Abstract
Purpose
Epidural corticosteroid injections (ESI) are a mainstay of nonoperative treatment for patients with lumbar spine pathology. Recent literature evaluating infection risk following ESI after elective orthopedic surgery has produced conflicting evidence. Our primary objective was to review the literature and provide a larger meta-analysis analyzing the temporal effects of steroid injections on the risk of infection following lumbar spine surgery.
Methods
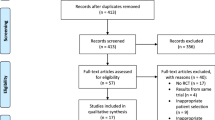
We conducted a query of the PubMed, Embase, and Scopus databases from inception until April 1, 2022 for studies evaluating the risk of infection in the setting of prior spinal steroid injections in patients undergoing lumbar spine decompression or fusion. Three meta-analyses were conducted, (1) comparing ESI within 30-days of surgery to control, (2) comparing ESI within 30-days to ESI between 1 and 3 months preoperatively, and (3) comparing any history of ESI prior to surgery to control. Tests of proportions were utilized for all comparisons between groups. Study heterogeneity was assessed via forest plots, and publication bias was assessed quantiatively via funnel plots and qualitatively with the Newcastle–Ottawa Scale.
Results
Nine total studies were included, five of which demonstrated an association between ESI and postoperative infection, while four found no association. Comparison of weighted means demonstrated no significant difference in infection rates between the 30-days ESI group and control group (2.67% vs. 1.69%, p = 0.144), 30-days ESI group and the > 30-days ESI group (2.34% vs. 1.66%, p = 0.1655), or total ESI group and the control group (1.99% vs. 1.70%, p = 0.544). Heterogeneity was low for all comparisons following sensitivity analyses.
Conclusion
Current evidence does not implicate preoperative ESI in postoperative infection rates following lumbar fusion or decompression. Operative treatment should not be delayed due to preoperative steroid injections based on current evidence. There remains a paucity of high-quality data in the literature evaluating the impact of preoperative ESI on postoperative infection rates.
Level of evidence
II.




Similar content being viewed by others
References
Vos T, Barber RM, Bell B, Global Burden Dis S et al (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet 386(9995):743–800. https://doi.org/10.1016/S0140-6736(15)60692-4
Ravindra VM, Senglaub SS, Rattani A et al (2018) Degenerative lumbar spine disease: estimating global incidence and worldwide volume. Glob Spine J 8(8):784–794. https://doi.org/10.1177/2192568218770769
Tosteson ANA, Lurie JD, Tosteson TD et al (2008) Surgical treatment of spinal stenosis with and without degenerative spondylolisthesis: cost-effectiveness after 2 years. Ann Intern Med 149(12):845–853. https://doi.org/10.7326/0003-4819-149-12-200812160-00003
Fekete T, Woernle C, Mannion AF et al (2015) The effect of epidural steroid injection on postoperative outcome in patients from the lumbar spinal stenosis outcome study. Spine 40(16):1303–1310. https://doi.org/10.1097/BRS.0000000000000969
Kaufmann TJ, Geske JR, Murthy NS et al (2013) Clinical effectiveness of single lumbar transforaminal epidural steroid injections. Pain Med 14(8):1126–1133. https://doi.org/10.1111/pme.12122
Manson NA, McKeon MD, Abraham EP (2013) Transforaminal epidural steroid injections prevent the need for surgery in patients with sciatica secondary to lumbar disc herniation: a retrospective case series. Can J Surg 56(2):89–96. https://doi.org/10.1503/cjs.014611
Manchikanti L, Pampati V, Falco FJE, Hirsch JA (2013) Assessment of the growth of epidural injections in the medicare population from 2000 to 2011. Pain Phys 16(4):E349-364
Goodman BS, Posecion LWF, Mallempati S, Bayazitoglu M (2008) Complications and pitfalls of lumbar interlaminar and transforaminal epidural injections. Curr Rev Musculoskelet Med 1(3–4):212–222. https://doi.org/10.1007/s12178-008-9035-2
