Abstract
Purpose
We aimed to demonstrate non-inferiority in terms of functional outcomes in patients with lumbar spinal stenosis who underwent full-endoscopic decompression compared with tubular-based microscopic decompression.
Methods
This prospective, randomized controlled, non-inferiority trial included 60 patients with single-level lumbar spinal stenosis who required decompression surgery. The patients were randomly assigned in a 1:1 ratio to the full-endoscopic group (FE group) or the tubular-based microscopic group (TM group). Based on intention-to-treat analysis, the primary outcome was the Oswestry Disability Index score at 24 months postoperative. The secondary outcomes included the visual analog scale (VAS) score for back and leg pain, European Quality of Life-5 Dimensions (EQ-5D) score, walking time, and patient satisfaction rate according to the modified MacNab criteria. Surgery-related outcomes were also analyzed.
Results
Of the total patients, 92% (n = 55) completed a 24-month follow-up. The primary outcomes were comparable between the two groups (p = 0.748). However, the FE group showed a statistically significant improvement in the mean VAS score for back pain at day 1 and at 6, 12, and 24 months after surgery (p < 0.05). No significant difference was observed in the VAS score for leg pain, EQ-5D score, or walking time (p > 0.05). Regarding the modified MacNab criteria, 86.7% of patients in the FE group and 83.3% in the TM group had excellent or good results at 24 months after surgery (p = 0.261). Despite the similar results in surgery-related outcomes, including operative time, radiation exposure, revision rate, and complication rate, between the two groups (p > 0.05), less blood loss and shorter length of hospital stay were observed in the FE group (p ≤ 0.001 and 0.011, respectively).
Conclusion
This study suggests that full-endoscopic decompression is an alternative treatment for patients with lumbar spinal stenosis because it provides non-inferior clinical efficacy and safety compared with tubular-based microscopic surgery. In addition, it offers advantages in terms of less invasive surgery.
Trial registration number (TRN): TCTR20191217001.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lumbar spinal stenosis is a degenerative spinal disease caused by intervertebral disc degeneration, thickening of ligamentum flavum, hypertrophy of facet joints, and osteophyte formation, resulting in a narrowing of the spinal canal and nerve root compression [1, 2]. The clinical presentations include intermittent neurogenic claudication, low back pain, buttock pain, radicular pain down to the thigh and leg, and neurological deficits [3]. Disease progression can lead to functional disabilities and worsening quality of life [4].
Surgical treatment is considered in patients with severe intractable pain, progressive neurological deficits, bowel and bladder dysfunction, reduced quality of life, and failure of conservative treatments [5]. Conventional laminectomy has been widely performed in patients with lumbar spinal stenosis. Conventional laminectomy causes extensive damage to the posterior spinal structures such as the paraspinal muscle, ligament, and bone, which can lead to postoperative low back pain, iatrogenic segmental instability, and spondylolisthesis, and various decompression techniques of minimally invasive spinal surgery (MISS) using microscopes and endoscopes have been introduced to overcome these problems [6,7,8,9,10]. These techniques also reduce the size of the incision, minimize soft tissue damage, reduce perioperative blood loss, decrease early postoperative pain and analgesic requirements, promote early ambulation, and shorten the length of hospital stays [11,12,13,14].
The microscopic technique is a standard surgical procedure for decompression surgery of lumbar spinal stenosis [15, 16]. Previous studies have reported satisfactory outcomes [11, 17, 18]. With a tubular retractor system, paraspinal muscle damage was reduced even more during microsurgery [19, 20]. Recently, a full-endoscopic technique using an interlaminar approach has been developed for lumbar discectomy, foraminotomy, and decompression [21]. This technique has shown benefits in terms of excellent magnification, illumination, and visualization during surgery. Favorable outcomes have been observed in patients with lumbar spinal stenosis treated by a full-endoscopic technique [22,23,24,25], but evidence showing the benefit of full-endoscopic decompression compared to tubular-based microscopic decompression is still weak. Therefore, a randomized controlled trial is required.
The objective of this prospective randomized controlled study was to compare the functional outcomes between the full-endoscopic decompression technique and tubular-based microscopic decompression technique in patients with single-level lumbar spinal stenosis.
