Abstract
Purpose
Objective functional tests like the five-repetition sit-to-stand test (5R-STS) can supplement an objective dimension to conventional patient-reported outcome measures. The reliability of unsupervised obtainment of 5R-STS performance is currently unknown.
Methods
We included patients with degenerative pathologies of the lumbar spine. Patients performed the 5R-STS during the initial clinical visit (supervised), as well as at home after instruction by a physiotherapist. At home, patients were first timed by a relative (unsupervised) and subsequently produced a video recording of themselves performing the 5R-STS for digital measurement (telesupervised). Two raters independently assessed the recordings.
Results
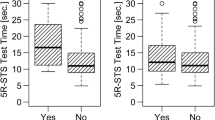
One hundred and twenty-one patients were recruited, of which 100 were eligible. Eighty-eight reported unsupervised results. Sixty-four returned recordings, of which 61 were ratable. Both unsupervised (r: 0.94, 95% CI 0.91–0.96, p < 0.001) and telesupervised (r: 0.90, 95% CI 0.83–0.94, p < 0.001) measurements demonstrated excellent correlation with clinical test times. Patients did not perform more slowly at home (p > 0.05). The interrater agreement for digital judgement of the telesupervised recording was excellent (ICC: 0.996, 95% CI 0.993–0.998, p < 0.001). We confirmed convergent validity with self-reported disability, back pain, and quality of life (all p < 0.05), but not with leg pain (p = 0.189).
Conclusions
Unsupervised at-home assessment using the 5R-STS is highly reliable. There does not appear to be a specific need for patients to return for a supervised 5R-STS follow-up. Rather, instructions can be provided, and the test performed and rated by a partner or family member at home. This is logistically and economically advantageous for patients, clinicians, and researchers.
Trial registry number
ClinicalTrials.gov Identifier: NCT03321357.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.






Similar content being viewed by others
References
Falavigna A, Dozza DC, Teles AR et al (2017) Current status of worldwide use of patient-reported outcome measures (PROMs) in spine care. World Neurosurg 108:328–335. https://doi.org/10.1016/j.wneu.2017.09.002
Deyo RAM, Battie M, Beurskens AJHM et al (1998) Outcome measures for low back pain research: a proposal for standardized use. Spine 23:2003–2013
Fairbank JC, Couper J, Davies JB, O’Brien JP (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66:271–273
Roland M, Morris R (1983) A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine 8:141–144
Rabin R, de Charro F (2001) EQ-5D: a measure of health status from the EuroQol Group. Ann Med 33:337–343
Prinsen CAC, Mokkink LB, Bouter LM et al (2018) COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res 27:1147–1157. https://doi.org/10.1007/s11136-018-1798-3
Guzman JZ, Cutler HS, Connolly J et al (2016) Patient-reported outcome instruments in spine surgery. Spine 41:429–437. https://doi.org/10.1097/BRS.0000000000001211
Parai C, Hägg O, Lind B, Brisby H (2018) The value of patient global assessment in lumbar spine surgery: an evaluation based on more than 90,000 patients. Eur Spine J 27:554–563. https://doi.org/10.1007/s00586-017-5331-0
Algattas H, Cohen J, Agarwal N, Hamilton DK (2017) Trends in the use of patient-reported outcome instruments in neurosurgical adult thoracolumbar deformity and degenerative disease literature. J Craniovertebral Junction Spine 8:103–107. https://doi.org/10.4103/jcvjs.JCVJS_29_17
Ostelo RWJG, Deyo RA, Stratford P et al (2008) Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine 33:90–94. https://doi.org/10.1097/BRS.0b013e31815e3a10
Gautschi OP, Corniola MV, Schaller K et al (2014) The need for an objective outcome measurement in spine surgery—the timed-up-and-go test. Spine J 14:2521–2522. https://doi.org/10.1016/j.spinee.2014.05.004
Guyatt GH, Sullivan MJ, Thompson PJ et al (1985) The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J 132:919–923
Mobbs RJ, Phan K, Maharaj M, Rao PJ (2016) Physical activity measured with accelerometer and self-rated disability in lumbar spine surgery: a prospective study. Glob Spine J 6:459–464. https://doi.org/10.1055/s-0035-1565259
Staartjes VE, Schröder ML (2018) The five-repetition sit-to-stand test: evaluation of a simple and objective tool for the assessment of degenerative pathologies of the lumbar spine. J Neurosurg Spine 29:380–387. https://doi.org/10.3171/2018.2.SPINE171416
