Abstract
Objectives
The design of tibial trays for total knee arthroplasty (TKA) has been a topic of research for several decades. Although all-polyethylene trays were developed to address issues such as osteolysis and to enhance the longevity of the prosthesis, as well as knee range of motion, metal-backed designs have remained the most commonly used type of prosthesis. This meta-analysis aimed to compare the clinical, radiological, and survival outcomes of both designs.
Methods
Five databases were searched from inception until October 1, 2020, for randomized controlled trials (RCTs) that compared the outcomes of all-polyethylene and metal-backed tibial components in TKA. The outcomes of interest included range of motion, knee society score, stairs climbing scores, radiostereographic analysis, survivorship and complication. This review was conducted in line with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Risk of bias was assessed using the Newcastle–Ottawa tool.
Results
A total of 14 RCTs with 1367 TKA were included with a mean age of – years and – years for all-polyethylene and metal-backed tibial components groups, respectively. All-polyethylene group demonstrated statistically significant differences in five-year survivorship (OR 0.27; 95% CI 0.10–0.75; p value 0.01) and stairs climbing score (OR − 2.07; 95% CI − 3.27–0.87; p value 0.0007) when compared to the metal-backed group. The metal-backed design was significantly more radiographically stable in anterior–posterior, varus–valgus, and internal–external rotations at the 2-year follow-up compared to all-polyethylene tibias (OR − 0.09; 95% CI − 0.16 to − 0.02; p value 0.02) as per the pooled radiostereographic analysis. However, ten-year survivorship (OR 0.92; 95% CI 0.53–1.60; p value 0.78), range of motion (OR − 0.57; 95% CI − 2.00–0.85, p value 0.43), knee society scores (OR 1.38; 95% CI − 0.47–3.23, p value 0.14), and complications (OR 0.83; 95% CI 0.5–1.39, p value 0.48) were comparable between both groups.
Conclusions
While this meta-analysis suggests that all-polyethylene tibial components in total knee arthroplasty may offer advantages over metal-backed components in terms of five-year survivorship, and stairs climbing score, this finding should be considered in the context of potential confounding factors. Nonetheless, based on the results, the all-polyethylene implant should be considered a viable choice for primary knee replacement.
Level of evidence
I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metal-backed tibial components have been the preferred implant design in knee replacement surgeries over the all-polyethylene counterpart since their introduction in the 1970s. The first generations of all-polyethylene tibias were hindered by drawbacks such as osteolysis and earlier implant failure, leading to decreased popularity among arthroplasty surgeons over the last few decades [1, 2]. However, the theoretical value of modularity made the metal-backed option more attractive.
The all-polyethylene tibias used in TKA are renowned for their reliability, minimal bone resection requirements, and lack of implant migration and backside wear. Furthermore, the all-polyethylene design is significantly more cost-effective than the metal-backed alternative [3, 4]. This is particularly advantageous given the increasing demand for knee replacements worldwide, with the potential to reduce implant costs by up to 50% [5, 6]. Recent advances in all-polyethylene tibial components have demonstrated equivalent clinical reliability when compared to metal-backed designs [2].
The concept of modularity in metal-backed tibial components is appealing, as evidenced by several biomechanical studies showing its theoretical advantages in load distribution and resistance to implant failure [7, 8]. Additionally, the ability to remove the polyethylene liner without affecting the tibial fixation simplifies revision for bearing wear. There is also the potential for improved motion with reduced thickness or greater stability with a thicker insert. However, despite these theoretical benefits, none have been shown to have clinical significance. In contrast, drawbacks of metal-backed tibial components include backside wear caused by micromotion at the polyethylene–metal interface, and the need for a larger bone cut to accommodate the metal tray at the expense of a thinner polyethylene liner [9, 10].
The purpose of this study was to present the most comprehensive evidence comparing all-polyethylene and metal-backed tibial components in total knee arthroplasty. We evaluated various clinical and radiological variables from the studies included in our analysis. We hypothesized that there would be no significant difference between the two groups in terms of survivorship, functional outcomes, and complication rates.
