics and outcomes were extracted from each study and verified by a second reviewer. Characteristics extracted included publication year, medical journal, study design, level of evidence, total study population, age, sex, number of fractures, fracture type (traumatic or pathologic), and fracture location. In addition, outcomes related to complications, radiographic, and functional findings were recorded. Complications were further classified as intraoperative complications (any complication reported during the operative procedure), postoperative device-related complications, and non-device-related complications. Radiographic and functional findings were reported descriptively due to the heterogeneity of the fractures being analyzed in the included studies.
Risk of bias in individual studies
The risk of bias was assessed by two independent reviewers using the MINORS tool. This is a validated assessment tool that assigns a value from 0 to 24 to comparative studies based on 12 criteria related to study design, outcomes assessed, and follow-up. Higher scores indicate a higher quality of study. Across these domains, each item is graded with a 2 when adequately reported, 1 when reported but inadequate, and 0 if not reported. Any discrepancies in the grading were resolved by discussion and consultation with a third reviewer. Case reports were not eligible for MINORS and excluded from the risk of bias assessment [11].
Results
Included studies
There were thirteen studies, comprising seven case series, four case reports, and two cohort studies included in the final analysis (Table 1). The studies were performed in Europe (77%) and North America (13%). The total sample size of the included studies consisted of 345 patients, with 242 females (70%) and 103 males (30%). The mean age range was 30–80 years old. A total of 370 fractures were recorded, with 260 (70%) traumatic fractures and 110 (30%) pathologic fractures. The location of these fractures included 141 humeral fractures, 12 femoral fractures, 43 radius fractures, 29 ulna fractures, 43 hand fractures, 36 pelvic fractures, 4 tibia fractures, 36 fibula fractures, and 1 fracture of the sternum (Table 2). The mean ± standard deviation (SD) MINORS score was 12 ± 1.7.
Complications
One Level III [9], Eight Level IV [1, 2, 5,6,7, 12,13,14], and three Level V [8, 15, 16] studies reported complications following PBSS. A total of sixty complications were reported (Table 3). Post-operative non-device related complications comprised a majority of all complications (35; 58%). One intra-operative device failure (2%) was due to incomplete resin curing. The most common post-operative device-related complications were due to breakage of the implant (16; 27%), device dislocation (3; 5%), and implant protrusion (2; 3%).
Radiographic findings
Radiographic outcomes were reported by six Level IV studies and one Level V study (Table 4). Three studies[2, 5, 12] assessing fractures of the distal radius, metacarpals, humerus, and pelvis found complete fracture healing in all patients at 12-month follow up. Similarly, two studies [1, 14] found 96% fracture healing among pelvic and humerus fractures, respectively. One study [16] reported evidence of fracture displacement on an individual with osteogenesis imperfecta type 4. Lastly, one study reported adequate treatment of a pathologic humerus fracture in a patient with metastatic renal cancer.
Two studies [5, 12] reported angulation reduction after operation with the PBSS. Two studies [2, 12] found minimal limb shortening in a majority of their patients with one study [12] reporting a median of 2 mm shortening in fifth metacarpal fractures, while another study [2] found 86% of patients who had radiographic follow up having absent or < 5 mm shortening in their heterogeneous fracture cohort.
Functional outcomes
Five Level IV and Two Level V studies reported functional outcomes (Table 4). Pain scores reported were overall minimal across studies. One study [5] found median pain scores of 0 at final follow up at rest and with activity. Three studies [7, 13, 14] utilized VAS scores to measure pain. VAS scores were consistently low in all studies, with one study [7] finding a significant decrease in VAS scores compared to baseline with up to 1 year of follow-up. DASH scores to measure disability were utilized in three studies [5, 7, 15] and demonstrated a significant downward trend of DASH scores reported until 1 year follow-up. Lastly, range of motion and strength were examined in five studies [1, 5, 7, 15, 17] which all found adequate range and strength recovery.
Discussion
PBSS may be used as an alternative to intramedullary nailing and plates in the correction in the fixation of both traumatic fractures and pathologic/impending fractures. The aim of our systematic review was to report the indications, complications, and functional and radiographic outcomes following PBSS implantation. Our analysis found that the PBSS system was utilized as a treatment option for a range of injuries, including traumatic and pathologic fractures in the upper extremities, lower extremities, chest, and pelvis. PBSS was associated with a low incidence of complications, with only a minority of cases attributed to the device itself. The most common device-related complication was implant breakage. There was only one intra-operative complication reported due to incomplete resin curing. The majority of studies found complete fracture healing and low patient-reported pain and disability scores by 12 months. While these findings are encouraging, the majority of studies were retrospective case series, and future prospective randomized trials and comparative studies are necessary to evaluate the efficacy of PBSS.
