Abstract
Purpose
Patient-reported outcome measures (PROMs) are integral to the assessment of treatment success, but loss to follow-up (attrition) may lead to bias in the results reported. We sought to evaluate the extent, nature and implications of attrition in a long-established, single-centre spine registry.
Methods
The registry contained the data of 15,264 consecutive spine surgery patients. PROMs included the Core Outcome Measures Index (COMI) and a rating of the Global Treatment Outcome (GTO) and Satisfaction with Care. Baseline characteristics associated with returning a 12-month PROM (= “responder”) were analysed (logistic regression). The 3-month outcomes of 12-month responders versus 12-month non-responders were compared (ANOVA and Chi-square).
Results
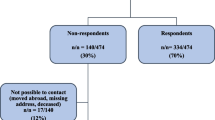
In total, 14,758/15,264 (97%) patients (60 ± 17y; 46% men) had consented to the use of their registry data for research. Preoperative, 3-month post-operative and 12-month post-operative PROMs were returned by 91, 90 and 86%, respectively. Factors associated with being a 12-month responder included: greater age, born in the country of the study, no private/semi-private insurance, better baseline status (lower COMI score), fewer previous surgeries, less comorbidity and no perioperative medical complications. 12-month non-responders had shown significantly worse outcomes in their 3-month PROMs than had 12-month responders (respectively, 66% vs 80% good GTO (“treatment helped/helped a lot”); 77% vs 88% satisfied/very satisfied; and 49% vs 63% achieved MCIC on COMI).
Conclusion
Although attrition in this cohort was relatively low, 12-month non-responders displayed distinctive characteristics and their early outcomes were significantly worse than those of 12-month responders. If loss to follow-up is not addressed, treatment success will likely be overestimated, with erroneously optimistic results being reported.


Similar content being viewed by others
References
de Beurs E, Warmerdam L, Twisk J (2019) Bias through selective inclusion and attrition: representativeness when comparing provider performance with routine outcome monitoring data. Clin Psychol Psychother 26:430–439
Bisson EF, Mummaneni PV, Knightly J, Alvi MA, Goyal A, Chan AK, Guan J, Biase M, Strauss A, Glassman S, Foley K, Slotkin JR, Potts E, Shaffrey M, Shaffrey CI, Haid RW, Fu KM, Wang MY, Park P, Asher AL, Bydon M (2020) Assessing the differences in characteristics of patients lost to follow-up at 2 years: results from the quality outcomes database study on outcomes of surgery for grade I spondylolisthesis. J neurosurg Spine 33:643–651
Hojmark K, Stottrup C, Carreon L, Andersen MO (2016) Patient-reported outcome measures unbiased by loss of follow-up. single-center study based on Danespine, the Danish spine surgery registry. Eur Spine J 25:282–286
Elkan P, Lagerback T, Moller H, Gerdhem P (2018) Response rate does not affect patient-reported outcome after lumbar discectomy. Eur Spine J 27:1538–1546
Endler P, Ekman P, Hellstrom F, Moller H, Gerdhem P (2020) Minor effect of loss to follow-up on outcome interpretation in the Swedish spine register. Eur Spine J 29:213–220
Parai C, Hagg O, Willers C, Lind B, Brisby H (2020) Characteristics and predicted outcome of patients lost to follow-up after degenerative lumbar spine surgery. Eur Spine J 29:3063–3073
Solberg TK, Sorlie A, Sjaavik K, Nygaard OP, Ingebrigtsen T (2011) Would loss to follow-up bias the outcome evaluation of patients operated for degenerative disorders of the lumbar spine? Acta Orthop 82:56–63
Schroder ML, de Wispelaere MP, Staartjes VE (2019) Predictors of loss of follow-up in a prospective registry: which patients drop out 12 months after lumbar spine surgery? Spine J 19:1672–1679
Norquist BM, Goldberg BA, Matsen FA 3rd (2000) Challenges in evaluating patients lost to follow-up in clinical studies of rotator cuff tears. J Bone Joint Surg Am 82:838–842
Murray DW, Britton AR, Bulstrode CJ (1997) Loss to follow-up matters. J Bone Joint Surg Br 79:254–257
Fekete TF, Loibl M, Jeszenszky D, Haschtmann D, Banczerowski P, Kleinstuck FS, Becker HJ, Porchet F, Mannion AF (2018) How does patient-rated outcome change over time following the surgical treatment of degenerative disorders of the thoracolumbar spine? Eur Spine J 27:700–708
Parai C, Hägg O, Lind B, Brisby H (2019) Follow-up of degenerative lumbar spine surgery-PROMs stabilize after 1 year: an equivalence study based on Swespine data. Eur Spine J 28:2187–2197
Mannion AF, Porchet F, Kleinstuck FS, Lattig F, Jeszenszky D, Bartanusz V, Dvorak J, Grob D (2009) The quality of spine surgery from the patient’s perspective: part 2. minimal clinically important difference for improvement and deterioration as measured with the core outcome measures index. Eur Spine J 18:374–379
Roder C, Chavanne A, Mannion AF, Grob D, Aebi M, El-Kerdi A (2005) SSE spine tango–content, workflow, set-up. www.eurospine.org-spine tango. a European spine registry. Eur Spine J 14:920–924
Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Semmer NK, Jacobshagen N, Dvorak J, Boos N (2005) Outcome assessment in low back pain: how low can you go? Eur Spine J 14:1014–1026
