Abstract
Purpose
Spinal surgeries are a very painful procedure. New regional techniques for postoperative pain management are being considered. The present study aimed to evaluate the hypothesis that the ultrasound-guided erector spinae plane (ESP) block would lead to lower opioid consumption compared to the thoracolumbar interfascial plane (TLIP) block after lumbar disk surgery. The study's primary objective was to compare postoperative total opioid consumption, and the secondary objective was to assess postoperative pain scores.
Methods
Sixty-eight patients who underwent elective lumbar disk surgery were randomly assigned to either the ESP block group or the TLIP block group. The current pain status of the patients in both the ESP and TLIP block groups was assessed using the Numerical Rating Scale (NRS) at specific time intervals (30 min, 1, 6, 12 and 24 h) during the postoperative period. The number of times patients administered a bolus dose of patient-controlled analgesia, (PCA) within the first 24 h was recorded.
Results
In the ESP group, the total opioid consumption in terms of morphine equivalents was found to be significantly lower (ESP group: 7.7 ± 7.0; TLIP group: 13.0 ± 10.1; p < 0.05). The NRS scores were similar between the groups at 30 min, 1, 6, and 12 h, but at 24 h, they were significantly lower in the ESP group. Moreover, the groups had no significant difference regarding observed side effects.
Conclusion
This study demonstrated the analgesic efficacy of both techniques, revealing that the ESP block provides more effective analgesia in patients undergoing lumbar disk surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal surgery patients generally suffer from chronic pain in the preoperative period and are exposed to widespread and severe acute pain in the postoperative period. Providing effective postoperative analgesia in spinal surgery patients is essential for the patient's comfort and preventing the negative effects of pain on the body systems, allowing early mobilization, reducing the duration of hospitalization, and minimizing the risk of developing postoperative chronic pain syndromes.
In spinal surgery, interfascial plane blocks have started to be preferred as an effective and safe choice for postoperative multimodal pain management due to their ability to provide long-lasting analgesia, reduce opioid consumption, and cause fewer motor blocks. The erector spinae plane (ESP) block was first documented in 2016 for treating thoracic neuropathic pain and was subsequently reported to provide postoperative analgesic effectiveness [1, 2]. The analgesic mechanism of the ESP block is believed to involve the diffusion of injected local anesthetics cranially and caudally, affecting the ventral and dorsal rami of the spinal nerves [3]. Incisional pain is reduced by the ESP block, which effectively blocks a large region of the anterior, lateral, and posterior thoracic and lumbar walls. The ESP block is also thought to prevent visceral autonomic pain and provide effective postoperative analgesia.
The thoracolumbar interfascial plane block (TLIP) is paraspinal. By spreading between the fascia of the multifidus and longissimus muscles at the third lumbar vertebral level, the local anesthetic used in this block which is carried out under ultrasound guidance-targets the dorsal branches of the thoracolumbar nerves. According to reports, it has been observed to offer efficacious analgesic effects with focused dermatomal coverage in the incision area in spinal surgeries [4, 5].
The present study aimed to assess and compare the analgesic efficacy of TLIP block and ESP block, both performed under ultrasound guidance, following lumbar discectomy surgery. The main objective of the study was to assess and compare postoperative amount of opioid consumed. The additional objective was to compare scores of postoperative pain.
Material and methods
The research was conducted as a double-blind, randomized, controlled trial, which received approval from the Clinical Trials Ethics Committee and registered on ClinicalTrials.gov (NCT04028154). The trial comprised patients who had given written consent over the period from January 2022 to March 2023. Accordingly, 68 patients, ranging in age from 18 to 75, with ASA I-II classification, who underwent elective one or two-level lumbar disk surgery, were enrolled. The presence of bleeding diathesis, hypersensitivity to the local anesthetics used, chronic opioid use, presence of psychiatric diseases, and infection at the injection site were determined as exclusion criteria.
Healthcare professionals assessed the patient's pain in the recovery room and the ward, who needed to be made aware of whether an ESP block or TLIP block was applied. Patients were informed about the patient-controlled analgesia (PCA) device to be used for pain management before the intervention and were instructed on using the numerical rating scale (NRS) for pain assessment. The participants were allocated into two distinct groups: ESPB and TLIPB. The randomization of patients was computer-assisted. This study was conducted following CONSORT criteria (Fig. 1).
