Abstract
Purpose
To evaluate short- and intermediate-term effects of kinematic training (KT) using virtual reality (VR) or laser in patients with chronic neck pain.
Methods
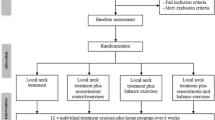
A randomised controlled trial with three arms (laser, VR, control) to post-intervention (N = 90), and two arms (laser or VR) continuing to 3 months follow-up. Home training intervention was provided during 4 weeks to VR and laser groups while control group waited.
Outcome measures
Primary outcome measures included neck disability index (NDI), global perceived effect (GPE), and cervical motion velocity (mean and peak). Secondary outcome measures included pain intensity (VAS), health status (EQ5D), kinesiophobia (TSK), range, smoothness, and accuracy of neck motion as measured by the neck VR system. Measures were taken at baseline, immediately post-training, and 3 months later.
Results
Ninety patients with neck pain were randomised to the trial, of which 76 completed 1 month follow-up, and 56 the 3 months follow-up. Significant improvements were demonstrated in NDI and velocity with good effect sizes in intervention groups compared to control. No within-group changes were presented in the control group, compared to global improvements in intervention groups. Velocity significantly improved at both time points in both groups. NDI, VAS, EQ5D, TSK and accuracy significantly improved at both time points in VR and in laser at 3 months evaluation in all but TSK. GPE scores showed 74–84% of participants perceived improvement and/or were satisfied. Significant advantages to the VR group compared to laser were found in velocity, pain intensity, health status and accuracy at both time points.
Conclusion
The results support home kinematic training using VR or laser for improving disability, neck pain and kinematics in the short and intermediate term with an advantage to the VR group. The results provide directions for future research, use and development.
Trial registration
ACTRN12615000231549.





Similar content being viewed by others
References
Lidgren L (2008) Preface: neck pain and the decade of the bone and joint 2000–2010. Spine 33:S1–S2
Hogg-Johnson S, van der Velde G, Carroll LJ, Holm LW, Cassidy JD, Guzman J, Cote P, Haldeman S, Ammendolia C, Carragee E, Hurwitz E, Nordin M, Peloso P (2008) The burden and determinants of neck pain in the general population: results of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Spine 33:S39–S51
Borghouts JA, Koes BW, Bouter LM (1998) The clinical course and prognostic factors of non-specific neck pain: a systematic review. Pain 77:1–13
Gross A, Kay TM, Paquin JP, Blanchette S, Lalonde P, Christie T, Dupont G, Graham N, Burnie SJ, Gelley G, Goldsmith CH, Forget M, Hoving JL, Brønfort G, Santaguida PL (2015) Exercises for mechanical neck disorders. Cochrane Libr. doi:10.1002/14651858.CD004250.pub5
Sarig Bahat H, Chen X, Reznik D, Kodesh E, Treleaven J (2015) Interactive cervical motion kinematics: sensitivity, specificity and clinically significant values for identifying kinematic impairments in patients with chronic neck pain. Man Ther 20:295–302. doi:10.1016/j.math.2014.10.002
Woodhouse A, Liljeback P, Vasseljen O (2010) Reduced head steadiness in whiplash compared with non-traumatic neck pain. J Rehabil Med 42:35–41. doi:10.2340/16501977-0484
Woodhouse A, Vasseljen O (2008) Altered motor control patterns in whiplash and chronic neck pain. BMC Musculoskelet Disord 9:90
Kristjansson E, Treleaven J (2009) Sensorimotor function and dizziness in neck pain: implications for assessment and management. J Orthop Sports Phys Ther 39:364–377
