Abstract
Purpose
To evaluate whether a set of pre-accident demographic, accident-related, post-accident treatment and psychosocial factors assessed in people with acute/subacute whiplash-associated disorders (WAD) mediate the association between pain intensity and: (1) pain interference and (2) expectations of recovery, using Bayesian networks (BNs) analyses. This study also explored the potential mediating pathways (if any) between different psychosocial factors.
Methods
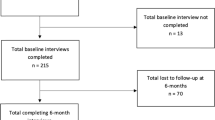
This was a cross-sectional study conducted on a sample of 173 participants with acute/subacute WAD. Pain intensity, pain interference, pessimism, expectations of recovery, pain catastrophizing, and self-efficacy beliefs were assessed. BN analyses were conducted to analyse the mediating effects of psychological factors on the association between pain intensity and pain-related outcomes.
Results
The results revealed that self-efficacy beliefs partially mediated the association between pain intensity and pain interference. Kinesiophobia partially mediated the association between self-efficacy and pain catastrophizing. Psychological factors did not mediate the association between pain intensity and expectations of recovery.
Conclusion
These results indicate that individuals with acute/subacute WAD may present with lesser pain interference associated with a determined pain intensity value when they show greater self-efficacy beliefs. As the cross-sectional nature of this study limits firm conclusions on the causal impact, researchers are encouraged to investigate the role that patient’s self-efficacy beliefs play in the transition to chronic WAD via longitudinal study designs.




Similar content being viewed by others
References
Elliott JM, Walton DM (2017) How do we meet the challenge of whiplash? J Orthop Sports Phys Ther 47:444–446. https://doi.org/10.2519/jospt.2017.0106
Bin CH, Yang KH, Wang ZG (2009) Biomechanics of whiplash injury. Chin J Traumatol—English Ed 12:305–314. https://doi.org/10.3760/cma.j.issn.1008-1275.2009.05.011
Pink J, Petrou S, Williamson E et al (2016) Economic and health-related quality of life outcomes of whiplash associated disorders. Spine 41:1378–1386. https://doi.org/10.1097/BRS.0000000000001512
Yadla S, Ratliff JK, Harrop JS (2007) Whiplash: diagnosis, treatment, and associated injuries. Curr Rev Musculoskelet Med 1:65–68. https://doi.org/10.1007/s12178-007-9008-x
Hogg-Johnson S, van der Velde G, Carroll LJ et al (2008) The burden and determinants of neck pain in the general population. Eur Spine J 17:39–51. https://doi.org/10.1007/s00586-008-0624-y
Ritchie C, Hendrikz J, Kenardy J, Sterling M (2013) Derivation of a clinical prediction rule to identify both chronic moderate/severe disability and full recovery following whiplash injury. Pain 154:2198–2206. https://doi.org/10.1016/j.pain.2013.07.001
Ritchie C, Sterling M (2016) Recovery pathways and prognosis after whiplash injury. J Orthop Sports Phys Ther 46:851–861. https://doi.org/10.2519/jospt.2016.6918
Kamper SJ, Rebbeck TJ, Maher CG et al (2008) Course and prognostic factors of whiplash: a systematic review and meta-analysis. Pain 138:617–629. https://doi.org/10.1016/j.pain.2008.02.019
Walton DEJ (2017) An integrated model of chronic whiplash-associated disorder. J Orthop Sport Phys Ther 47:462–471
Nieto R, Miró J, Huguet A (2009) The fear-avoidance model in whiplash injuries. Eur J Pain 13:518–523. https://doi.org/10.1016/j.ejpain.2008.06.005
Vangronsveld K, Peters M, Goossens M et al (2007) Applying the fear-avoidance model to the chronic whiplash syndrome. Pain 131:258–261. https://doi.org/10.1016/j.pain.2007.04.015
Campbell L, Smith A, McGregor L, Sterling M (2018) Psychological factors and the development of chronic whiplash associated disorder(s). Clin J Pain 34:755–768
Söderlund A, Sandborgh M, Johansson A-C (2017) Is self-efficacy and catastrophizing in pain-related disability mediated by control over pain and ability to decrease pain in whiplash-associated disorders? Physiother Theory Pract 33:376–385. https://doi.org/10.1080/09593985.2017.1307890
Söderlund A, Åsenlöf P (2010) The mediating role of self-efficacy expectations and fear of movement and (re)injury beliefs in two samples of acute pain. Disabil Rehabil 32:2118–2126. https://doi.org/10.3109/09638288.2010.483036