Materials and methods
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, with a PRISMA checklist and algorithm [11].
Search strategy
PubMed/Medline, CINAHL, Cochrane, Embase, and Google Scholar databases were systematically searched from inception until October 1, 2020, to identify articles in peer-reviewed journals. The search was performed using the following keywords and their derivatives: "Knee arthroplasty," "Knee replacement," "Joint replacement," "Total knee," "Tibial," "All-polyethylene," "Metal-backed," "Tibail tray," "Randomized," and "RCT." Search results were screened against the eligibility criteria by two authors independently based on the title and/or abstract. Conflicts were resolved via a discrepancy meeting with a third, more senior author. A full-text review of articles that met the eligibility criteria was performed, and references of included articles were manually sought to ensure all relevant studies were included.
Outcomes of interest
The study evaluated several outcomes of interest, including range of motion, clinical and functional knee society scores at the final follow-up, stair climbing scores at one and five years, survivorship at five and ten years, and overall complication rates. Radiostereographic analysis was pooled at two years, encompassing anterior–posterior rotation, internal–external rotation migration, and varus–valgus malalignment.
Eligibility criteria
Inclusion criteria
-
1.
All original comparative level I of evidence RCTs reporting primary TKA indicated in all-polyethylene versus metal-backed tibial components.
-
2.
Studies with a minimum follow-up period of one year.
-
3.
RCTs that published complete manuscript with available data in English.
-
4.
RCTs that published clear outcome measures with attached data presented as or can be transferred to mean and standard deviation values.
Exclusion criteria
-
1.
Non-comparative or not reporting outcomes.
-
2.
Review articles, cross-sectional, case series and reports.
-
3.
Preclinical or animal studies.
-
4.
Studies with incomplete or unextractable data.
-
5.
Studies published in languages other than English.
Data extraction methods
A pre-designed data collection sheet in Microsoft Excel was utilized by two independent reviewers to extract data. The extracted data included demographic information such as the first authors’ surnames, study year, design and location, the mean age of patients, number of participants, and mean follow-up period. Other information collected included whether patellar resurfacing was performed, the type of prosthesis used, range of motion, clinical and functional knee society scores, stair climbing scores, survivorship, overall complication rates, and radiostereographic analysis.
Qualitative assessment (risk of bias)
Two authors assessed the methodological quality of the included studies using the Newcastle–Ottawa tool, which comprises of three key domains; patient selection, comparability, and outcomes [12]. A higher overall score indicates a lower risk of bias; a score of 5 or less (out of 9) corresponds to a high risk of bias.
Quantitative analysis
The meta-analysis was conducted using RevMan V.5.0.18.33 (The Cochrane Collaboration, Copenhagen, Denmark). Continuous variables were presented as mean and standard deviation, or standardized using validated formulas [13] when presented as range, confidence interval, or first and third interquartile. Studies that could not be standardized were excluded [14]. For four studies with graph data, the Digitalizer application was used. Dichotomous variables were analyzed using Relative risk (RR) with 95% CI. Heterogeneity was measured using I2, and results were considered statistically significant at p < 0.05.
Results
Study selection
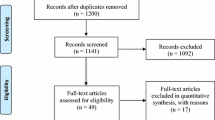
Searching the databases yielded 286 articles, and after removing 95 duplicates, 191 records were screened by title and abstracts, of which 169 were excluded. A total of 22 papers were eligible for a full-text review. As a result, 14 studies met the eligibility criteria and were included in the qualitative and quantitative synthesis. The PRISMA flowchart is displayed in Fig. 1.