The anesthesia technique
In each group, anesthetic induction was conducted with a dosage of 2 mg/kg of propofol, 1 μg/kg of fentanyl, and0.6 mg/kg of rocuronium. Anesthesia maintenance was achieved with a 50/50 oxygen/air mixture at 3 L/min flow rate and 2% sevoflurane. Intraoperative analgesia was provided with 0.05 mcg/kg/min of remifentanil. In order to provide postoperative analgesia, both groups received intravenous administration of 1 mg/kg of tramadol and 1 g of paracetamol, 30 min prior to the conclusion of the surgical procedure. During emergence, neuromuscular blockade was reversed with 2 mg/kg of sugammadex, and extubation was performed. Patients with a modified Aldrete score of 9 or higher in there covery room were transferred to the ward.
Ultrasound-guided ESP block
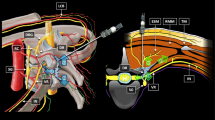
Just prior to the patients’ awakening after the surgery, an ESP block was performed on the ESPB group. The block was administered while the patients were in the prone position under ultrasound imaging guidance. A high-frequency linear ultrasound probe (10–15 MHz Logiq-e GE, USA) was used, and it was advanced sagittally to a point 3 cm lateral to the T10 spinous process. However, for patients with a BMI of 35 kg/m2and above, a curvilinear ultrasound probe (1–6 MHz Logiq-e GE, USA) was used to acquire the image. The erector spinae muscle and transverse process were visible thanks to the ultrasonography, and the needle was gently moved along the transverse process until it reached the bone (Fig. 2).
Using a test dose of 0.5–1 mL of 0.9% NaCl, hydro dissection was performed between the transverse process and the erector spinae muscle fascia following confirmation of needle placement through the craniocaudal spread. Then, a 20 mL fluid injection was made into the gap that exists between the transverse process and the erector spinal muscle. 10 mL of 0.5% bupivacaine, 5 mL of 2% lidocaine, and 5 mL of 0.9% NaCl were contained in the volume. The same procedure was then replicated on the opposite side for each patient, resulting in 40 mL of fluid being administered to each individual. It is noteworthy that all procedures were conducted under sterile conditions.
Ultrasound-guided TLIP block
The TLIP block, similar to the other group, was performed on the patients in the prone position under ultrasound guidance immediately before waking them up. The USG probe was utilized under identical experimental settings as those employed in the ESP group. The paraspinal muscles were visualized by advancing the probe laterally (Fig. 2). After identifying the multifidus, longissimus, and iliocostalis muscles, the needle's position was confirmed by injecting 0.5–1 mL of 0.9% NaCl test dose between the multifidus and longissimus muscles. Subsequently, a total volume of 20 mL, containing 10 mL of 0.5% bupivacaine, 5 mL of 2% lidocaine, and 5 mL of 0.9% NaCl, were applied to the plane between the multifidus and longissimus muscles. The same procedure was then replicated on the opposite side for each patient, resulting in 40 mL of fluid being administered to each individual. All procedures were completed under sterile conditions.
Postoperative analgesia protocol
A bilateral block of 0.25% bupivacaine, with a volume of 40 mL, was delivered to each group prior to awakening. In order to provide postoperative analgesia, each group received intravenous administration of 1 mg/kg tramadol and 1 g paracetamol, 30 min prior to the conclusion of the surgical procedure. All patients were provided with PCA devices, which administered a bolus dose of tramadol at a rate of 0.1 mg/kg, without a continuous basal infusion. Additionally, a lockout time of 20 min was established.
The patients' pain scores were assessed with an 11-point NRS that spanned from 0 to 10 (0 = no pain, 10 = worst imaginable pain). If the NRS score was 4 or higher in the recovery room, an additional 0.5 mg/kg meperidine was administered. Pain was assessed at postoperative 30 min, 1, 6, 12 and 24 h using the NRS.
During the follow-up in the ward, patients received 1 g IV paracetamol every 8 h (omitted if the patient's NRS score was below 4 and the patient did not request analgesics). If the NRS score remained 4 or higher despite paracetamol administration, additional 75 mg IM diclofenac sodium was also given. The number of bolus doses administered with PCA within the first 24 h was recorded. Patients who experienced nausea or vomiting were given 4 mg IV ondansetron.