Methods
Study design
This parallel, prospective, randomized controlled study was conducted at our institute. We designed this study as a non-inferiority trial with an endpoint of 24 months. Approval was obtained from the institutional review board before study initiation. This study was registered in the Clinical Trials Registry (Number). A CONSORT 2010 guideline with an extension of the non-inferiority trial was followed [26]. All patients diagnosed with degenerative lumbar spinal stenosis from December 2019 to October 2020 were enrolled in our study. All participants provided informed consent before data collection.
Participant population
Patients with the following criteria were included: age from 40 to 80 years, symptoms of intermittent neurogenic claudication and/or radiculopathy, unresponsiveness to conservative treatment including physical therapy and epidural steroid injection for at least 3 months, single-level stenosis at the central and/or lateral recess area, and clinical symptoms correlated with magnetic resonance imaging (MRI). The exclusion criteria were presence of foraminal stenosis in the level below, degenerative spondylolisthesis (Meyerding grade > 1), presence of radiographic instability, prior spinal surgery, cauda equina syndrome, concomitant with other spinal abnormalities (e.g., infection, trauma, tumor), and patients who were not capable of answering questionnaires.
Randomization and follow-up
All patients were randomly assigned to two groups at a 1:1 ratio: the full-endoscopic group (FE group) and the tubular-based microscopic group (TM group). Randomization was performed using a computer-generated program with a block size of four. The randomization codes were concealed in opaque, sealed envelopes opened one day before the surgery by orthopedic residents who were not involved in the study. All operations were performed by a single spine surgeon who specialized in minimally invasive spine surgery, with more than 200 cases in each operation. Although the surgeon could not be blinded, the patients, data collector, and analyzer were blinded. All patients in both groups were given the same premedication, postoperative pain control, and postoperative rehabilitation protocol. The patients were followed up for 24 months after surgery at the outpatient department (OPD) or via telephone calls due to the coronavirus disease 2019 (COVID-19) pandemic.
Surgical technique
All surgeries were performed under general anesthesia in both groups. All patients were placed in the prone position on a radiolucent table. Unilateral laminotomy with decompression (ULBD) was performed in both groups.
Full-endoscopic technique
A 1-cm-long paramedian skin incision was made on the side with the predominant radicular symptoms. A blunt dilator, followed by an endoscopic working sleeve, was inserted toward the inferomedial edge of the upper lamina. Ipsilateral laminotomy was performed using a high-speed burr and Kerrison punches under direct endoscopic visual control and continuous fluid irrigation, and the ligamentum flavum was resected. Contralateral decompression was performed by undercutting the base of spinous process and contralateral lamina called the “over the top technique.” The remaining ligamentum flavum was excised carefully (Fig. 1). No drain was placed at the end of the surgery.
Endoscopic view of intraoperative findings. a An ipsilateral laminotomy was performed, and the ipsilateral traversing root and dural sac were decompressed. b Undercutting the base of the spinous process and contralateral lamina to access the contralateral side called “over the top technique.” c Contralateral decompression was performed, and the contralateral traversing root was decompressed
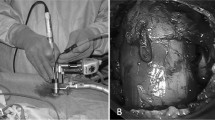
Tubular-based microscopic technique
A 3-cm-long paramedian skin incision was made on the side with the predominant radicular symptoms. After splitting the lumbar fascia and paraspinal muscles, serial tubular dilators, followed by a tubular retractor, were applied and attached to the operating table. Under microscopic visualization, the remaining paraspinal muscles and soft tissue over the lamina and the medial part of the facet joint were removed. Unilateral laminotomy and decompression were performed in the same manner as mentioned in the full-endoscopic technique (Fig. 2). No drain was placed at the end of the surgery.
Outcome measurement
All patients completed the questionnaires on the day prior to the surgery, at days 1 and 2 and 6 weeks, and 3, 6, 12, and 24 months after surgery, either by visiting the OPD or telephone calls due to the COVID-19 pandemic (the 1-day postoperative data collected at the inpatient ward). All the data were collected by a blinded research assistant. The primary outcome was the improvement in the Oswestry Disability Index (ODI) score at the 24-month follow-up visit.
Demographic data, including age, sex, body mass index (BMI), comorbidity, predominant side, area of stenosis, and affected level, were analyzed in both groups. Functional outcomes, including the visual analog scale (VAS) score for back and leg pain, ODI score, European Quality of Life-5 Dimensions (EQ-5D) score, and walking time, were analyzed preoperatively and during 24 months postoperatively in both groups. In addition, patient satisfaction rates according to the modified MacNab criteria at 24 months postoperative were compared. Surgery-related outcomes including operative time, estimated blood loss, radiation exposure, length of hospital stay, peri- and postoperative complications (e.g., incidental durotomy, surgical site infection, postoperative dysesthesia, and postoperative instability), and revision surgery were also collected and analyzed.