Study characteristics
A total of 14 RCTs investigating the impact of all-polyethylene and metal-backed tibial components on TKR were included (Table 1). The included studies were published during the period from 2000 to 2019. The studies included in the meta-analysis recorded a total of 1367 TKA procedures, of which 686 patients received an all-polyethylene tibial tray, and the remaining 681 received a metal-backed tibial tray. All included RCTs utilized a single brand and design of prosthesis and randomized patients based on the type of tibial implant within the same brand. The randomized groups were well-matched in terms of age and gender. Follow-up duration varied among the studies, ranging from 1 to 10 years, resulting in some heterogeneity. We specifically analyzed studies with comparable follow-up durations, categorizing them as short-term (1–5 years), long-term (6–10 years), and final follow-up (1–10 years). None of the studies reported the use of vitamin E-treated polyethylene, probably because it was not well established at the time of the included studies. However, only two studies, Hamersveld et al. [15] and Bettinson et al. [16], mentioned the use of Ultra-high-molecular-weight polyethylene (Fig. 2).
Quality assessment
The scores of all 14 studies ranged from 7 to 9, indicating a low overall risk of bias. [12]. A summary of the qualitative assessment, according to the Newcastle–Ottawa scale, is shown in Table 2.
Functional knee society score
Ten of the RTC studies [3, 15, 17,18,19,20,21,22,23,24] reported the functional knee society score, and the results were analyzed at the final assessment. The final assessment ranged from 1 to 3 years in seven studies, 5 years in one study, and 10 years in two studies. None of the papers reported a statistically significant difference between APT and MBT tibias, and our analysis confirmed this. Figure 3 displays the forest plot of the functional knee society score, which shows no statistical difference between the two tibial designs (OR 1.38; 95% CI − 0.47–3.23, p value 0.14) and high heterogeneity across the results (I2 = 84%).
Clinical knee society score
Ten RCTs [3, 15, 17,18,19,20,21,22,23,24] reported the clinical or pain knee society score, and none of them reported a statistically significant difference at the final follow-up, which ranged from 1 to 10 years. This was also confirmed by the meta-analysis (OR − 0.20; 95% CI − 1.46–1.05, p value 0.75). Figure 4 presents the forest plot of the pooled data from the included papers, and it shows no statistically significant difference between the two groups (p = 0.75). The heterogeneity was low, with an I2 value of 25%.
Knee range of motion
At the final follow-up, eight studies [3, 17,18,19, 21,22,23,24] reported the degree of knee flexion among APT and MBT designs. The fixed effect of the meta-analysis revealed no statistically significant difference between the two groups, as demonstrated in Fig. 5 (OR − 0.57; 95% CI − 2.00–0.85, p value 0.43).
Stairs climbing score
The stairs climbing score was reported in both Pagnano et al. [24] and Kalisvaart et al. [18], with a total of 311 patients randomized between the two tibial designs at the final follow-ups of 1 year and 5 years, respectively. According to our fixed model analysis, the all-polyethylene tibia was statistically superior in the stairs climbing score at the final follow-up of the included studies. This is shown in Fig. 6 (OR − 2.07; 95% CI − 3.27 to − 0.87; p value 0.0007).
Radiostereographic analysis (RSA)
Radiostereographic analysis was performed in 7 studies [3, 15, 19, 21, 25, 26] of the analyzed RCTs, with all of these papers reporting RSA at 2 years. None of these studies showed any significant implant migration differences between APT and MBT designs. However, our fixed model analyses revealed that MBT knees were significantly superior in terms of anterior–posterior rotation (Fig. 7) and internal–external rotation migration (Fig. 8) at 2 years, as shown in the data pooled from 6 studies [3, 15, 19, 21, 25] with (OR − 0.09; 95% CI − 0.16 to − 0.02; p value 0.02) and (OR − 0.11; 95% CI − 0.16 to − 0.06, p value < 0.0001), respectively. Moreover, MBT knees were also superior in terms of varus–valgus malalignment (Fig. 9) at 2 years, as shown in the data pooled from 7 studies [3, 15, 19, 21, 25, 26] (OR − 0.10; 95% CI − 0.14–0.06, p value < 0.00001). Additionally, all-polyethylene knees were significantly higher rates in terms of maximal implant subsidence at 2 years (OR 0.11; 95% CI 0.06–0.15, p value < 0.00001), as shown in Fig. 10 [3, 19, 25, 26]. Although APT appeared to be more stable statistically, it is unknown whether these results are clinically significant.