Sjolander P, Michaelson P, Jaric S, Djupsjobacka M (2008) Sensorimotor disturbances in chronic neck pain-range of motion, peak velocity, smoothness of movement, and repositioning acuity. Man Ther 13:122–131
Sarig Bahat H, Weiss PL, Laufer Y (2010) The effect of neck pain on cervical kinematics, as assessed in a virtual environment. Arch Phys Med Rehabil 91:1884–1890
Takasaki H, Treleaven J, Johnston V, Jull G (2013) Contributions of physical and cognitive impairments to self-reported driving difficulty in chronic whiplash-associated disorders. Spine 38:1554–1560
Röijezon U, Björklund M, Bergenheim M, Djupsjöbacka M (2008) A novel method for neck coordination exercise—a pilot study on persons with chronic non-specific neck pain. J Neuroeng Rehabil 5:36. doi:10.1186/1743-0003-5-36
Sullivan MJ, Adams H, Rhodenizer T, Stanish WD (2006) A psychosocial risk factor—targeted intervention for the prevention of chronic pain and disability following whiplash injury. Phys Ther 86:8–18
Sarig Bahat H, Takasaki H, Chen X, Bet-Or Y, Treleaven J (2015) Cervical kinematic training with and without interactive VR training for chronic neck pain—a randomized clinical trial. Man Ther 20:68–78. doi:10.1016/j.math.2014.06.008
Sveistrup H, Thornton M, Bryanton C, McComas J, Marshall S, Finestone H, McCormick A, McLean J, Brien M, Lajoie Y, Bisson Y (2004) Outcomes of intervention programs using flat screen virtual reality. In: Proceedings of the 26th annual international conference of IEEE/EMBS
Bahat HS, Chen X, Reznik D, Kodesh E, Treleaven J (2015) Interactive cervical motion kinematics: sensitivity, specificity and clinically significant values for identifying kinematic impairments in patients with chronic neck pain. Man Ther 20:295–302
Vernon H (2008) The Neck Disability Index: state-of-the-art, 1991–2008. J Manip Physiol Ther 31:491–502
Cleland JA, Childs JD, Whitman JM (2008) Psychometric Properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil 89:69
Hoving JL, O’Leary EF, Niere KR, Green S, Buchbinder R (2003) Validity of the Neck Disability Index, Northwick Park Neck Pain Questionnaire, and problem elicitation technique for measuring disability associated with whiplash-associated disorders. Pain 102:273–281
Pietrobon R, Coeytaux RR, Carey TS, Richardson WJ, DeVellis RF (2002) Standard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic review. Spine (Phila Pa 1976) 27:515–522
Pool JJ, Ostelo RW, Hoving JL, Bouter LM, de Vet HC (2007) Minimal clinically important change of the Neck Disability Index and the Numerical Rating Scale for patients with neck pain. Spine (Phila Pa 1976) 32:3047–3051. doi:10.1097/BRS.0b013e31815cf75b
Evans R, Bronfort G, Maiers M, Schulz C, Hartvigsen J (2014) “I know it’s changed”: a mixed-methods study of the meaning of global perceived effect in chronic neck pain patients. Eur Spine J 23:888–897. doi:10.1007/s00586-013-3149-y
Hurwitz EL, Morgenstern H, Vassilaki M, Chiang L-M (2004) Adverse reactions to chiropractic treatment and their effects on satisfaction and clinical outcomes among patients enrolled in the UCLA Neck Pain Study. J Manip Physiol Ther 27:16
Cleland J, Childs J, Fritz J, Whitman J (2006) Interrater reliability of the history and physical examination in patients with mechanical neck pain. Arch Phys Med Rehabil 87:1388–1395
Group TE (1990) EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Brooks R, Group E (1996) EuroQol: the current state of play. Health Policy 37:53–72
Soer R, Reneman MF, Speijer BLGN, Coppes MH, Vroomen PCAJ (2012) Clinimetric properties of the EuroQol-5D in patients with chronic low back pain. Spine J 12:1035–1039. doi:10.1016/j.spinee.2012.10.030
