Abstract
Purpose
The objective of the study was to determine whether all patients with spinal non-missile penetrating injuries (NMPIs) need to be managed at a tertiary neurosurgical centre.
Methods
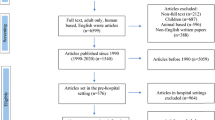
A retrospective analysis of clinical, demographic, and imaging records was performed on all NMPI patients referred to the Department of Neurosurgery at Tygerberg Academic Hospital in Cape Town, South Africa, between 1 January 2016 and 31 December 2019.
Results
Ninety-six patients were identified (94 males and 2 females) with 35 cervical, 60 thoracic, and 1 lumbar spinal stab. Eighty-six had an incomplete spinal cord injury. Six patients presented with cerebrospinal fluid (CSF) leak, all of which resolved spontaneously. MRI was performed in nine patients. Six patients had retained blades, of which 5 were removed in the emergency room (ER). Surgery was performed in two patients (cervical intramedullary abscess and a retained blade). Two patients developed meningitis, and one an intramedullary abscess. Twenty-two patients had associated injuries (pneumothorax, bowel injury). The average length of stay was 17 days, with 81% being unchanged neurologically. The average time from discharge to leaving the hospital was 11 days.
Conclusion
Early management of NMPI should include prophylactic antibiotics and wound debridement and X-ray imaging to exclude retained blades. Bowel and lung injury must be managed accordingly. Tertiary neurosurgical referral is not routinely necessary and is only warranted for deteriorating neurology, retained blades not removable in the ER, and respiratory failure secondary to spinal cord injury. Complications include meningitis and persistent CSF leak, which should be referred timeously.

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Chen Y, Tang Y, Vogel L, DeVivo M (2013) Causes of spinal cord injury. Top Spinal Cord Inj Rehabil 19:1–8
Peacock WS, Shrosbee RB, Key AD (1977) A review of 450 stab wounds of spinal cord. S Afr Med J 51:961–964
Sothmann J, Stander J, Kruger N, Dunn R (2015) Epidemiology of acute spinal cord injuries in the Groote Schuur hospital acute spinal cord injury (GSH ASCI) unit, Cape Town, South Africa, over the past 11 years. S Afr Med J 105:835
Wallace D, Sy C, Peitz G, Grandhi R (2018) Management of non-missile penetrating spinal injury. Neurosurg Rev 42:791–798
Enicker B, Gonya S, Hardcastle T (2015) Spinal stab injury with retained knife blades: 51 consecutive patients managed at a regional referral unit. Injury 46:1726–1733
Ozsoy K, Menekse G, Okten A, Guzel A (2013) Cerebrospinal fluid fistula due to penetrating trauma. Indian J Neurotrauma 10:52–54
Hart C, Williams E (1994) Epidemiology of spinal cord injuries: a reflection of changes in South African society. Paraplegia 32:709–714
Wegner L, Behardien A, Loubser C, Ryklief W, Smith D (2016) Meaning and purpose in the occupations of gang-involved young men in Cape Town. S Afr J Occup Ther 46:53–58
Walker I, Vlok A, Kamat A (2016) A double-edged sword: the effect of technological advancements in the management of neurotrauma patients. Br J Neurosurg 31(1):89–93
Le Roux JC, Dunn RN (2005) Gunshot injuries of the spine—a review of 49 cases managed at the Groote Schuur acute spinal cord injury Unit. SAJS 43:165–168
Levy M, Gans W, Wijesinghe H, SooHoo W, Adkins R, Stillerman C (1996) Use of methylprednisolone as an adjunct in the management of patients with penetrating spinal cord injury: outcome analysis. Neurosurgery 39:1141–1149
McCaughey E, Purcell M, Barnett S, Allan D (2016) Spinal cord injury caused by stab wounds: incidence, natural history, and relevance for future research. J Neurotrauma 33:1416–1421
Injury AAS (1982) Standards for neurological classification of spinal injury patients. American Spinal Injury Association, Chicago, IL
Heary R, Vaccaro A, Mesa J, Northrup B, Albert T, Balderston R, Cotler J (1997) Steroids and gunshot wounds to the spine. Neurosurgery 41:576–584
Fredericks C, Yon J, Kubasiak J, Basu A, Nagy K, Bokhari F (2016) Delayed cerebrospinal fluid leak after penetrating cervical trauma. Trauma 19:63–65
Quesnel A, Veber B, Proust F, Agasse E, Beuret Blanquart F, Verin E (2015) What are the perspectives for ventilated tetraplegics? A French retrospective study of 108 patients with cervical spinal cord injury. Ann Phys Rehabil Med 58:74–77. https://doi.org/10.1016/j.rehab.2014.12.004
Jacobsohn M, Semple P, Dunn R, Candy S (2007) Stab injuries to the spinal cord. Neurosurgery 61:1262–1267
Rall JM, Gebremariam FA, Joubert G (2019) Imaging findings of penetrating spinal cord injuries secondary to stab wounds on magnetic resonance imaging in a tertiary trauma unit, South Africa. S Afr J Rad 23:2078–6778
Harrington B, Gretschel A, Lombard C, Lonser R, Vlok A (2020) Complications, outcomes, and management strategies of non-missile penetrating head injuries. J Neurosurg. https://doi.org/10.3171/2020.4.JNS20122
Simpson R, Venger B, Narayan R (1989) Treatment of acute penetrating injuries of the spine. J Trauma: Inj, Infect, Criti Care 29:43–46
Shahlaie K, Chang D, Anderson J (2006) Nonmissile penetrating spinal injury. J Neurosurg Spine 4:400–408
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Institutional and ethical approval was obtained under the Health Research Ethics Committee of the University of Stellenbosch Number N20/03/028.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seroto, P.M., Harrington, B.M., Lombard, C. et al. The role of tertiary neurosurgical intervention in non-missile penetrating injuries of the spine. Eur Spine J 30, 1397–1401 (2021). https://doi.org/10.1007/s00586-020-06665-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06665-4