Moke L, Severijns P, Schelfaut S et al (2018) Performance on balance evaluation systems test (BESTest) impacts health-related quality of life in adult spinal deformity patients. Spine 43:637. https://doi.org/10.1097/BRS.0000000000002390
Haddas R, Lieberman IH, Block A (2018) The relationship between fear-avoidance and objective biomechanical measures of function in patients with adult degenerative scoliosis. Spine 43:647. https://doi.org/10.1097/BRS.0000000000002381
Ferguson SA, Marras WS, Burr DL et al (2009) Quantification of a meaningful change in low back functional impairment. Spine 34:2060. https://doi.org/10.1097/BRS.0b013e3181b34764
Gautschi OP, Smoll NR, Corniola MV et al (2016) Validity and reliability of a measurement of objective functional impairment in lumbar degenerative disc disease: the timed up and go (TUG) test. Neurosurgery 79:270–278. https://doi.org/10.1227/NEU.0000000000001195
Regterschot GRH, Zhang W, Baldus H et al (2014) Test–retest reliability of sensor-based sit-to-stand measures in young and older adults. Gait Posture 40:220–224. https://doi.org/10.1016/j.gaitpost.2014.03.193
Ejupi A, Brodie M, Gschwind YJ et al (2015) Kinect-based five-times-sit-to-stand test for clinical and in-home assessment of fall risk in older people. Gerontology 62:118–124. https://doi.org/10.1159/000381804
Joswig H, Stienen MN, Smoll NR et al (2017) Patients’ preference of the timed up and go test or patient-reported outcome measures before and after surgery for lumbar degenerative disk disease. World Neurosurg 99:26–30. https://doi.org/10.1016/j.wneu.2016.11.039
Jones SE, Kon SSC, Canavan JL et al (2013) The five-repetition sit-to-stand test as a functional outcome measure in COPD. Thorax 68:1015–1020. https://doi.org/10.1136/thoraxjnl-2013-203576
Duncan RP, Leddy AL, Earhart GM (2011) Five times sit to stand test performance in Parkinson disease. Arch Phys Med Rehabil 92:1431–1436. https://doi.org/10.1016/j.apmr.2011.04.008
Simmonds MJ, Olson SL, Jones S et al (1998) Psychometric characteristics and clinical usefulness of physical performance tests in patients with low back pain. Spine 23:2412–2421
Mokkink LB, Terwee CB, Patrick DL et al (2010) The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol 63:737–745. https://doi.org/10.1016/j.jclinepi.2010.02.006
Von Elm E, Altman DG, Egger M et al (2007) Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335:806–808. https://doi.org/10.1136/bmj.39335.541782.AD
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Core Team R (2018) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Stienen MN, Smoll NR, Joswig H et al (2017) Validation of the baseline severity stratification of objective functional impairment in lumbar degenerative disc disease. J Neurosurg Spine. https://doi.org/10.3171/2016.11.SPINE16683
Shum GLK, Crosbie J, Lee RYW (2007) Three-dimensional kinetics of the lumbar spine and hips in low back pain patients during sit-to-stand and stand-to-sit. Spine 32:E211–E219. https://doi.org/10.1097/01.brs.0000259204.05598.10
Shum GLK, Crosbie J, Lee RYW (2005) Effect of low back pain on the kinematics and joint coordination of the lumbar spine and hip during sit-to-stand and stand-to-sit. Spine 30:1998–2004
Gautschi OP, Joswig H, Corniola MV et al (2016) Pre- and postoperative correlation of patient-reported outcome measures with standardized timed up and go (TUG) test results in lumbar degenerative disc disease. Acta Neurochir (Wien) 158:1875–1881. https://doi.org/10.1007/s00701-016-2899-9
Gautschi OP, Stienen MN, Corniola MV et al (2016) Assessment of the minimum clinically important difference in the timed up and go test after surgery for lumbar degenerative disc disease. Neurosurgery. https://doi.org/10.1227/NEU.0000000000001320
Acknowledgements
We thank Marlies P. de Wispelaere, MSc, for her efforts in clinical informatics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the article and its content were composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Staartjes, V.E., Beusekamp, F. & Schröder, M.L. Can objective functional impairment in lumbar degenerative disease be reliably assessed at home using the five-repetition sit-to-stand test? A prospective study. Eur Spine J 28, 665–673 (2019). https://doi.org/10.1007/s00586-019-05897-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-05897-3