Complications
Our review of included studies showed a complication rate of 16% for the PBSS system, with 60% of these complications not related to the device. Among the device-related complications, breakage was the most common issue. Regarding device instillation, the PBSS had minimal intraoperative complications, with only one reported case of incomplete resin curing.
Compared to IMN and plate complication rates, PBSS offers a similar rate of overall complications. Distal radial fractures, for example, undergoing volar locking plates has a complication rate between 3 and 36% reported [18,19,20]. Similarly, among humeral shaft fractures, one study found complications of 58% for plating and 43% for IMN [21]. However, PBSS offers a number of benefits that may explain low rate of intra-operative complication rates. Our analysis found a majority of fractures treated with PBSS were humeral shaft fractures (Fig. 3). In the fixation of humeral fractures with IMN, a number of complications can occur such as protrusion of the nail can lead to pain and stiffness. Iatrogenic comminution can occur with previously reported rates of between 7 and 20%, and the diameter of the humeral canal may limit nailing efficiency. Furthermore, neurovascular injuries include risk to the radial nerve from the insertion of the nail, a risk to the axillary nerve from proximal locking, and a risk to the contents of the cubital fossa with distal locking [22]. The malleability of the intramedullary polymer in PBSS may provide an advantage over the limitations of plating fixation in terms of under or oversizing and misplacement [22]. PBSS can also offer stabilization with augmentation using a plate, which depends on the patient’s bone quality and density (Fig. 4). Patients with poorer quality of bone or lower density of bone may require this more comprehensive treatment.
Radiographic findings
The use of PBSS in the treatment of fractures has been associated with favorable Radiologic outcomes, including almost complete fracture healing, minimal limb shortening, and no implant migration. Two studies demonstrated complete radiographic healing in all patients within three months following PBSS fixation [2]. Similarly, a study on humeral fractures treated with PBSS had a healing rate of 96% in one year. In comparison, a prospective study comparing IMN and plating for humeral shaft fractures found healing rates of 93 and 87%, respectively, at an average follow-up of 16 weeks [21]. Nonetheless, not all patients with PBSS fixation had complete fracture healing. One study found four patients with limb deformities, three patients with > 5 mm shortening, and Recurvatum/procurvatum deformity present in five individuals [2]. Lastly, two studies found volar and dorsal angular deformities present at follow-up [5, 7]. Further research is warranted to comprehensively assess the radiographic outcomes of PBSS across a range of fracture types and anatomic locations.
Functional outcomes
The majority of studies found minimal pain scores with good recovery of function following PBSS. VAS scores were consistently low in all studies, with one study [7] finding a significant decrease in VAS scores compared to baseline with up to 1 year of follow-up. DASH scores to measure disability were utilized in three studies [5, 7, 15] and demonstrated a significant downward trend of DASH scores reported until 1 year follow-up. One study using PBSS for humeral shaft fracture reported a mean DASH score of 23.9 at one-year follow up. Similarly, a systematic review evaluating functional outcomes following locking plate fixation of humeral fractures found a similar DASH scores [23]. Lastly, the majority of studies found adequate range and strength recovery after 12 months. Given the reported functional findings thus far, PBSS seems to offer comparable functional outcomes compared to IMN and plating; however, research needs to directly compare these fixation modalities and their impact on functional recovery in patients with various types of fractures.
Cost effectiveness
As with any emerging novel technology, the economic effect of the PBSS should be discussed. In 2005, a model predicted the total number of fractures in the US to exceed 2 million and the economic cost to be $16.9 billion [24]. The model projected that number to increase to 3 million fractures per year at a cost of $25.3 billion in 2025. An analysis on economic burden among osteoporosis-related fracture in the Medicare US population found that the one of the highest costs included inpatient medical services and rehabilitation services, such as skilled nursing facilities [25]. One area that PBSS may have tangible effects on reducing healthcare cost and the economic burden on the healthcare system is decreasing inpatient hospital length of stay and expected faster recovery—which in turn, would lower costs of rehabilitation [26, 27]. However, there remains a need for an economic analysis on the impacts of the PBSS compared to traditional means of fracture repair to determine the effects of PBSS fixation on healthcare costs.