Statistical analysis
We calculated a sample size using non-inferiority trial formula with an 80% of power, type I error of 0.05, and non-inferiority margin of 12.8 points in ODI score [27]. Assuming a dropout rate of 10%, 60 patients (30 patients in each group) were required. Non-inferiority of the full-endoscopic technique was considered if the upper limit of the one-sided 95% confidence interval (CI) for the mean difference in ODI score at 24 months was lower than 12.8 points.
We analyzed all clinical data based on the intention-to-treat (ITT) principle. However, our primary outcome was analyzed on the basis of the per-protocol (PP) principle. To prove the non-inferiority of the full-endoscopic technique, both ITT and PP strategies were applied for the primary outcome. Quantitative and qualitative data were compared using an independent t-test and a Chi-square test, respectively. Statistical significance was set at P < 0.05. Outcomes with two or more measurements per patient were analyzed using regression based on a generalized estimating equation (GEE) approach with an identity link for continuous outcomes. All statistical analyses were conducted using the Stata 17 software (StataCorp LLC, College Station, TX, USA).
Results
Baseline characteristics
A total of 65 patients were assessed for eligibility. Five patients were excluded (one patient did not meet the inclusion criteria, and four patients met the exclusion criteria). The remaining 60 patients were randomly assigned to the FE and TM groups, with 30 patients in each group. Crossover was not detected in either group. Five patients (three patients in the FE group and two patients in the TM group) were lost to follow-up prior to the 24-month follow-up period (one patient died from COVID-19 infection, and four patients did not visit the OPD or answer the telephone calls) (Fig. 3). The baseline characteristics of the two groups were compared. No significant difference was observed in the baseline demographic and preoperative data between the two groups (all p > 0.05) (Table 1).
Primary outcome
Based on the ITT analysis, the mean ODI score at 24 months postoperative was 9.48 ± 10.05 (mean change, − 33.62; 95% CI, − 38.58 to − 28.66) in the FE group and 11.53 ± 13.21 (mean change, − 32.3; 95% CI, − 38.57 to − 26.04) in the TM group, demonstrating a significant improvement from the preoperative baseline in both groups (P < 0.0001). However, the mean difference of improvement in ODI score at 24 months postoperative between the two groups was − 1.31 (95% CI, − 9.3 to 6.68; p = 0.748; Table 2 and Fig. 4c). Based on per-protocol analysis, the mean difference of improvement in ODI score at 24 months postoperative was − 3.34 (95% CI, − 11.14 to 4.45; p = 0.4). Therefore, full-endoscopic decompression was confirmed to be non-inferiority based on both ITT and PP analyses (Table 3).
Secondary outcomes
A significant improvement was observed in all secondary outcomes, including VAS score for back pain, VAS score for leg pain, EQ-5D score, and walking time postoperatively (p < 0.0001). The improvement in the mean VAS score for back pain in the FE group was significantly greater than that in the TM group at day 1 and 6, 12, and 24 months after surgery (p = 0.041, 0.004, 0.009, and 0.037, respectively; Table 2, Fig. 4a). However, no significant difference was observed in terms of improvement in the VAS score of leg pain, EQ-5D score, and walking time at any time point (all p > 0.05; Table 2, Fig. 4b, d, and e). Patient satisfaction rates measured by the modified MacNab criteria were 86.7% in the FE group and 83.3% in the TM group, with excellent or good results at 24 months after surgery (p = 0.261; Fig. 5).