Kori S, Miller R, Todd D (1990) Kinesiophobia: a new view of chronic pain behaviour. Pain Manag 3:35–43
Buitenhuis J, Jaspers JP, Fidler V (2006) Can kinesiophobia predict the duration of neck symptoms in acute whiplash? Clin J Pain 22:272–277. doi:10.1097/01.ajp.0000173180.54261.0a
Cleland JA, Fritz JM, Childs JD (2008) Psychometric properties of the Fear-Avoidance Beliefs Questionnaire and Tampa Scale of Kinesiophobia in patients with neck pain. Am J Phys Med Rehabil 87:109–117. doi:10.1097/PHM.0b013e31815b61f1
Vlaeyen JWS, Kole-Snijders AMJ, Rotteveel A et al (1995) The role of fear of movement/(re)injury in pain disability. J Occup Rehabil 5:235–252
Ostelo RW, Swinkels-Meewisse IJ, Vlaeyen JW, Knol DL, de Vet HC (2007) Assessing pain and pain-related fear in acute low back pain: what is the smallest detectable change? Int J Behav Med 14:242–248
Sarig Bahat H, Sprecher E, Sela I, Treleaven J (2016) Neck motion kinematics: an inter-tester reliability study using an interactive neck VR assessment in asymptomatic individuals. Eur Spine J 25:2139–2148. doi:10.1007/s00586-016-4388-5
Sarig Bahat H, Weiss PL, Laufer Y (2009) Cervical motion assessment using virtual reality. Spine 34:1018–1024
Audette I, Dumas JP, Cote JN, De Serres SJ (2010) Validity and between-day reliability of the cervical range of motion (CROM) device. J Orthop Sports Phys Ther 40:318–323. doi:10.2519/jospt.2010.3180
Cohen J (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates, Hillsdale
Cook RJ, Sackett DL (1995) The number needed to treat: a clinically useful measure of treatment effect. BMJ Br Med J 310:452
Tsang SMH, Szeto GPY, Lee RYW (2014) Altered spinal kinematics and muscle recruitment pattern of the cervical and thoracic spine in people with chronic neck pain during functional task. J Electromyogr Kinesiol 24:104–113. doi:10.1016/j.jelekin.2013.10.011
Rizzo A, Kim GJ (2005) A SWOT analysis of the field of virtual reality rehabilitation and therapy. Presence-Teleoper Virtual Environ 14:119–146
Yelvar GDY, Çırak Y, Dalkılınç M, Demir YP, Guner Z, Boydak A (2017) Is physiotherapy integrated virtual walking effective on pain, function, and kinesiophobia in patients with non-specific low-back pain? Randomised controlled trial. Eur Spine J 26:538–545
Thomas JS, France CR, Leitkam ST, Applegate ME, Pidcoe PE, Walkowski S (2016) Effects of real-world versus virtual environments on joint excursions in full-body reaching tasks. IEEE J Transl Eng Health Med 4:1–8
Villiger M, Bohli D, Kiper D, Pyk P, Spillmann J, Meilick B, Curt A, Hepp-Reymond M-C, Hotz-Boendermaker S, Eng K (2013) Virtual reality—augmented neurorehabilitation improves motor function and reduces neuropathic pain in patients with incomplete spinal cord injury. Neurorehabil Neural Repair 27:675–683
Zronek M, Sanker H, Newcomb J, Donaldson M (2016) The influence of home exercise programs for patients with non-specific or specific neck pain: a systematic review of the literature. J Man Manip Ther 24(2):62–73. doi:10.1179/2042618613Y.0000000047
Bertozzi L, Villafañe JH, Capra F, Reci M, Pillastrini P (2015) Effect of an exercise programme for the prevention of back and neck pain in poultry slaughterhouse workers. Occup Ther Int 22:36–42
Lauche R, Langhorst J, Dobos GJ, Cramer H (2013) Clinically meaningful differences in pain, disability and quality of life for chronic nonspecific neck pain—a reanalysis of 4 randomized controlled trials of cupping therapy. Complement Ther Med 21:342–347. doi:10.1016/j.ctim.2013.04.005
Carreon LY, Glassman SD, Campbell MJ, Anderson PA (2010) Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J 10:469–474. doi:10.1016/j.spinee.2010.02.007