Complication rate
Seven RCTs [3, 18, 19, 21,22,23,24] reported on complication events at their final follow-ups, which ranged from 1 to 10 years. While more events occurred in the MBT group, the overall fixed model analysis showed no significant difference (OR 0.83; 95% CI 0.5–1.39, p value 0.48). Figure 11 displays the forest plot of the pooled data. Pooled complications were mainly infection, aseptic loosening and knee stiffness.
Survivorship
Survivorship percentages were reported in the included studies. Data on two endpoints were pooled, with two studies [18, 23] reporting implant survivorship at 5 years and three others [16, 17, 22] reporting at 10 years. At 5 years, the all-polyethylene tibia design showed a lower revision rate and appeared to be superior compared to the metal-backed counterpart (OR 0.27; 95% CI 0.10–0.75; p value 0.01) (Fig. 12). However, there was no significant difference between the survivorship of both designs at 10 years (OR 0.92; 95% CI 0.53–1.60; p value 0.78) (Fig. 13). It was not possible to pool the type of polyethylene used in the studies or whether they were treated with vitamin E or not. Also, no study has reported results beyond 10 years.
Discussion
Despite the relative lack of popularity compared to metal-backed counterparts in current practice, the literature suggests that all-polyethylene tibial trays yield comparable results. The most significant findings of this meta-analysis were that the all-polyethylene tibial tray was associated with better outcomes, including higher scores on stair climbing, short-term survivorship, and maximal implant subsidence. Furthermore, this study found that all of the randomized trials included in our analysis showed comparable results in terms of overall complication rates, long-term survivorship, range of motion and knee society scores.
The selection of tibial components for total knee arthroplasty has been a topic of debate throughout the development of the procedure. While surgeons from various backgrounds may claim the effectiveness of one implant over another, randomized trials have failed to demonstrate the superiority of any particular implant [14, 27,28,29]. For example, studies have shown that fixed-bearing versus mobile-bearing tibias, cruciate-retaining versus posterior-stabilized, and metal-backed versus all-polyethylene tibias all yield similar outcomes [30].
Over the past decade, several meta-analyses have been conducted to compare the two tibial designs [31,32,33,34,35,36]. However, apart from the study by Tao Cheng et al. in 2011, none of the other studies were classified as Level I evidence [35]. While the results of most studies showed comparable outcomes for both tibial designs, authors often cautioned readers to interpret their conclusions carefully due to publication bias and poor methodological quality of the included studies. Cheng et al. [35] published the only Level I meta-analysis, which included data from nine randomized controlled trials (RCTs) and only pooled complication rates using a fixed model. While the authors conducted a systematic review of functional knee scores, quality of life scores, range of motion, and implant position for each RCT, none of these data were systematically analyzed in fixed or random effect models. In contrast, our study included 14 RCTs, and all of our results were presented in a systematic analysis pattern, where studies with similar outcomes were pooled together and analyzed.
When considering the similar clinical performance of both tibial designs, cost becomes an important factor. While some studies have reported cost savings of up to 30% with the all-polyethylene tibia [3, 4], others have claimed the opposite [14, 32]. Longo et al. [32], in their Level III meta-analysis in 2016, found that metal-backed and all-polyethylene tibias had comparable clinical outcomes and range of motion. However, they also found that complications and revision rates were higher with the all-polyethylene design, making metal-backed tibias more cost-effective. Despite analyzing 32 studies, there was significant heterogeneity among the included studies in the later meta-analysis [32], and there were inadequate reports on the complications. In addition to the issues with heterogeneity and inadequate reporting of complications in the Longo et al. meta-analysis [32], some of the studies included were reporting on older versions of polyethylene that have since lost popularity due to wear and weaker mechanical characteristics. This may explain their reporting of a higher complication rate with all-polyethylene tibias. In contrast, our study found fewer complications and a lower early revision rate when more contemporary polyethylene components were studied. This could be attributed to the recent use of vitamin E-treated polyethylene, which has been shown to have theoretical superiority in vitro, although not necessarily in vivo [37, 38].
