Abstract
Study design
Systematic review, meta-analysis, evidence synthesis.
Objectives
To analyse the literature evidence available to support the usage of wound drain in various scenarios of spine surgery and provide an evidence summary on the surgical practice.
Materials and methods
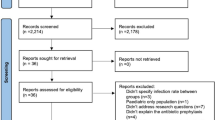
We conducted independent and duplicate electronic database searches adhering to PRISMA guidelines in PubMed, Embase, and Cochrane Library till April 2020. Quality appraisal was done as per Cochrane ROB tool, and evidence synthesis was done as per GRADE approach. Five domains of spine surgery with associated key questions were identified. Evidence tables were generated for each question and critical appraisal done as per the GRADE approach.
Results
Twenty-three studies (9—RCTs, 4—prospective studies, 10—retrospective studies) were included. Analysis of studies in cervical spine either by anterior or posterior approach and single/multilevel thoracolumbar spinal surgeries did not show any evidence of reduction in surgical site infection (SSI) or haematoma formation with the use of drain. Deformity correction surgeries and surgeries done for trauma or tumour involving spine also did not find any added benefit from the use of wound drains despite increasing the total blood loss.
Conclusion
Evidence from this review suggests that routine use of drain in various domains of spine surgery does not reduce the risk of SSI and their absence did not increase the risk of haematoma formation. The current best evidence is presented with its limitations. High-quality studies to address their use in spine surgeries in cervical, trauma, and tumour domains are required to further strengthen the evidence synthesised from available literature.






Similar content being viewed by others
References
Spina NT, Aleem IS, Nassr A, Lawrence BD (2018) Surgical site infections in spine surgery: preoperative prevention strategies to minimize risk. Glob Spine J 8(4 Suppl):31S–36S
Aleem IS, Tan LA, Nassr A, Riew KD (2020) Surgical site infection prevention following spine surgery. Glob Spine J 10(1 Suppl):92S–98S
Waly F, Alzahrani MM, Abduljabbar FH, Landry T, Ouellet J, Moran K et al (2015) The outcome of using closed suction wound drains in patients undergoing lumbar spine surgery: a systematic review. Glob Spine J 5(6):479–485
von Eckardstein KL, Dohmes JE, Rohde V (2016) Use of closed suction devices and other drains in spinal surgery: results of an online, Germany-wide questionnaire. Eur Spine J 25(3):708–715
Mirzai H, Eminoglu M, Orguc S (2006) Are drains useful for lumbar disc surgery? A prospective, randomized clinical study. J Spinal Disord Tech 19(3):171–177
Choi HS, Lee SG, Kim WK, Son S, Jeong TS (2016) Is surgical drain useful for lumbar disc surgery? Korean J Spine 13(1):20–23. https://doi.org/10.14245/kjs.2016.13.1.20
Adogwa O, Elsamadicy AA, Sergesketter AR et al (2018) Post-operative drain use in patients undergoing decompression and fusion: incidence of complications and symptomatic hematoma. J Spine Surg 4(2):220–226. https://doi.org/10.21037/jss.2018.05.09
Brown MD, Brookfield KFW (2004) A randomized study of closed wound suction drainage for extensive lumbar spine surgery. Spine 29(10):1066–1068
van Tulder M, Furlan A, Bombardier C, Bouter L, Editorial Board of the Cochrane Collaboration Back Review Group (2003) Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine 28:1290–1299
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. PLoS Med 6:e1000097
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S et al (2004) Grading quality of evidence and strength of recommendations. BMJ 328(7454):1490
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898
Sterne JAC, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ 355:4919. https://doi.org/10.1136/bmj.i4919
GRADEpro GDT: GRADEpro Guideline Development Tool [Software] (2015) McMaster University (developed by Evidence Prime, Inc.). www.gradepro.org. Accessed 15 Mar 2020
Suurmond R, van Rhee H, Hak T (2017) Introduction, comparison and validation of meta-essentials: a free and simple tool for meta-analysis. research synthesis methods. 8 4:537–553. https://doi.org/10.1002/jrsm.1260
Ovadia D, Drexler M, Kramer M, Herman A, Lebel DE (2019) Closed wound subfascial suction drainage in posterior fusion surgery for adolescent idiopathic scoliosis: a prospective randomized control study. Spine 44(6):377–383
Kogure K, Node Y, Tamaki T, Yamazaki M, Takumi I, Morita A (2015) Indwelling drains are not necessary for patients undergoing one-level anterior cervical fixation surgery. J Nippon Med Sch 82(3):124–129
Brazolino MAN, Jacob C Jr, Cardoso IM, Batista JL Jr, Maia TC, Debom TG et al (2017) Postoperative complications of suction drain in patients submitted to 1-level lumbar arthrodesis. Coluna/Columna 16:314–317
Gubin AV, Prudnikova OG, Subramanyam KN, Burtsev AV, Khomchenkov MV, Mundargi AV (2019) Role of closed drain after multi-level posterior spinal surgery in adults: a randomised open-label superiority trial. Eur Spine J 28(1):146–154
Payne DH, Fischgrund JS, Herkowitz HN, Barry RL, Kurz LT, Montgomery DM (1996) Efficacy of closed wound suction drainage after single-level lumbar laminectomy. J Spinal Disord 9(5):401–403