Limitations
There are several limitations to consider. First, given that PBSS is a relatively recent technology, a limited amount of data is available, which restricted our analysis. Consequently, included studies often had varying inclusion criteria, resulting in significant heterogeneity among studies regarding the type and location of the fractures and the outcome data reported. This heterogeneity prevented us from conducting a meta-analysis, and the results were instead presented descriptively. Additionally, while we utilized a rigorous systematic review protocol (PRISMA), our analysis is susceptible to publication bias, as studies with negative or null results may not have been published. Therefore, caution must be taken when interpreting the results of this systematic review, and future studies must address these limitations to enhance our understanding of PBSS's optimal use and long-term outcomes. Lastly, there are very few studies that directly compare outcomes related to alternative methods of fracture fixation such as IMN and plating. Furthermore, no prospective, randomized control trials have assessed the efficacy of PBSS.
Conclusion
The photodynamic bone stabilization system represents a promising option for fracture treatment across a range of fracture types, locations, and injury mechanisms. Both radiographic and functional outcomes have been favorable, with minimal device-related complications. While the existing literature primarily comprises non-comparative and retrospective studies, the results to date suggest that the PBSS has potential. More prospective randomized trials and comparative studies are necessary to evaluate the efficacy of PBSS relative to traditional fracture repair. Further research focuses on higher quality, randomized, and prospective data is required to fully understand the indications, optimal use, and long-term outcomes of PBSS.
References
Vegt P, Verbruggen J, Gausepohl T et al (2018) The photodynamic bone stabilization system in the treatment of humerus fractures: a prospective clinical trial. Cureus. https://doi.org/10.7759/CUREUS.2809
Gausepohl T, Pennig D, Heck S et al (2017) Effective management of bone fractures with the illuminoss® photodynamic bone stabilization system: initial clinical experience from the European Union registry. Orthop Rev (Pavia) 9:5–8. https://doi.org/10.4081/OR.2017.6988
Trost M, Knieps M, Hackl M et al (2022) Biomechanical comparison of different fixation methods in metatarsal shaft fractures: a cadaver study. Clin Biomech (Bristol, Avon). https://doi.org/10.1016/J.CLINBIOMECH.2022.105588
Hagenaars T, Van Oijen GW, Roerdink WH et al (2016) Functional recovery after treatment of extra-articular distal radius fractures in the elderly using the IlluminOss® System (IO-Wrist); a multicenter prospective observational study. BMC Musculoskelet Disord. https://doi.org/10.1186/S12891-016-1077-9
Van Oijen GW, Vegt PA, Hagenaars T et al (2021) Outcome after treatment of distal radius fractures in the elderly using the IlluminOss® System. Eur J Trauma Emerg Surg 47:1129–1136. https://doi.org/10.1007/S00068-019-01289-W
Krumme J, Macconnell A, Wallace M et al (2021) Early experience in pathologic humerus fracture treated with the photodynamic bone stabilization system shows limitations related to patient selection. Orthopedics 44:154–159. https://doi.org/10.3928/01477447-20210416-06
Vegt P, Muir JM, Block JE (2014) The photodynamic bone stabilization system: a minimally invasive, percutaneous intramedullary polymeric osteosynthesis for simple and complex long bone fractures. Med Devices (Auckl) 7:453–461. https://doi.org/10.2147/MDER.S71790
Fourman MS, Rothenberg AC, McGough RL et al (2020) Standalone photodynamic intramedullary implants in the treatment of bilateral refractory femoral nonunions in a patient with osteogenesis imperfecta: significant utility in load-bearing bones, but not a replacement for biomechanical optimization. Oper Tech Orthop 30:100805. https://doi.org/10.1016/J.OTO.2020.100805
Hoellwarth JS, Weiss K, Goodman M et al (2020) Evaluating the reoperation rate and hardware durability of three stabilizing implants for 105 malignant pathologic humerus fractures. Injury 51:947–954. https://doi.org/10.1016/J.INJURY.2020.02.124
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. https://doi.org/10.1136/BMJ.N71
Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716. https://doi.org/10.1046/J.1445-2197.2003.02748.X
Surke C, Meier R, Haug L, Vögelin E (2020) Osteosynthesis of fifth metacarpal neck fractures with a photodynamic polymer bone stabilization system. J Hand Surg Eur 45:119–125. https://doi.org/10.1177/1753193419880775