Cleland JA, Childs JD, Whitman JM (2008) Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil 89:69–74. doi:10.1016/j.apmr.2007.08.126
Sarig Bahat H, Igbariya M, Quek J, Treleaven J (2016) Cervical kinematics of fast neck motion across age. J Nov Physiother 6:7
Childs JD, Cleland JA, Elliott JM, Teyhen DS, Wainner RS, Whitman JM, Sopky BJ, Godges JJ, Flynn TW (2008) Neck pain: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther 38:A1–A34
Chen J, Solinger AB, Poncet JF, Lantz CA (1999) Meta-analysis of normative cervical motion. Spine 24:1571–1578
Bryanton C, Bosse J, Brien M, McLean J, McCormick A, Sveistrup H (2006) Feasibility, motivation, and selective motor control: virtual reality compared to conventional home exercise in children with cerebral palsy. Cyberpsychol Behav 9:123–128
Yamato TP, Saragiotto BT, Maher C (2014) Therapeutic exercise for chronic non-specific neck pain. Br J Sports Med. doi:10.1136/bjsports-2014-093874 (published online first)
Miller J, Gross A, D’Sylva J, Burnie SJ, Goldsmith CH, Graham N, Haines T, Bronfort G, Hoving JL (2010) Manual therapy and exercise for neck pain: a systematic review. Man Ther 15:334–354
Revel M, Minguet M, Gergory P, Vaillant J, Manuel JL (1994) Changes in cervicocephalic kinesthesia after a proprioceptive rehabilitation program in patients with neck pain: a randomized controlled study. Arch Phys Med Rehabil 75:895–899
Rudolfsson T, Djupsjöbacka M, Häger C, Björklund M (2014) Effects of neck coordination exercise on sensorimotor function in chronic neck pain: a randomized controlled trial. J Rehabil Med 46:908–914
Hurwitz E, Carragee E, van der Velde G, Carroll L, Nordin M, Guzman J, Peloso P, Holm L, Cote P, Hogg-Johnson S (2008) Treatment of neck pain: noninvasive interventions: results of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Spine (Phila Pa 1976) 33:S123–S152
Evans R, Bronfort G, Nelson B, Goldsmith CH (2002) Two-year follow-up of a randomized clinical trial of spinal manipulation and two types of exercise for patients with chronic neck pain. Spine 27:2383–2389
Ludvigsson ML, Peterson G, O’Leary S, Dedering Å, Peolsson A (2015) The effect of neck-specific exercise with, or without a behavioral approach, on pain, disability, and self-efficacy in chronic whiplash-associated disorders: a randomized clinical trial. Clin J Pain 31:294
Falla D, Hodges PW (2017) Individualized exercise interventions for spinal pain. Exerc Sport Sci Rev 45:105–115
Fewtrell MS, Kennedy K, Singhal A, Martin RM, Ness A, Hadders-Algra M, Koletzko B, Lucas A (2008) How much loss to follow-up is acceptable in long-term randomised trials and prospective studies? Arch Dis Child 93:458–461
Kristman V, Manno M, Côté P (2004) Loss to follow-up in cohort studies: how much is too much? Eur J Epidemiol 19:751–760
Acknowledgements
This work was funded by the Physiotherapy Research Fellowships (HMR), provided by Queensland Health, Health and Medical Research, Preventive Health Unit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding was supported by Queensland Government (2013003214).
Ethics approval
This study was approved by the Human Medical Research Ethics Committee, University of Queensland, and registered by the Australian New Zealand Clinical Trials Registry—trial registration ACTRN12615000231549.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Sarig Bahat, H., Croft, K., Carter, C. et al. Remote kinematic training for patients with chronic neck pain: a randomised controlled trial. Eur Spine J 27, 1309–1323 (2018). https://doi.org/10.1007/s00586-017-5323-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5323-0