Data collection
Both groups were assessed for demographics and surgical parameters, including age, height, weight, gender, comorbidities, ASA scores, surgical levels, and operation durations. Within 24 h of surgery, the primary outcome was the amount of opioids consumed, measured in milligrams and computed as morphine equivalent dose. The meperidine dose and approximate IV tramadol consumption over 24 h were stored in PCA's electronic memory. The 24-h cumulative morphine equivalent dose was calculated.
To determine if ESPB and TLIPB offered analgesic benefits during the initial postoperative phase, NRS scores were taken at 30, 1, 6, 12 and 24 h. Number of effective bolus administrations and postoperative paracetamol use. Side symptoms like nausea, vomiting, itching, and constipation were recorded. The initial postoperative mobilization, oral intake, hospital stay, and first-day problems were also noted.
Statistical analysis
The data were analyzed using SPSS 21.0. A similar study [6] was taken as a reference in the sample calculation using the G Power program, and the effect size calculation was made. In the sample calculation performed with the t test, the effect size was found to be 0.8. In order to reach sufficient sampling, it was planned to include 34 patients in each group with 90% power, 5% margin of error, and 0.8 effect size, with a 10% dropout rate. Parametric data were evaluated using the Student t test and nonparametric data with the chi-square test. One-way analysis of variance (ANOVA) was used to examine repeated measurements within and across groups. Data having a normal distribution were presented using the mean and standard deviation, while non-normal data were reported using the median. Statistical significance was set at p < 0.05.
Results
The study had a cohort of 71 patients. Three patients who were initially included in the trial were subsequently eliminated due to incompatibility with PCA. Ultimately, a total of 34 patients were incorporated into both the ESP and TLIP block cohorts.
After doing a thorough analysis of the demographic data, it was determined that there were no statistically significant disparities seen between the groups in relation to gender, age, weight, and BMI (p > 0.05) (Table 1). Similarly, no statistically significant variations were found between the two groups concerning surgical procedure levels, operation duration, and application duration of the blocks (p > 0.05).
The average postoperative mobilization time was 15.9 ± 4.5 h in the ESP group and 18.7 ± 2.62 h in the TLIP group, with a statistically significant difference being observed (p = 0.011). Regarding hospital stay and time to oral intake initiation, there were no statistically significant differences between the groups (p > 0.05) (Table 1).
In the postoperative recovery unit, the use of meperidine in the ESPB group was 14.6 ± 22.4 mg, and in the TLIPB, it was 27.3 ± 28.2 mg, and a statistically significant difference was found (p = 0.045) (Table 2). There was no statistically significant difference between the groups using diclofenac sodium as rescue analgesia and the number of PCA button presses for pain relief.
The amount of tramadol consumed postoperatively was 56.2 ± 54.4 mg in the ESPB group and 80.4 ± 55.3 mg in the TLIPB group. A statistically significant difference was noted between the two groups. The total opioid consumption in morphine equivalent dose was assessed, revealing a mean value of 7.7 ± 7.0 mg in the ESPB group and 13.0 ± 10.1 mg in the TLIPB group. A statistically significant difference was seen between the two groups (p = 0.015) (Table 2).
The postoperative NRS scores were assessed within the initial 24-h period. There was no statistically significant disparity observed between the two groups in relation to the NRS scores recorded at the time intervals of 30 min, 1 h, 6 h, and 12 h (p = 0.236, p = 0.065, p = 0.710, p = 0.114, respectively). However, the NRS scores at 24 h were statistically significant between the groups (p = 0.000) (Fig. 3, Table 3).
During the postoperative 24-h period, there were no statistically significant differences between the groups regarding the presence of nausea, vomiting, itching, constipation, and the need for antiemetic drugs (p > 0.05) (Table 4). No instances of complications, such as procedure-related pneumothorax and infection, were detected in either of the groups. Following the surgical procedure, there was no observed presence of motor block in either of the groups.
Discussion
The present study demonstrates that the implementation of ESP block in spinal surgery resulted in a notable decrease in the need for postoperative analgesics, surpassing the effectiveness of TLIP block. There were no statistically significant variations in NRS scores seen between the groups at the 30-min, 1-h, 6-h, and 12-h time points. However, at the 24-h mark, the ESP group exhibited considerably lower scores in a statistically significant manner. The period of postoperative mobilization was found to be significantly shorter in the ESP group, although no statistically significant difference was observed in the duration of hospital stay. There were no identified problems associated with the surgeries.