Our study also included radiostereographic analysis (RSA) as a means of comparing the two tibial designs. Interestingly, we found that the metal-backed design was significantly more radiographically stable in anterior–posterior, varus–valgus, and internal–external rotations at the 2-year follow-up compared to all-polyethylene tibias. However, caution should be exercised when interpreting these results due to significant heterogeneity among the studies. Moreover, the metal-backed design had significantly less maximal implant subsidence. This is consistent with the findings of Nouta et al. [34], who conducted a systematic review in 2012 and similarly reported better implant fixation in all-polyethylene tibias with lower maximum total point motion compared to the metal-backed counterpart.
Our study's main advantage is its inclusion of high-quality articles in the meta-analysis, making it, to our knowledge, the only level 1 evidence meta-analysis on the subject. We analyzed all 14 RCTs comparing the two tibial design concepts. However, the heterogeneity of the studies limited the sample size we could analyze, and some studies reported outcome measures that others did not. We also encountered difficulties reporting outcomes at the last follow-up, as the studies had different follow-up periods, so we reported our results at the final follow-up assessment instead of a mean time with a wide range of final surveillance.
Conclusion
While this meta-analysis suggests that all-polyethylene tibial components in total knee arthroplasty may offer advantages over metal-backed components in terms of five-year survivorship, and stairs climbing score, this finding should be considered in the context of potential confounding factors. Nonetheless, based on the results, the all-polyethylene implant should be considered a viable choice for primary knee replacement.
Availability of data, material and code
Not applicable as this is a review article. However, happy to provide access to any statistical data (coding) upon request.
References
Pomeroy DL, Schaper LA, Badenhausen WE (2000) Results of all-polyethylene tibial components as a cost-saving technique. Clin Orthop Relat Res 380:140–143
Yassin M, Garti A, Weissbrot M, Ashkenazi U, Khatib M, Robinson D (2015) All-polyethylene tibial components are not inferior to metal-backed tibial components in long-term follow-up of knee arthroplasties. Eur J Orthop Surg Traumatol 25(6):1087–1091
Norgren B, Dalén T, Nilsson KG (2004) All-poly tibial component better than metal-backed: a randomized RSA study. Knee 11(3):189–196
Mohan V, Inacio MC, Namba RS, Sheth D, Paxton EW (2013) Monoblock all-polyethylene tibial components have a lower risk of early revision than metal-backed modular components. Acta Orthop 84(6):530–536
Rand JA (1993) Comparison of metal-backed and all-polyethylene tibial components in cruciate condylar total knee arthroplasty. J Arthroplasty 8(3):307–313
Gioe TJ, Maheshwari AV (2010) The all-polyethylene tibial component in primary total knee arthroplasty. J Bone Joint Surg Am 92(2):478–487
Apel DM, Tozzi JM, Dorr LD (1991) Clinical comparison of all-polyethylene and metal-backed tibial components in total knee arthroplasty. Clin Orthop Relat Res 273:243–252
Brihault J, Navacchia A, Pianigiani S, Labey L, De Corte R, Pascale V, Innocenti B (2016) All-polyethylene tibial components generate higher stress and micromotions than metal-backed tibial components in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24(8):2550–2559
Waddell DD, Sedacki K, Yang Y, Fitch DA (2016) Early radiographic and functional outcomes of a cancellous titanium-coated tibial component for total knee arthroplasty. Musculoskelet Surg 100(1):71–74