Katz JN, Zimmerman ZE, Mass H, Makhni MC (2022) Diagnosis and management of lumbar spinal stenosis: a review. JAMA 327(17):1688–1699. https://doi.org/10.1001/jama.2022.5921
McIntosh AL, Hanssen AD, Wenger DE, Osmon DR (2006) Recent intraarticular steroid injection may increase infection rates in primary THA. Clin Orthop Relat Res® 451:50–54. https://doi.org/10.1097/01.blo.0000229318.51254.79
Desai A, Ramankutty S, Board T, Raut V (2009) Does intraarticular steroid infiltration increase the rate of infection in subsequent total knee replacements? Knee 16(4):262–264. https://doi.org/10.1016/j.knee.2008.12.002
Werner BC, Cancienne JM, Burrus MT, Griffin JW, Gwathmey FW, Brockmeier SF (2016) The timing of elective shoulder surgery after shoulder injection affects postoperative infection risk in medicare patients. J Shoulder Elbow Surg 25(3):390–397. https://doi.org/10.1016/j.jse.2015.08.039
Wang D, Camp CL, Ranawat AS, Coleman SH, Kelly BT, Werner BC (2017) The timing of hip arthroscopy after intra-articular hip injection affects postoperative infection risk. Arthroscopy 33(11):1988-1994.e1. https://doi.org/10.1016/j.arthro.2017.06.037
Kurtz SM, Mont MA, Chen AF et al (2021) Intra-articular corticosteroid or hyaluronic acid injections are not associated with periprosthetic joint infection risk following total knee arthroplasty. J Knee Surg 35(9):983–996. https://doi.org/10.1055/s-0040-1721128
Forsythe B, Agarwalla A, Puzzitiello RN, Sumner S, Romeo AA, Mascarenhas R (2019) The timing of injections prior to arthroscopic rotator cuff repair impacts the risk of surgical site infection. J Bone Jt Surg Am 101(8):682–687. https://doi.org/10.2106/JBJS.18.00631
Kokubun BA, Manista GC, Courtney PM, Kearns SM, Levine BR (2017) Intra-articular knee injections before total knee arthroplasty: outcomes and complication rates. J Arthroplasty 32(6):1798–1802. https://doi.org/10.1016/j.arth.2017.01.041
Kreitz TM, Mangan J, Schroeder GD et al (2021) Do preoperative epidural steroid injections increase the risk of infection after lumbar spine surgery? Spine 46(3):E197. https://doi.org/10.1097/BRS.0000000000003759
Hartveldt S, Janssen SJ, Wood KB et al (2016) Is There an association of epidural corticosteroid injection with postoperative surgical site infection after surgery for lumbar degenerative spine disease? Spine 41(19):1542–1547. https://doi.org/10.1097/BRS.0000000000001548
Seavey JG, Balazs GC, Steelman T, Helgeson M, Gwinn DE, Wagner SC (2017) The effect of preoperative lumbar epidural corticosteroid injection on postoperative infection rate in patients undergoing single-level lumbar decompression. Spine J 17(9):1209–1214. https://doi.org/10.1016/j.spinee.2017.04.003
Pisano AJ, Seavey JG, Steelman TJ, Fredericks DR, Helgeson MD, Wagner SC (2020) The effect of lumbar corticosteroid injections on postoperative infection in lumbar arthrodesis surgery. J Clin Neurosci 71:66–69. https://doi.org/10.1016/j.jocn.2019.10.015
Kazarian GS, Steinhaus ME, Kim HJ (2021) The impact of corticosteroid injection timing on infection rates following spine surgery: a systematic review and meta-analysis. Glob Spine J. https://doi.org/10.1177/21925682211026630
Papavasiliou AV, Isaac DL, Marimuthu R, Skyrme A, Armitage A (2006) Infection in knee replacements after previous injection of intra-articular steroid. J Bone Jt Surg Br 88(3):321–323. https://doi.org/10.1302/0301-620X.88B3.17136
Forlenza EM, Burnett RA, Korrapati A, Yang J, Forsythe B, Della Valle CJ (2021) Preoperative corticosteroid injections demonstrate a temporal and dose-dependent relationship with the rate of postoperative infection following total hip arthroplasty. J Arthroplasty 36(6):2033-2037.e1. https://doi.org/10.1016/j.arth.2021.01.076
Singla A, Yang S, Werner BC et al (2017) The impact of preoperative epidural injections on postoperative infection in lumbar fusion surgery. J Neurosurg Spine 26(5):645–649. https://doi.org/10.3171/2016.9.SPINE16484