Surgery-related outcomes
The mean operative time and radiation exposure during surgery were similar between the two groups (p = 0.549 and p = 0.096, respectively). However, the mean estimated blood loss was significantly lower in the FE group (10.1 ± 6.86 vs. 39.17 ± 35.77, p < 0.001). Moreover, the length of the hospital stays after surgery was significantly shorter in the FE group (36 ± 15.11 vs. 46.4 ± 15.35, p = 0.011). The peri- and postoperative complication rates were 10% in the FE group and 20% in the TM group, which were not significantly different between the two groups (p = 0.278). One patient in the TM group experienced a dural tear intraoperatively, which was repaired during surgery with fibrin glue. One patient in the TM group experienced a superficial surgical site infection that required continuous wound dressing and prolonged oral antibiotics. Two patients (one patient in each group) experienced ipsilateral dysesthesia, and four patients (two patients in each group) experienced contralateral dysesthesia after surgery. However, all patients recovered completely after receiving epidural steroid injections. All patients underwent dynamic radiography at 12 and 24 months after surgery to evaluate postoperative instability [28]. Instability was defined as a translation > 4 mm or sagittal angulation change > 11° on flexion and extension radiographs [29]. One patient in the TM group developed instability at 12 months postoperatively and required spinal fusion surgery. Up to 18 months after surgery, three patients (one patient in the FE group and two patients in the TM group) underwent revision surgery with an additional spinal fusion procedure due to postoperative instability and/or severe back pain (VAS ≥ 8) with functional impairment (p = 0.554) (Table 3).
Discussion
Conventional laminectomy is the traditional procedure for patients with lumbar spinal stenosis. Turner et al. [30] reported an overall success rate of 64% in conventional laminectomy. However, conventional surgery also has several disadvantages. Extensive open surgical approaches to the target pain generator require muscle resection, resection of the lamina, spinous process, and some parts of the facet joints not only injure the paraspinal musculature but also potentially cause iatrogenic instability, which subsequently requires additional spinal fusion [31]. Recently, various MISS techniques have been developed to minimize the resection of posterior spinal structures and facet joints to preserve spinal stability. Spetzger et al. [32] demonstrated the feasibility of microscopic ULBD in cadavers. Subsequently, Mobbs et al. conducted a comparative study between microscopic and open decompressive laminectomy. The microscopic ULBD technique has shown favorable outcomes with additional benefits in terms of less invasiveness [17]. The full-endoscopic technique was initially performed in patients with lumbar disc herniation and later in those with lumbar spinal stenosis [33, 34]. Previous studies have shown comparable effectiveness and favorable outcomes in patients with lumbar spinal stenosis treated with full-endoscopic decompression compared to open microscopic decompression [22, 23]. Currently, full-endoscopic and tubular-based microscopic techniques are widely performed in patients with degenerative spinal diseases, including lumbar spinal stenosis. A comparative study of these two techniques is lacking. Thus, we conducted a prospective randomized controlled trial to compare the functional outcomes between full-endoscopic decompression and tubular-based microscopic decompression in patients with single-level lumbar spinal stenosis.
In our study, successful operations were performed in 60 patients, but only 55 patients completed the 24-month follow-up period. According to the ITT analysis, 60 patients were included in the statistical analysis. Based on the per-protocol population, we excluded patients who underwent revision surgery and were lost to follow-up. Our primary outcome, the mean difference in ODI score at 24 months postoperatively, was similar to the results of previous studies [22, 23]. However, the tubular retractor was not applied in microscopic surgery in the previous study, which is required for microscopic decompression. The postoperative functional outcomes in our study, including VAS scores for back and leg pain, EQ-5D score, walking time, and patient satisfaction rate according to the modified MacNab criteria, were significantly improved in both groups. The FE group showed statistically significant improvements in the mean VAS score for back pain at 1 day and 6, 12, and 24 months after surgery. However, the mean difference in improvement in VAS score for back pain did not reach the minimum clinically important difference of 3 points at any time point [24]. These results may be due to less muscle injury from soft tissue trauma, less bone resection, and greater preservation of the facet joint, leading to a lower rate of iatrogenic instability. This study also showed a significant improvement in the mean VAS of leg pain, EQ-5D, and walking time after surgery in both groups, indicating adequate decompression. The patient satisfaction rates according to the modified MacNab at 24 months postoperative were not significantly different between the two groups and were comparable to the results of previous studies [23, 35]. The length of hospital stay was also significantly shorter in the FE group than in the TM group. We assumed that due to less damage to the posterior spinal structures during the surgery, postoperative back pain was reduced, leading to faster recovery and earlier ambulation. Estimated blood loss, summarized by intraoperative blood loss and Redivac drain output, was significantly lower in the FE group. This result was thought to be due to less dissection of the paraspinal muscle and bone, easier control of bleeding under endoscopic visualization, and vascular vasoconstriction due to continuous fluid irrigation [36]. Although the exact amount of blood loss in the FE group was difficult to measure due to continuous saline irrigation during surgery, we calculated the intraoperative blood loss in the FE group using hematocrit from the rinsed solution compared to the hematocrit from the patient’s blood [37]. The mean operative time was comparable between the two groups. Since the operative time in full-endoscopic surgery depends on many factors, especially the surgeon’s experience, the operative time could be shortened by an experienced spine surgeon [38, 39]. The amount of radiation exposure during surgery was slightly higher in the FE group, although the difference was not statistically significant. The complication rates were somewhat higher in the TM group, but no significant difference was found between the two groups, which is similar to a previous study [40]. No major complication events were observed in any of the groups. The revision surgery rates were also not significantly different between groups.