Enea D, Cigna V, Sgolacchia C, Tozzi L, Verdenelli A, Gigante A (2015) Retained versus resected posterior cruciate ligament in mobile-bearing total knee replacement: a retrospective, clinical and functional assessment. Musculoskelet Surg 99(2):149–154
Moher D, Liberati A, Tetzlaff J, Altman DG (2010) The PRISMA group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2013) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in metaanalyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 29 Jan 2023
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Murray DW, MacLennan GS, Breeman S, Dakin HA, Johnston L, Campbell MK, Gray AM, Fiddian N, Fitzpatrick R, Morris RW, Grant AM, KAT group (2014) A randomised controlled trial of the clinical effectiveness and cost-effectiveness of different knee prostheses the Knee Arthroplasty Trial (KAT). Health Technol Assess 18(19):1–235 (vii–viii)
Van Hamersveld KT, Marang-Van De Mheen PJ, Nelissen RGHH, Toksvig-Larsen S (2018) Migration of all-polyethylene compared with metal-backed tibial components in cemented total knee arthroplasty. Acta Orthop 4:412–417
Bettinson KA, Pinder IM, Moran CG, Weir DJ, Lingard EA (2009) All-polyethylene compared with metal-backed tibial components in total knee arthroplasty at ten years: a prospective, randomized controlled trial. J Bone Joint Surg Am 91(7):1587–1594
Abdel MP, Tibbo ME, Stuart MJ, Trousdale RT, Hanssen AD, Pagnano MW (2018) A randomized controlled trial of fixed—versus mobile-bearing total knee arthroplasty: a follow-up at a mean of ten years. Bone Joint J 100B(7):925–929
Kalisvaart MM, Pagnano MW, Trousdale RT, Stuart MJ, Hanssen AD (2012) Randomized clinical trial of rotating-platform and fixed-bearing total knee arthroplasty: no clinically detectable differences at five years. J Bone Joint Surg Am 94(6):481–489
Adalberth G, Nilsson KG, Byström S, Kolstad K, Milbrink J (2001) All-polyethylene versus metal-backed and stemmed tibial components in cemented total knee arthroplasty: a prospective, randomised RSA study. J Bone Joint Surg Br 83(6):825–831
Hasan S, Marang-Van De Mheen PJ, Kaptein BL, Nelissen RGHH, Toksvig-Larsen S (2019) All-polyethylene versus metal-backed posterior stabilized total knee arthroplasty: similar 2-year results of a randomized radiostereometric analysis study. Acta Orthop 90(6):590–595
Adalberth G, Nilsson KG, Byström S, Kolstad K, Milbrink J (2000) Low-conforming all-polyethylene tibial component not inferior to metal-backed component in cemented total knee arthroplasty: prospective, randomized radiostereometric analysis study of the AGC total knee prosthesis. J Arthroplasty 15(6):783–792
Gioe TJ, Stroemer ES, Santos ER (2007) All-polyethylene and metal-backed tibias have similar outcomes at 10 years: a randomized level I [corrected] evidence study. Clin Orthop Relat Res 455:212–218
Gioe TJ, Bowman KR (2000) A randomized comparison of all-polyethylene and metal-backed tibial components. Clin Orthop Relat Res 380:108–115
Pagnano MW, Trousdale RT, Stuart MJ, Hanssen AD, Jacofsky DJ (2004) Rotating platform knees did not improve patellar tracking: a prospective, randomized study of 240 primary total knee arthroplasties. Clin Orthop Relat Res 428:221–227
Hyldahl H, Regnér L, Carlsson L, Kärrholm J, Weidenhielm L (2005) All-polyethylene vs. metal-backed tibial component in total knee arthroplasty—a randomized RSA study comparing early fixation of horizontally and completely cemented tibial components: part 1. Horizontally cemented components AP: better fixated than MB. Acta Orthop 76(6):769–777
Muller SD, Deehan DJ, Holland JP, Outterside SE, Kirk LM, Gregg PJ, McCaskie AW (2006) Should we reconsider all-polyethylene tibial implants in total knee replacement? J Bone Joint Surg Br 88(12):1596–1602