Zoccali C, Attala D, Pugliese M et al (2021) The IlluminOss® photodynamic bone stabilization system for pathological osteolyses and fractures of the humerus: indications, advantages and limits in a series of 12 patients at 24 months of minimum follow-up. BMC Musculoskelet Disord. https://doi.org/10.1186/S12891-020-03927-6
Oikonomidis S, Alabsi A, Ashqar G et al (2019) Intramedullary stabilization of pubic ramus fractures in elderly patients with a photodynamic bone stabilization system (IlluminOss). Geriatr Orthop Surg Rehabil. https://doi.org/10.1177/2151459318824904
Albertini U, Conti A, Ratto N et al (2020) Electrochemotherapy and simultaneous photodynamic bone stabilization of upper limbs in metastatic renal cancer disease: case report and literature review. Case Rep Med. https://doi.org/10.1155/2020/8408943
Meijering D, Harsevoort GJ, Janus AJM, van Helden SH (2018) Supracondylar femur fracture repair using IlluminOss in a patient with osteogenesis imperfecta type 4. J Orthop 15:663–665. https://doi.org/10.1016/J.JOR.2018.05.045
Pesch S, Gromer A, Beirer M et al (2019) Augmentation of simultaneous acetabular and femoral neck fracture in osteogenesis imperfecta using photodynamic bone stabilization–a case report. Trauma Case Rep. https://doi.org/10.1016/J.TCR.2019.100200
Williksen JH, Frihagen F, Hellund JC et al (2013) Volar locking plates versus external fixation and adjuvant pin fixation in unstable distal radius fractures: a randomized, controlled study. J Hand Surg Am 38:1469–1476. https://doi.org/10.1016/J.JHSA.2013.04.039
Arora R, Lutz M, Hennerbichler A et al (2007) Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma 21:316–322. https://doi.org/10.1097/BOT.0B013E318059B993
Wichlas F, Haas NP, Disch A et al (2014) Complication rates and reduction potential of palmar versus dorsal locking plate osteosynthesis for the treatment of distal radius fractures. J Orthop Traumatol 15:259–264. https://doi.org/10.1007/S10195-014-0306-Y
Chapman JR, Henley MB, Agel J, Benca PJ (2000) Randomized prospective study of humeral shaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma 14:162–166. https://doi.org/10.1097/00005131-200003000-00002
Farragos AF, Schemitsch EH, McKee MD (1999) Complications of intramedullary nailing for fractures of the humeral shaft: a review. J Orthop Trauma 13:258–267. https://doi.org/10.1097/00005131-199905000-00006
Sproul RC, Iyengar JJ, Devcic Z, Feeley BT (2011) A systematic review of locking plate fixation of proximal humerus fractures. Injury 42:408–413. https://doi.org/10.1016/J.INJURY.2010.11.058
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res Off J Am Soc Bone Miner Res 22(3):465–475. https://doi.org/10.1359/jbmr.061113
Williams SA, Daigle SG, Weiss R, Wang Y, Arora T, Curtis JR (2021) Economic burden of osteoporosis-related fractures in the US medicare population. Ann Pharmacother 55(7):821–829. https://doi.org/10.1177/1060028020970518
Hagenaars T, Van Oijen GW, Roerdink WH et al (2016) Functional recovery after treatment of extra-articular distal radius fractures in the elderly using the IlluminOss® System (IO-Wrist); a multicenter prospective observational study. BMC Musculoskelet Disord 17:235. https://doi.org/10.1186/s12891-016-1077-9
BONEZONE by ORTHOWORLD Inc. IlluminOSS presents novel approach to fracture fixation. BONEZONE, June 14, 2021. https://bonezonepub.com/2014/04/09/illuminoss-offers-novel-approach-to-fracture-fixation/
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or private sector.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Waived by the Cleveland Clinic Foundation, Cleveland, OH, USA. One of the authors (AFK) certifies receipt of personal payments or benefits, during the study period, in an amount of USD 10,000 to USD 100,000 from DePuy, a Johnson & Johnson Company; in an amount of USD 10,000 to USD 100,000 from Zimmer Biomet; in an amount less than USD 10,000 from Innomed; in an amount less than USD 10,000 from Proctor and Gamble; and in an amount less than USD 10,000 from Signature Orthopedics. The other authors that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, K.Y., McNassor, R., Hecht II, C.J. et al. Photodynamic bone stabilization for traumatic and pathologic fractures: a systematic review of utilization, complications, and patient-reported outcomes. Eur J Orthop Surg Traumatol 34, 1269–1277 (2024). https://doi.org/10.1007/s00590-024-03833-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-024-03833-w