Although the analgesic mechanism of ESPB has not been elucidated, it is believed that the applied local anesthetic affects the dorsal and ventral branches of spinal nerves, providing a multi-dermatomal sensory block [3, 7]. ESPB can provide visceral and somatic analgesia through the paravertebral and epidural spread. ESPB has been shown to offer adequate analgesic treatment for a variety of lumbar spine surgical procedures in randomized trials and case reports [8,9,10,11]. The classical methodology proposed by Hand et al. [1] involves the administration of a local anesthetic solution into the interfascial region located between the multifidus and longissimus muscles at the third lumbar vertebra level. The mechanism of TLIPB targets the dorsal branches of the lumbar nerves. After lumbar spine surgery, several studies have demonstrated the efficacy of analgesic management [4, 12,13,14].
There needs to be more studies in the literature comparing these two techniques. Çiftçi et al. compared ESP and TLIP blocks in a patient group undergoing single-level discectomies with a control group. They reported that both blocks provided significantly good analgesia, but unlike our study, they found no superiority of the ESP or TLIP block over each other [15]. We believe that the better analgesia, earlier mobilization, and lower pain scores at 24 h in our study may be explained by ESPB being applied to deeper muscle groups, resulting in delayed clearance from the surgical area [4, 14], its wide craniocaudal spread capacity, ventral branch blockade, and epidural spread [8].
Kumar et al. [16] shared similar results to our study with lower pain scores and opioid consumption in the ESP block compared to TLIP block in their comparison of ESP and TLIP blocks in a patient group undergoing discectomy surgery during their 48-h observations in the ESP group. The use of 0.2% ropivacaine in the blocks in their study differs from our method, which constitutes a limitation in our comparison. On the other hand, Wang et al. [17] compared TLIP and ESP blocks in patient groups, including fusion surgeries, and unlike us, they found ESP block superior in terms of NRS score and opioid consumption at 12 h. Our perception that single-level TLIP application in long-segment surgeries may cause insufficient analgesia contributed to the superiority of ESP block in this study. Recently, Tantri et al. [18] reported in their study, which included longer segment stabilization surgeries compared to Wang et al. that ESP and TLIP blocks had no superiority in pain scores and opioid consumption. Unlike other studies, the application of ESP block at the L3 level may have limited the analgesic area.
One primary constraint of our study pertains to the limited sample size. Another limitation is that the applied blocks were performed immediately before awakening the patients, so they could not evaluate the sensory block area. Another limitation is that our mobilization time is longer than expected in microdiscectomy cases, depending on the routines in our clinical practice. Finally, since fusion surgeries are primarily performed in long segments, a single-level intervention would not be sufficient in these cases and only included patients undergoing discectomy in the study. Therefore, the study cannot provide information about the effectiveness in patients undergoing instrumentation. Comparative studies are needed to assess effectiveness in this group of patients.
Conclusion
Based on our findings and literature data, we concluded that the ESP block was more advantageous, although postoperative analgesic efficacy was achieved for both blocks. However, further support from more clinical randomized studies is necessary.
References
Hand WR, Taylor JM, Harvey NR, Epperson TI et al (2015) Thoracolumbar interfascial plane (TLIP) block: a pilot study in volunteers. Can J Anaesth (Journal Canadien d’Anesthesie) 62(11):1196–1200. https://doi.org/10.1007/s12630-015-0431-y
Almeida CR, Oliveira AR, Cunha P (2019) Continuous bilateral erector of spine plane block at T8 for extensive lumbar spine fusion surgery: case report. Pain Pract Off J World Inst Pain 19(5):536–540. https://doi.org/10.1111/papr.12774
Yang HM, Choi YJ, Kwon HJ et al (2018) Comparison of injectate spread and nerve involvement between retrolaminar and erector spinae plane blocks in the thoracic region: a cadaveric study. Anaesthesia 73(10):1244–1250. https://doi.org/10.1111/anae.14408