KAT Trial Group, Johnston L, MacLennan G, McCormack K, Ramsay C, Walker A (2009) The Knee Arthroplasty Trial (KAT) design features, baseline characteristics, and two-year functional outcomes after alternative approaches to knee replacement. J Bone Joint Surg Am 91(1):134–141
Gioe TJ, Glynn J, Sembrano J, Suthers K, Santos ER, Singh J (2009) Mobile and fixed-bearing (all-polyethylene tibial component) total knee arthroplasty designs: a prospective randomized trial. J Bone Joint Surg Am 91(9):2104–2112
Robinson RP, Green TM (2011) Eleven-year implant survival rates of the all-polyethylene and metal-backed modular Optetrak posterior stabilized knee in bilateral simultaneous cases. J Arthroplasty 26(8):1165–1169
Hantouly AT, Ahmed AF, Alzobi O, Toubasi A, Salameh M, Elmhiregh A, Hameed S, Ahmed GO, Alvand A, Al Dosari MAA (2022) Mobile-bearing versus fixed-bearing total knee arthroplasty: a meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol 32(3):481–495
Costa GG, Lo PM, Grassi A, Agrò G, Cialdella S, Mosca M, Caravelli S, Zaffagnini S (2020) Metal-backed tibial components do not reduce risk of early aseptic loosening in unicompartmental knee arthroplasty: a systematic review and meta-analysis. J Knee Surg 33(2):180–189
Longo UG, Ciuffreda M, D’Andrea V, Mannering N, Locher J, Denaro V (2017) All-polyethylene versus metal-backed tibial component in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25(11):3620–3636
Voss B, El-Othmani MM, Schnur AK, Botchway A, Mihalko WM, Saleh KJ (2016) A meta-analysis comparing all-polyethylene tibial component to metal-backed tibial component in total knee arthroplasty: assessing survivorship and functional outcomes. J Arthroplasty 31(11):2628–2636
Nouta KA, Verra WC, Pijls BG, Schoones JW, Nelissen RG (2012) All-polyethylene tibial components are equal to metal-backed components: systematic review and meta-regression. Clin Orthop Relat Res 470(12):3549–3559
Cheng T, Zhang G, Zhang X (2011) Metal-backed versus all-polyethylene tibial components in primary total knee arthroplasty. Acta Orthop 82(5):589–595
Cheng T, Pan X, Liu T, Zhang X (2012) Tibial component designs in primary total knee arthroplasty: should we reconsider all-polyethylene component? Knee Surg Sports Traumatol Arthrosc 20(8):1438–1449
Takemura S, Minoda Y, Sugama R, Ohta Y, Nakamura S, Ueyama H, Nakamura H (2019) Comparison of a vitamin E-infused highly crosslinked polyethylene insert and a conventional polyethylene insert for primary total knee arthroplasty at two years postoperatively. Bone Joint J 101-B(5):559–564
Busch A, Jäger M, VITAS group, Wegner A, Haversath M (2020) Vitamin E-blended versus conventional polyethylene liners in prostheses: prospective, randomized trial with 3-year follow-up. Orthopade 49(12):1077–1085
Funding
Open Access funding provided by the Qatar National Library.
Author information
Authors and Affiliations
Contributions
AE: Data collection, statistical analysis, manuscript writing. YA: Data collection, statistical analysis. OA: Data collection, manuscript review and submission. BZ: Data collection, MA: manuscript writing. BM: Data reviewing.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This is a review article. No ethical approval is required.
Consent to participate
Not applicable as this is a review article.
Consent for publication
Not applicable as this is a review article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elmhiregh, A., Abuodeh, Y., Alzobi, O. et al. All-polyethylene versus metal-backed tibial components in total knee arthroplasty: a meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol 33, 3611–3622 (2023). https://doi.org/10.1007/s00590-023-03594-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03594-y