Ferrer M, Pellise F, Escudero O, Alvarez L, Pont A, Alonso J, Deyo R (2006) Validation of a minimum outcome core set in the evaluation of patients with back pain. Spine 31:1372–1379
Deyo RA, Battié M, Beurskens AJHM, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Von Korff M, Waddell G (1998) Outcome measures for low back pain research. Propos Stand Spine 23:2003–2013
Fankhauser C, Mutter U, Aghayev E, Mannion AF (2012) Validity and responsiveness of the core outcome measures index (COMI) for the neck. Eur Spine J 21:101–114
Mannion AF, Porchet F, Kleinstück F, Lattig F, Jeszenszky D, Bartanusz V, Dvorak J, Grob D (2009) The quality of spine surgery from the patient’s perspective: part 1. the core outcome measures index (COMI) in clinical practice. Eur Spine J 18:367–373
Abdeldaiem A, Saweeres ESB, Shehab-Eldien AA, Mannion AF, Rehan Youssef A (2020) Cross-cultural adaptation and validation of the Arabic version of the core outcome measures index for the back (COMI-back) in patients with non-specific low back pain. Eur Spine J 29:2413–2430
Fitz-Henry J (2011) The ASA classification and peri-operative risk. Ann R Coll Surg Engl 93:185–187
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43:1130–1139
Austin PC, Tu JV (2004) Automated variable selection methods for logistic regression produced unstable models for predicting acute myocardial infarction mortality. J Clin Epidemiol 57:1138–1146. https://doi.org/10.1016/j.jclinepi.2004.04.003
Schulz KF, Grimes DA (2002) Sample size slippages in randomised trials: exclusions and the lost and wayward. Lancet 359:781–785
Etter JF, Perneger TV (1997) Analysis of non-response bias in a mailed health survey. J Clin Epidemiol 50:1123–1128. https://doi.org/10.1016/s0895-4356(97)00166-2
Tzogiou C, Boes S, Brunner B (2021) What explains the inequalities in health care utilization between immigrants and non-migrants in Switzerland? BMC Public Health 21:530
Hutchings A, Grosse Frie K, Neuburger J, van der Meulen J, Black N (2013) Late response to patient-reported outcome questionnaires after surgery was associated with worse outcome. J Clin Epidemiol 66:218–225
Mannion AF, Mariaux F, Reitmeir R, Fekete TF, Haschtmann D, Loibl M, Jeszenszky D, Kleinstuck FS, Porchet F, Elfering A (2020) Development of the “core yellow flags index” (CYFI) as a brief instrument for the assessment of key psychological factors in patients undergoing spine surgery. Eur Spine J 29:1935–1952
Müller D, Haschtmann D, Fekete TF, Kleinstück F, Reitmeir R, Loibl M, O’Riordan D, Porchet F, Jeszenszky D, Mannion AF (2022) Development of a machine-learning based model for predicting multidimensional outcome after surgery for degenerative disorders of the spine. Eur Spine J 31:2125–2136
Kim J, Lonner JH, Nelson CL, Lotke PA (2004) Response bias: effect on outcomes evaluation by mail surveys after total knee arthroplasty. J Bone Joint Surg Am 86:15–21
Ludemann R, Watson DI, Jamieson GG (2003) Influence of follow-up methodology and completeness on apparent clinical outcome of fundoplication. Am J Surg 186:143–147
Mannion AF, Impellizzeri FM, Leunig M, Jeszenszy D, Becker HJ, Haschtmann D, Preiss S, Fekete TF (2018) EUROSPINE 2017 FULL PAPER AWARD: time to remove our rose-tinted spectacles: a candid appraisal of the relative success of surgery in over 4500 patients with degenerative disorders of the lumbar spine, hip or knee. Eur Spine J 27:778–788
Stromqvist B, Fritzell P, Hagg O, Jonsson B (2009) The Swedish Spine Register: development, design and utility. Eur Spine J 18(Suppl 3):294–304
Sackett DL (1998) Evidence-based medicine. Spine 23:1085–1086
Heymans MW, van Buuren S, Knol DL, van Mechelen W, de Vet HC (2007) Variable selection under multiple imputation using the bootstrap in a prognostic study. BMC Med Res Methodol 7:33
Acknowledgements
First and foremost, we would like to thank Gordana Balaban for her diligent work in running and managing our Spine Outcomes database since its inception. We are also grateful to our other research assistants who have helped with the administration of the Spine Tango Surgery and Patient Self-Assessment forms over the years, including Julian Amacker, Kirsten Clift, Selina Nauer, Sara Preziosa, Stéphanie Dosch, Riccardo Curatolo, Dorian Braun, Carol Gross and Selina Nager. We thank all the patients of the Schulthess Klinik who have contributed data to our in-house registry and kindly allowed us to use that data for research. We also thank past surgeons of the Schulthess Klinik Spine Center who dutifully completed their Spine Tango documentation forms for the spine surgeries they performed.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest in relation to the presented work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mannion, A.F., Fekete, T.F., O’Riordan, D. et al. Does loss to follow-up lead to an overestimation of treatment success? Findings from a spine surgery registry of over 15,000 patients. Eur Spine J 32, 813–823 (2023). https://doi.org/10.1007/s00586-023-07541-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07541-7