Our study has some limitations. First, although a randomized controlled study was performed, the surgeons could not be blinded to the operation. However, both the patients and the research assistant, who evaluated the results and collected the data, were blinded. Therefore, the results were less likely to be affected by the single-blind study design. Second, full-endoscopic decompression is a highly demanding technique that requires a learning curve. Due to the limited number of experienced surgeons in full-endoscopic surgery, generalizability might be restricted. However, the number of trained surgeons has continued to increase annually. Finally, the follow-up time of 24 months postoperatively was too short to detect any long-term clinical outcomes and complications. Further long-term clinical studies are required.
Conclusion
The full-endoscopic decompression technique demonstrated non-inferiority to the tubular-based microscopic decompression technique over 24-month follow-up. Furthermore, this technique has several advantages, including less postoperative back pain, less blood loss, and shorter length of postoperative hospital stay. Therefore, full-endoscopic decompression is considered an alternative treatment for patients with degenerative lumbar spinal stenosis.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Waldrop R, Cheng J, Devin C, McGirt M, Fehlings M, Berven S (2015) The burden of spinal disorders in the elderly. Neurosurgery 77(Suppl 4):S46-50. https://doi.org/10.1227/NEU.0000000000000950
Yabe Y, Hagiwara Y, Ando A, Tsuchiya M, Minowa T, Takemura T et al (2015) Chondrogenic and fibrotic process in the ligamentum flavum of patients with lumbar spinal canal stenosis. Spine 40(7):429–435. https://doi.org/10.1097/BRS.0000000000000795
Chad DA (2007) Lumbar spinal stenosis. Neurol Clin 25(2):407–418. https://doi.org/10.1016/j.ncl.2007.01.003
Benoist M (2002) The natural history of lumbar degenerative spinal stenosis. Joint Bone Spine 69(5):450–457. https://doi.org/10.1016/s1297-319x(02)00429-3
Sengupta DK, Herkowitz HN (2003) Lumbar spinal stenosis: treatment strategies and indications for surgery. Orthop Clin North Am 34(2):281–295. https://doi.org/10.1016/s0030-5898(02)00069-x
Tsai RY, Yang RS, Bray RS Jr (1998) Microscopic laminotomies for degenerative lumbar spinal stenosis. J Spinal Disord 11(5):389–394
Ikuta K, Arima J, Tanaka T, Oga M, Nakano S, Sasaki K et al (2005) Short-term results of microendoscopic posterior decompression for lumbar spinal stenosis. J Neurosurg Spine 2(5):624–633. https://doi.org/10.3171/spi.2005.2.5.0624
Yagi M, Okada E, Ninomiya K, Kihara M (2009) Postoperative outcome after modified unilateral-approach microendoscopic midline decompression for degenerative spinal stenosis. J Neurosurg Spine 10(4):293–299. https://doi.org/10.3171/2009.1.SPINE08288
Choi CM, Chung JT, Lee SJ, Choi DJ (2016) How I do it? Biportal endoscopic spinal surgery (BESS) for treatment of lumbar spinal stenosis. Acta Neurochir 158(3):459–463. https://doi.org/10.1007/s00701-015-2670-7
Komp M, Hahn P, Merk H, Godolias G, Ruetten S (2011) Bilateral operation of lumbar degenerative central spinal stenosis in full-endoscopic interlaminar technique with unilateral approach: prospective 2-year results of 74 patients. J Spinal Disord Tech 24(5):281–287. https://doi.org/10.1097/BSD.0b013e3181f9f55e
Phan K, Mobbs RJ (2016) Minimally invasive versus open laminectomy for lumbar stenosis: a systematic review and meta-analysis. Spine 41(2):E91–E100. https://doi.org/10.1097/BRS.0000000000001161
Lee CW, Yoon KJ, Ha SS (2019) Comparative analysis between three different lumbar decompression techniques (microscopic, tubular, and endoscopic) in lumbar canal and lateral recess stenosis: preliminary report. Biomed Res Int 2019:6078469. https://doi.org/10.1155/2019/6078469