Kamper SJ, Maher CG, Menezes Costa LDC et al (2012) Does fear of movement mediate the relationship between pain intensity and disability in patients following whiplash injury? A prospective longitudinal study. Pain 153:113–119. https://doi.org/10.1016/j.pain.2011.09.023
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PCVJSI (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 12:1495–1499. https://doi.org/10.1016/j.ijsu.2014.07.013
Karcioglu O, Topacoglu H, Dikme O, Dikme O (2018) A systematic review of the pain scales in adults: which to use? Am J Emerg Med 36:707–714. https://doi.org/10.1016/j.ajem.2018.01.008
Lorig KR, Ritter PL, González VM (2003) Hispanic chronic disease self-management: a randomized community-based outcome trial. Nurs Res 52:361–369. https://doi.org/10.1097/00006199-200311000-00003
Ramírez-Maestre C, Esteve R, López-Martínez AE et al (2019) Goal adjustment and well-being: the role of optimism in patients with chronic pain. Ann Behav Med 53:597–607. https://doi.org/10.1093/abm/kay070
Hirsch JK, Britton PC, Conner KR (2010) Psychometric evaluation of the life orientation test-revised in treated opiate dependent individuals. Int J Ment Health Addict 8:423–431. https://doi.org/10.1007/s11469-009-9224-2
Ferrando PJ, Chico E, Tous M (2002) Propiedades psicométricas del test de optimismo Life Orientation Test. Psicothema 14:673–680
Sterling M, Jull G, Kenardy J (2006) Physical and psychological factors maintain long-term predictive capacity post-whiplash injury. Pain 122:102–108. https://doi.org/10.1016/j.pain.2006.01.014
Gómez L, López E, Ruiz GT (2011) Psychometric properties of the spanish version of the tampa scale for kinesiophobia (TSK). J Pain 12(4):425–35. https://doi.org/10.1016/j.jpain.2010.08.004
García Campayo J, Rodero B, Alda M et al (2008) Validación de la versión española de la escala de la catastrofización ante el dolor (Pain Catastrophizing Scale) en la fibromialgia. Med Clin (Barc) 131:487–492. https://doi.org/10.1157/13127277
Andrade Ortega JA, Delgado Martínez AD, Ruiz RA (2010) Validation of the Spanish version of the neck disability index. Spine (Phila Pa 1976) 35:E114–E118. https://doi.org/10.1157/13115352
Scutari M (2010) Learning bayesian networks with the bn learn R package. J Stat Softw 35:22
Scutari M, Nagarajan R (2013) Identifying significant edges in graphical models of molecular networks. Artif Intell Med 57:207–217. https://doi.org/10.1016/j.artmed.2012.12.006
Crombez G, Eccleston C, Van DS et al (2012) Fear-Avoidance model of chronic pain. Clin J Pain 28:475–483. https://doi.org/10.1097/AJP.0b013e3182385392
Hinkle D, Wiersma WJS (2003) Applied statistics for the behavioral sciences. Houghton Mifflin, Boston
Nagarajan R, Scutari MLS (2013) Bayesian networks in R with applications in systems biology. Verlag, New York
Nicholas MK (2007) The pain self-efficacy questionnaire: taking pain into account. Eur J Pain 11:153–163. https://doi.org/10.1016/j.ejpain.2005.12.008
Jackson T, Wang Y, Wang Y, Fan H (2014) Self-efficacy and chronic pain outcomes: a meta-analytic review. J Pain 15:800–814. https://doi.org/10.1016/j.jpain.2014.05.002
Martinez-Calderon J, Zamora-Campos C, Navarro-Ledesma S, Luque-Suarez A (2018) The role of self-efficacy on the prognosis of chronic musculoskeletal pain: a systematic review. J Pain 19:10–34. https://doi.org/10.1016/J.JPAIN.2017.08.008
Peck KR, Smitherman TA (2015) Mediator variables in headache research: methodological critique and exemplar using self-efficacy as a mediator of the relationship between headache severity and disability. Headache 55:1102–1111. https://doi.org/10.1111/head.12633
Schulz S, Brenk-Franz K, Kratz A et al (2015) Self-efficacy in multimorbid elderly patients with osteoarthritis in primary care—influence on pain-related disability. Clin Rheumatol 34:1761–1767. https://doi.org/10.1007/s10067-014-2766-0
Costa LDCM, Maher CG, McAuley JH et al (2011) Self-efficacy is more important than fear of movement in mediating the relationship between pain and disability in chronic low back pain. Eur J Pain 15:213–219. https://doi.org/10.1016/j.ejpain.2010.06.014
Wallis BJ, Lord SM, Bogduk N (1997) Resolution of psychological distress of whiplash patients following treatment by radiofrequency neurotomy: a randomised, double-blind, placebo-controlled trial. Pain 73:15–22. https://doi.org/10.1016/s0304-3959(97)00060-2