Yang S, Werner BC, Cancienne JM et al (2016) Preoperative epidural injections are associated with increased risk of infection after single-level lumbar decompression. Spine J 16(2):191–196. https://doi.org/10.1016/j.spinee.2015.07.439
Støttrup CC, Andresen AK, Carreon L, Andersen MØ (2019) Increasing reoperation rates and inferior outcome with prolonged symptom duration in lumbar disc herniation surgery: a prospective cohort study. Spine J 19(9):1463–1469. https://doi.org/10.1016/j.spinee.2019.04.001
Villavicencio AT, Nelson EL, Rajpal S, Burneikiene S (2017) The timing of surgery and symptom resolution in patients undergoing transforaminal lumbar interbody fusion for lumbar degenerative disk disease and radiculopathy. Clin Spine Surg 30(6):E765–E769. https://doi.org/10.1097/BSD.0000000000000392
Rihn JA, Hilibrand AS, Radcliff K et al (2011) Duration of symptoms resulting from lumbar disc herniation: effect on treatment outcomes: analysis of the spine patient outcomes research trial (SPORT). J Bone Jt Surg Am 93(20):1906–1914. https://doi.org/10.2106/JBJS.J.00878
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
GA Wells B Shea D O’Connell et al 2000 The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses Oxford
Li P, Hou X, Gao L, Zheng X (2020) Infection risk of lumbar epidural injection in the operating theatre prior to lumbar fusion surgery. J Pain Res 13:2181–2186. https://doi.org/10.2147/JPR.S261922
Donnally CJ, Rush AJ, Rivera S et al (2018) An epidural steroid injection in the 6 months preceding a lumbar decompression without fusion predisposes patients to post-operative infections. J Spine Surg 4(3):529–533. https://doi.org/10.21037/jss.2018.09.05
Koltsov JCB, Smuck MW, Zagel A et al (2019) Lumbar epidural steroid injections for herniation and stenosis: incidence and risk factors of subsequent surgery. Spine J 19(2):199–205. https://doi.org/10.1016/j.spinee.2018.05.034
Canseco JA, Karamian BA, DiMaria SL et al (2021) Timing of preoperative surgical antibiotic prophylaxis after primary one-level to three-level lumbar fusion. World Neurosurg 153:e349–e358. https://doi.org/10.1016/j.wneu.2021.06.112
Patel HA, Cheppalli NS, Bhandarkar AW, Patel V, Singla A (2022) lumbar spinal steroid injections and infection risk after spinal surgery: a systematic review and meta-analysis. Asian Spine J. https://doi.org/10.31616/asj.2021.0164
Patel AA, Singh K, Nunley RM, Minhas SV (2016) Administrative databases in orthopaedic research: pearls and pitfalls of big data. J Am Acad Orthop Surg 24(3):172–179. https://doi.org/10.5435/JAAOS-D-13-00009
Schoenfeld AJ (2016) Research using “big data” in orthopaedic trauma: a dynasty of databases or finite research resource? J Orthop Trauma 30(5):225–227. https://doi.org/10.1097/BOT.0000000000000541
Bohl DD, Russo GS, Basques BA et al (2014) Variations in data collection methods between national databases affect study results: a comparison of the nationwide inpatient sample and national surgical quality improvement program databases for lumbar spine fusion procedures. J Bone Jt Surg Am 96(23):e193. https://doi.org/10.2106/JBJS.M.01490
Bohl DD, Basques BA, Golinvaux NS, Baumgaertner MR, Grauer JN (2014) nationwide inpatient sample and national surgical quality improvement program give different results in hip fracture studies. Clin Orthop Relat Res 472(6):1672–1680. https://doi.org/10.1007/s11999-014-3559-0
Bedard NA, Pugely AJ, McHugh MA, Lux NR, Bozic KJ, Callaghan JJ (2018) Big data and total hip arthroplasty: how do large databases compare? J Arthroplasty 33(1):41-45.e3. https://doi.org/10.1016/j.arth.2017.09.003
Shaffer WO, Baisden JL, Fernand R, Matz PG (2013) An evidence-based clinical guideline for antibiotic prophylaxis in spine surgery. Spine J 13(10):1387–1392. https://doi.org/10.1016/j.spinee.2013.06.030
Karamian BA, Toci GR, Lambrechts MJ et al (2022) Cefazolin prophylaxis in spine surgery: patients are frequently underdosed and at increased risk for infection. Spine J. https://doi.org/10.1016/j.spinee.2022.05.018