Rahman M, Summers LE, Richter B, Mimran RI, Jacob RP (2008) Comparison of techniques for decompressive lumbar laminectomy: the minimally invasive versus the “classic” open approach. Minim Invasive Neurosurg 51(2):100–105. https://doi.org/10.1055/s-2007-1022542
Asgarzadie F, Khoo LT (2007) Minimally invasive operative management for lumbar spinal stenosis: overview of early and long-term outcomes. Orthop Clin North Am 38(3):387–399. https://doi.org/10.1016/j.ocl.2007.02.006
Kim HS, Sharma SB, Raorane HD, Kim KR, Jang IT (2021) Early results of full-endoscopic decompression of lumbar central canal stenosis by outside-in technique: a clinical and radiographic study. Medicine 100(39):e27356. https://doi.org/10.1097/MD.0000000000027356
Phan K, Teng I, Schultz K, Mobbs RJ (2017) Treatment of lumbar spinal stenosis by microscopic unilateral laminectomy for bilateral decompression: a technical note. Orthop Surg 9(2):241–246. https://doi.org/10.1111/os.12335
Mobbs RJ, Li J, Sivabalan P, Raley D, Rao PJ (2014) Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article. J Neurosurg Spine 21(2):179–186. https://doi.org/10.3171/2014.4.SPINE13420
Toyoda H, Nakamura H, Konishi S, Dohzono S, Kato M, Matsuda H (2011) Clinical outcome of microsurgical bilateral decompression via unilateral approach for lumbar canal stenosis: minimum five-year follow-up. Spine 36(5):410–415. https://doi.org/10.1097/BRS.0b013e3181d25829
Kim YB, Hyun SJ (2007) Clinical applications of the tubular retractor on spinal disorders. J Korean Neurosurg Soc 42(4):245–250. https://doi.org/10.3340/jkns.2007.42.4.245
Palmer S, Turner R, Palmer R (2002) Bilateral decompression of lumbar spinal stenosis involving a unilateral approach with microscope and tubular retractor system. J Neurosurg 97(2 Suppl):213–217. https://doi.org/10.3171/spi.2002.97.2.0213
Hasan S, Hartl R, Hofstetter CP (2019) The benefit zone of full-endoscopic spine surgery. J Spine Surg 5(Suppl 1):S41–S56. https://doi.org/10.21037/jss.2019.04.19
Komp M, Hahn P, Oezdemir S, Giannakopoulos A, Heikenfeld R, Kasch R et al (2015) Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician 18(1):61–70
Ruetten S, Komp M, Merk H, Godolias G (2009) Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine 10(5):476–485. https://doi.org/10.3171/2008.7.17634
Lee CH, Choi M, Ryu DS, Choi I, Kim CH, Kim HS et al (2018) Efficacy and safety of full-endoscopic decompression via interlaminar approach for central or lateral recess spinal stenosis of the lumbar spine: a meta-analysis. Spine 43(24):1756–1764. https://doi.org/10.1097/BRS.0000000000002708
Chen KT, Choi KC, Shim HK, Lee DC, Kim JS (2022) Full-endoscopic versus microscopic unilateral laminotomy for bilateral decompression of lumbar spinal stenosis at L4–L5: comparative study. Int Orthop. https://doi.org/10.1007/s00264-022-05549-0
Piaggio G, Elbourne DR, Pocock SJ, Evans SJ, Altman DG, C Group (2012) Reporting of noninferiority and equivalence randomized trials: extension of the CONSORT 2010 statement. JAMA 308(24):2594–2604. https://doi.org/10.1001/jama.2012.87802
Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY (2008) Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the oswestry disability index, medical outcomes study questionnaire short form 36, and pain scales. Spine J 8(6):968–974. https://doi.org/10.1016/j.spinee.2007.11.006
White AA, Panjabi MM (1990) Clinical biomechanics of the spine, 2nd edn. Lippincott Williams and Wilkins, Philadelphia
Xue J, Chen H, Zhu B, Li X, Ouyang Z, Li S et al (2021) Percutaneous spinal endoscopy with unilateral interlaminar approach to perform bilateral decompression for central lumbar spinal stenosis: radiographic and clinical assessment. BMC Musculoskelet Disord 22(1):236. https://doi.org/10.1186/s12891-021-04100-3
Turner JA, Ersek M, Herron L, Deyo R (1992) Surgery for lumbar spinal stenosis attempted meta-analysis of the literature. Spine 17(1):1–8. https://doi.org/10.1097/00007632-199201000-00001