Li C, Jia J, Qin Z, Tang Z (2018) The use of ultrasound-guided modified thoracolumbar interfascial plane (TLIP) block for multi-level lumbar spinal surgery. J Clin Anesth 46:49–51. https://doi.org/10.1016/j.jclinane.2018.01.018
Hamilton DL (2021) Does thoracolumbar interfascial plane block provide more focused analgesia than erector spinae plane block in lumbar spine surgery? J Neurosurg Anesthesiol 33(1):92–93. https://doi.org/10.1097/ANA.0000000000000643
Tulgar S, Kose HC, Selvi O et al (2018) Comparison of ultrasound-guided lumbar erector spinae plane block and transmuscular quadratus lumborum block for postoperative analgesia in hip and proximal femur surgery: a prospective randomized feasibility study. Anesth Essays Res 12(4):825–831. https://doi.org/10.4103/aer.AER_142_18
Greenhalgh K, Womack J, Marcangelo S (2019) Injectate spread in erector spinae plane block. Anaesthesia 74(1):126–127. https://doi.org/10.1111/anae.14523
Yayik AM, Cesur S, Ozturk F et al (2019) Postoperative analgesic efficacy of the ultrasound-guided erector spinae plane block in patients undergoing lumbar spinal decompression surgery: a randomized controlled study. World Neurosurg 126:e779–e785. https://doi.org/10.1016/j.wneu.2019.02.149
Singh S, Choudhary NK, Lalin D, Verma VK (2020) Bilateral ultrasound-guided erector spinae plane block for postoperative analgesia in lumbar spine surgery: a randomized control trial. J Neurosurg Anesthesiol 32(4):330–334. https://doi.org/10.1097/ANA.0000000000000603
Asar S, Sarı S, Altinpulluk EY et al (2022) Efficacy of erector spinae plane block on postoperative pain in patients undergoing lumbar spine surgery. Eur Spine J 31:197–204. https://doi.org/10.1007/s00586-021-07056-z
Melvin JP, Schrot RJ, Chu GM, Chin KJ (2018) Low thoracic erector spinae plane block for perioperative analgesia in lumbosacral spine surgery: a case series. Bloc du plan des muscles érecteurs du rachis thoracique bas pour analgésie périopératoire dans la chirurgie du rachis lombosacré: unesérie de cas. Can J Anaesth (Journal Canadien d’Anesthesie) 65(9):1057–1065. https://doi.org/10.1007/s12630-018-1145-8
Ahiskalioglu A, Yayik AM, Doymus O et al (2018) Efficacy of ultrasound-guided modified thoracolumbar interfascial plane block for postoperative analgesia after spinal surgery: a randomized-controlled trial. Can J Anaesth (Journal canadien d’anesthesie) 65(5):603–604. https://doi.org/10.1007/s12630-018-1051-0
Ekinci M, Ciftci B, Atalay YO (2019) Ultrasound-guided modified thoracolumbar interfascial plane block is effective for pain management following multi-level lumbar spinal fusion surgery. Ain-Shams J Anesthesiol 11(1):3. https://doi.org/10.1186/s42077-019-0046-6
Ahiskalioglu A, Yayik AM, Celik EC et al (2019) Ultrasound guided modified thoracolumbar interfascial plane block for low back pain management. J Clin Anesth 54:138–139. https://doi.org/10.1016/j.jclinane.2018.11.010
Ciftci B, Ekinci M, Celik EC et al (2020) Ultrasound-guided erector spinae plane block versus modified-thoracolumbar interfascial plane block for lumbar discectomy surgery: a randomized, controlled study. World Neurosurg 144:e849–e855. https://doi.org/10.1016/j.wneu.2020.09.077
Kumar A, Sinha C, Kumar A et al (2023) Modified thoracolumbar interfascial plane block versus erector spinae plane block in patients undergoing spine surgeries: a randomized controlled trial. J Neurosurg Anesthesiol. https://doi.org/10.1097/ANA.0000000000000900
Wang L, Wu Y, Dou L et al (2021) Comparison of two ultrasound-guided plane blocks for pain and postoperative opioid requirement in lumbar spine fusion surgery: a prospective, randomized, and controlled clinical trial. Pain Ther 10(2):1331–1341. https://doi.org/10.1007/s40122-021-00295-4
Tantri AR, Rahmi R, Marsaban AHM et al (2023) Comparison of postoperative IL-6 and IL-10 levels following erector spinae plane block (ESPB) and classical thoracolumbar interfascial plane (TLIP) block in a posterior lumbar decompression and stabilization procedure: a randomized controlled trial. BMC Anesthesiol 23(1):13. https://doi.org/10.1186/s12871-023-01973-w
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dilsiz, P., Sari, S., Tan, K.B. et al. A comparison of the effects of thoracolumbar interfascial plane (TLIP) block and erector spinae plane (ESP) block in postoperative acute pain in spinal surgery. Eur Spine J 33, 1129–1136 (2024). https://doi.org/10.1007/s00586-023-08097-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-08097-2