Hung P, Chang M, Chou P et al (2017) Is a drain tube necessary for minimally invasive lumbar spine fusion surgery? Eur Spine J 26:733–737. https://doi.org/10.1007/s00586-016-4672-4
Kumar V, Singh A, Waliullah S, Kumar D (2019) Analysis of efficacy in postoperative use of closed suction drain in cases of traumatic dorsolumbar spine injury. J Orthop Traumatol Rehabil 11:1–5
Blank J, Flynn JM, Bronson W, Ellman P, Pill SG, Lou JE et al (2003) The use of postoperative subcutaneous closed suction drainage after posterior spinal fusion in adolescents with idiopathic scoliosis. J Spinal Disord Tech 16(6):508–512
Gubin AV, Prudnikova OG, Burtsev AV, Khomchenkov MV, Kotel’nikov AO (2017) Role of postoperative wound drains in spinal surgery. Genij Ortopedii 23(2):180–186
Kotil K (2016) Closed drainage versus non-drainage for single-level lumbar disc surgery: relationship between epidural hematoma and fibrosis. Asian Spine J 10(6):1072–1078. https://doi.org/10.4184/asj.2016.10.6.1072
Sen O, Kizilkilic O, Aydin MV, Yalcin O, Erdogan B, Cekinmez M et al (2005) The role of closed-suction drainage in preventing epidural fibrosis and its correlation with a new grading system of epidural fibrosis on the basis of MRI. Eur Spine J 14(4):409–414
Kochai A, Erkorkmaz Ü (2019) The role of drains in adolescent idiopathic scoliosis surgery: is it necessary? Medicine 98(51):e18061
Diab M, Smucny M, Dormans JP, Erickson MA, Ibrahim K, Lenke LG et al (2012) Use and outcomes of wound drain in spinal fusion for adolescent idiopathic scoliosis. Spine 37(11):966–973
Poorman CE, Passias PG, Bianco KM, Boniello A, Yang S, Gerling MC (2014) Effectiveness of postoperative wound drains in one- and two-level cervical spine fusions. Int J Spine Surg 8:34. https://doi.org/10.14444/1034
Herrick DB, Tanenbaum JE, Mankarious M, Vallabh S, Fleischman E, Kurra S et al (2018) The relationship between surgical site drains and reoperation for wound-related complications following posterior cervical spine surgery: a multicenter retrospective study. J Neurosurg Spine 29(6):628–634
Kanayama M, Oha F, Togawa D, Shigenobu K, Hashimoto T (2010) Is closed-suction drainage necessary for single-level lumbar decompression? Review of 560 cases. Clin Orthop Relat Res 468(10):2690–2694
Walsh TL, Querry AM, McCool S, Galdys AL, Shutt KA, Saul MI et al (2017) Risk factors for surgical site infections following neurosurgical spinal fusion operations: a case control study. Infect Control Hosp Epidemiol 38(3):340–347
Walid MS, Abbara M, Tolaymat A, Davis JR, Waits KD, Robinson JS et al (2012) The role of drains in lumbar spine fusion. World Neurosurg 77(3):564–568
Sohn S, Chung CK, Kim CH (2013) Is closed-suction drainage necessary after intradural primary spinal cord tumor surgery? Eur Spine J 22(3):577–583. https://doi.org/10.1007/s00586-012-2504-8
Zhou J, Wang R, Huo X, Xiong W, Kang L, Xue Y (2020) Incidence of surgical site infection after spine surgery: a systematic review and meta-analysis. Spine 45(3):208–216
Deng H, Chan AK, Ammanuel SG, Chan AY, Oh T, Skrehot HC et al (2019) Risk factors for deep surgical site infection following thoracolumbar spinal surgery. J Neurosurg Spine 32(2):292–301
Davidoff CL, Rogers JM, Simons M, Davidson AS (2018) A systematic review and meta-analysis of wound drains in non-instrumented lumbar decompression surgery. J Clin Neurosci 53:55–61
Zijlmans JL, Buis DR, Verbaan D, Vandertop WP (2016) Wound drains in non-complex lumbar surgery: a systematic review. Bone Joint J 98-B(7):984–989
Parker MJ, Livingstone V, Clifton R, McKee A (2007) Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev 3:CD001825. https://doi.org/10.1002/14651858.cd001825.pub2
Yao R, Tan T, Tee JW, Street J (2018) Prophylaxis of surgical site infection in adult spine surgery: a systematic review. J Clin Neurosci 52:5–25
Liu J-M, Chen W-Z, Fu B-Q, Chen J-W, Liu Z-L, Huang S-H (2016) The use of closed suction drainage in lumbar spinal surgery: is it really necessary? World Neurosurg 90:109–115
Gerngross H, Engler V (1989) Schwerkraft- kontra Saugdrainage. Eine experimentelle und klinische Studie [Gravity drainage versus suction drainage: an experimental and clinical study]. Unfallchirurg 92(1):37–42
Patel SB, Griffiths-Jones W, Jones CS et al (2017) The current state of the evidence for the use of drains in spinal surgery: systematic review. Eur Spine J 26(11):2729–2738. https://doi.org/10.1007/s00586-017-4983-0
Fang Z, Tian R, Jia YT, Xu TT, Liu Y (2017) Treatment of cerebrospinal fluid leak after spine surgery. Chin J Traumatol 20(2):81–83. https://doi.org/10.1016/j.cjtee.2016.12.002
Al Jammal OM, Delavar A, Maguire KR, Hirshman BR, Wali AR, Kazzaz M et al (2019) National trends in the surgical management of lumbar spinal stenosis in adult spinal deformity patients. Spine 44(23):E1369–E1378
Tan T, Lee H, Huang MS, Rutges J, Marion TE, Mathew J et al (2020) Prophylactic postoperative measures to minimize surgical site infections in spine surgery: systematic review and evidence summary. Spine J. 20(3):435–447
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Muthu, S., Ramakrishnan, E., Natarajan, K.K. et al. Risk–benefit analysis of wound drain usage in spine surgery: a systematic review and meta-analysis with evidence summary. Eur Spine J 29, 2111–2128 (2020). https://doi.org/10.1007/s00586-020-06540-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06540-2