Guha D, Heary RF, Shamji MF (2015) Iatrogenic spondylolisthesis following laminectomy for degenerative lumbar stenosis: systematic review and current concepts. Neurosurg Focus 39(4):E9. https://doi.org/10.3171/2015.7.FOCUS15259
Spetzger U, Bertalanffy H, Naujokat C, von Keyserlingk DG, Gilsbach JM (1997) Unilateral laminotomy for bilateral decompression of lumbar spinal stenosis. Part I: anatomical and surgical considerations. Acta Neurochir 139(5):392–396. https://doi.org/10.1007/bf01808872
Mayer HM, Brock M (1993) Percutaneous endoscopic lumbar discectomy (PELD). Neurosurg Rev 16(2):115–120. https://doi.org/10.1007/BF00258242
Ahn Y, Lee SH, Park WM, Lee HY (2003) Posterolateral percutaneous endoscopic lumbar foraminotomy for L5–S1 foraminal or lateral exit zone stenosis. J Neurosurg 99(3 Suppl):320–323. https://doi.org/10.3171/spi.2003.99.3.0320
Ruetten S, Komp M, Hahn P, Oezdemir S (2013) Decompression of lumbar lateral spinal stenosis: full-endoscopic, interlaminar technique. Oper Orthop Traumatol 25(1):31–46. https://doi.org/10.1007/s00064-012-0195-2
Torudom Y, Dilokhuttakarn T (2016) Two portal percutaneous endoscopic decompression for lumbar spinal stenosis: preliminary study. Asian Spine J 10(2):335–342. https://doi.org/10.4184/asj.2016.10.2.335
Sun DD, Lv D, Wu WZ, Ren HF, Bao BH, Liu Q et al (2020) Estimation and influence of blood loss under endoscope for percutaneous endoscopic lumbar discectomy (PELD): a clinical observational study combined with in vitro experiment. J Orthop Surg Res 15(1):281. https://doi.org/10.1186/s13018-020-01797-1
Ahn J, Iqbal A, Manning BT, Leblang S, Bohl DD, Mayo BC et al (2016) Minimally invasive lumbar decompression-the surgical learning curve. Spine J 16(8):909–916. https://doi.org/10.1016/j.spinee.2015.07.455
Park SM, Kim HJ, Kim GU, Choi MH, Chang BS, Lee CK et al (2019) Learning curve for lumbar decompressive laminectomy in biportal endoscopic spinal surgery using the cumulative summation test for learning curve. World Neurosurg 122:e1007–e1013. https://doi.org/10.1016/j.wneu.2018.10.197
Heo DH, Lee DC, Park CK (2019) Comparative analysis of three types of minimally invasive decompressive surgery for lumbar central stenosis: biportal endoscopy, uniportal endoscopy, and microsurgery. Neurosurg Focus 46(5):E9. https://doi.org/10.3171/2019.2.FOCUS197
Acknowledgements
We would like to acknowledge Miss Cheunrueti Yeekian, PhD, for the statistical consultant and analysis in this study. The author (G.X.L.) wishes to acknowledge the financial support of the “Xiamen Health High-Level Talent Training Program.”
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
VK and KJ helped in conceptualization; VK and TT helped in methodology and writing—original draft preparation; TT performed formal analysis and investigation; GXL, WS, WL, WY, JSK, and KJ helped in writing—review and editing; VK supervised the study.
Corresponding author
Ethics declarations
Conflict of interest
JSK is currently a consultant for RIWOSpine, GmbH, Germany, and Elliquence, LLC, USA. WS and WL are currently speakers for Medtronic company. For the remaining authors, none were declared.
Ethical standard
The trial was registered at the Thai Clinical Trials Registry (TCTR2019217001). Institutional review board (IRB) approval was obtained from the Queen Savang Vadhana Memorial Hospital.
Informed consent
All participants provided oral and written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kotheeranurak, V., Tangdamrongtham, T., Lin, GX. et al. Comparison of full-endoscopic and tubular-based microscopic decompression in patients with lumbar spinal stenosis: a randomized controlled trial. Eur Spine J 32, 2736–2747 (2023). https://doi.org/10.1007/s00586-023-07678-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07678-5