Paré C, Thibault P, Côté P et al (2019) The relation between level of catastrophizing and mental health comorbidity in individuals with whiplash injuries. Clin J Pain 35:880–886. https://doi.org/10.1097/AJP.0000000000000749
Wicksell RK, Olsson GL, Hayes SC (2010) Psychological flexibility as a mediator of improvement in acceptance and commitment therapy for patients with chronic pain following whiplash. Eur J Pain 14:1059.e1-1059.e11. https://doi.org/10.1016/j.ejpain.2010.05.001
Lee H, Hübscher M, Moseley GL et al (2015) How does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck pain. Pain 156:988–997. https://doi.org/10.1097/j.pain.0000000000000146
Vlaeyen JWS, Linton SJ (2000) Fear-avoidance and its consequences in muscle skeleton pain: a state of the art. Pain 85:317–332
Sullivan MJL, Thorn B, Rodgers W, Ward LC (2004) Path model of psychological antecedents to pain experience: experimental and clinical findings. Clin J Pain 20:164–173. https://doi.org/10.1097/00002508-200405000-00006
He C-H, Yu F, Jiang Z-C et al (2014) Fearful thinking predicts hypervigilance towards pain-related stimuli in patients with chronic pain. PsyCh J 3:189–200. https://doi.org/10.1002/pchj.57
Ohman A, Mineka S (2001) Fears, phobias, and preparedness: toward an evolved module of fear and fear learning. Psychol Rev 108:483–522. https://doi.org/10.1037/0033-295x.108.3.483
Mathews A (1990) Why worry? The cognitive function of anxiety. Behav Res Ther 28:455–468. https://doi.org/10.1016/0005-7967(90)90132-3
Ozegovic D, Carroll LJ, Cassidy JD (2010) Factors associated with recovery expectations following vehicle collision: a population-based study. J Rehabil Med 42:66–73. https://doi.org/10.2340/16501977-0466
Picha KJ, Howell DM (2017) A model to increase rehabilitation adherence to home exercise programmes in patients with varying levels of self-efficacy. Musculoskelet Care. https://doi.org/10.1002/msc.1194
Bandura A (1977) Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 84:191
Martinez-Calderon J, Flores-Cortes M, Morales-Asencio M et al (2020) Which interventions enhance pain self-efficacy in people with chronic musculoskeletal pain? A systematic review and meta analysis of randomized controlled trials including over 12,000 participants. J Orthop Sport Phys Ther 50:418–430
Ludvigsson ML, Peterson G, O’Leary S et al (2015) The effect of neck-specific exercise with, or without a behavioral approach, on pain, disability, and self-efficacy in chronic whiplash-associated disorders: a randomized clinical trial. Clin J Pain 31:294–303. https://doi.org/10.1097/AJP.0000000000000123
Bring A, Åsenlöf P, Söderlund A (2016) What is the comparative effectiveness of current standard treatment, against an individually tailored behavioural programme delivered either on the Internet or face-to-face for people with acute whiplash associated disorder? A randomized controlled trial. Clin Rehabil 30:441–453. https://doi.org/10.1177/0269215515581503
Marshall PWM, Schabrun S, Knox MF (2017) Physical activity and the mediating effect of fear, depression, anxiety, and catastrophizing on pain related disability in people with chronic low back pain. PLoS ONE 12:1–15. https://doi.org/10.1371/journal.pone.0180788
Shigetoh H, Tanaka Y, Koga M et al (2019) The mediating effect of central sensitization on the relation between pain intensity and psychological factors: a cross-sectional study with mediation analysis. Pain Res Manag 2019:3916135. https://doi.org/10.1155/2019/3916135
Liew BXW, Scutari M, Peolsson A et al (2019) Investigating the causal mechanisms of symptom recovery in chronic whiplash-associated disorders using bayesian networks. Clin J Pain 35:647–655. https://doi.org/10.1097/AJP.0000000000000728
Acknowledgements
Dr. Javier Martinez-Calderon is supported by the Universidad de Malaga through a postdoctoral grant. All authors state that they have no conflicts of interest to declare.
Funding
Dr. Javier Martinez-Calderon is supported by the University of Malaga through a postdoctoral grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared. All data are stored and protected by the University of Malaga.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pedrero-Martin, Y., Falla, D., Martinez-Calderon, J. et al. Self-efficacy beliefs mediate the association between pain intensity and pain interference in acute/subacute whiplash-associated disorders. Eur Spine J 30, 1689–1698 (2021). https://doi.org/10.1007/s00586-021-06731-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06731-5