Lopez WY, Rider SM, Nwosu K et al (2019) The Impact of vancomycin and cefazolin as standard preoperative antibiotic prophylaxis on surgical site infections following instrumented spinal fusion. Spine (Phila Pa 1976) 44(6):E366–E371. https://doi.org/10.1097/BRS.0000000000002839
Centers for Disease Control and Prevention (CDC) (2012) Multistate outbreak of fungal infection associated with injection of methylprednisolone acetate solution from a single compounding pharmacy-United States, 2012. MMWR. Morbidity and mortality weekly report 61(41):839–842
Wilson-Smith A, Chang N, Lu VM et al (2018) Epidural steroids at closure after microdiscectomy/laminectomy for reduction of postoperative analgesia: systematic review and meta-analysis. World Neurosurg 110:e212–e221. https://doi.org/10.1016/j.wneu.2017.10.133
Rasmussen S, Krum-Møller DS, Lauridsen LR et al (2008) Epidural steroid following discectomy for herniated lumbar disc reduces neurological impairment and enhances recovery: a randomized study with two-year follow-up. Spine (Phila Pa 1976) 33(19):2028–2033. https://doi.org/10.1097/BRS.0b013e3181833903
Abrishamkar S, Rafiei AR, Sabouri M et al (2011) The effect of impregnated autogenous epidural adipose tissue with bupivacaine, methylprednisolone acetate or normal saline on postoperative radicular and low back pain in lumbar disc surgery under spinal anesthesia; a randomized clinical trial study*. J Res Med Sci 16(5):621–626
Aljabi Y, El-Shawarby A, Cawley DT, Aherne T (2015) Effect of epidural methylprednisolone on post-operative pain and length of hospital stay in patients undergoing lumbar microdiscectomy. The Surgeon 13(5):245–249. https://doi.org/10.1016/j.surge.2014.03.012
Keorochana G, Pairuchvej S, Setrkraising K, Arirachakaran A, Kongtharvonskul J (2018) Comparative outcomes of perioperative epidural steroids after percutaneous endoscopic lumbar discectomy for lumbar disc herniation: a randomized placebo-controlled trial. World Neurosurg 119:e244–e249. https://doi.org/10.1016/j.wneu.2018.07.122
Friedly JL, Comstock BA, Turner JA et al (2014) A randomized trial of epidural glucocorticoid injections for spinal stenosis. N Engl J Med 371(1):11–21. https://doi.org/10.1056/NEJMoa1313265
Friedly JL, Comstock BA, Turner JA et al (2017) Long-term effects of repeated injections of local anesthetic with or without corticosteroid for lumbar spinal stenosis: a randomized trial. Arch Phys Med Rehabil 98(8):1499-1507.e2. https://doi.org/10.1016/j.apmr.2017.02.029
Kreiner DS, Shaffer WO, Baisden JL et al (2013) An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J 13(7):734–743. https://doi.org/10.1016/j.spinee.2012.11.059
Fornari M, Robertson SC, Pereira P et al (2020) Conservative treatment and percutaneous pain relief techniques in patients with lumbar spinal stenosis: WFNS spine committee recommendations. World Neurosurg: X 7:100079. https://doi.org/10.1016/j.wnsx.2020.100079
Radcliff KE, Rihn J, Hilibrand A et al (2011) Does the duration of symptoms in patients with spinal stenosis and degenerative spondylolisthesis affect outcomes?: analysis of the spine outcomes research trial. Spine (Phila Pa 1976) 36(25):2197–2210. https://doi.org/10.1097/BRS.0b013e3182341edf
Acknowledgements
The authors of this manuscript would like to thank Kerri-Anne Ciesielka for assistance with statistical analysis.
Funding
The authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity for the preparation of this article. Relevant disclosures related to the topic of the article are listed on disclosure forms.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, Y., Issa, T.Z., Kanhere, A.P. et al. Preoperative epidural steroid injections do not increase the risk of postoperative infection in patients undergoing lumbar decompression or fusion: a systematic review and meta-analysis. Eur Spine J 31, 3251–3261 (2022). https://doi.org/10.1007/s00586-022-07436-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07436-z