Abstract
Background
The Swiss Federal Office of Public Health demanded a nationwide HTA-registry for cervical total disc arthroplasty (TDA), to decide about its reimbursement. The goal of the SWISSspine registry is to generate evidence about the safety and efficiency of cervical TDA.
Materials and methods
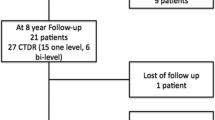
Three hundred thirty-two cases treated between 3.2005 and 6.2006 who were eligible for 5 years follow-ups were included in the study. Follow-up rates for 3–6 months, 1, 2 and 5 years were 84.6, 74.4, 50.6 and 64.8 %, respectively. Outcome measures were neck and arm pain, medication, quality of life, intraoperative and postoperative complication and revision rates. In addition, segmental mobility, ossification, adjacent and distant segment degeneration were analyzed at the 5-year follow-up.
Results
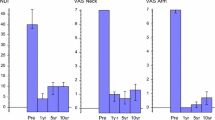
There was significant, clinically relevant and lasting reduction of neck (preop/postop 60/21 VAS points) and arm pain (preop/postop VAS 67/17) and a consequently decreased analgesics consumption and quality of life improvement (preop/postop 0.39/0.82 EQ-5D points) until the 5-year follow-up. The rates for intraoperative and early postoperative complications were 0.6 and 7.2 %, respectively. In 0.6 % an early and in 3.9 % a late revision surgery was performed. At the 5-year follow-up, the average range of motion of the mobile segments (88.2 %) was 10.2°. In 40.7 % of the patients osteophytes at least potentially affecting range of motion were seen.
Conclusions
Cervical TDA appeared as safe and efficient in long-term pain alleviation, consequent reduction of pain killer consumption and in improvement of quality of life. The improvement is stable over the 5 years postoperative period. The vast majority of treated segments remained mobile after 5 years, although 40.7 % of patients showed osteophytes.



Similar content being viewed by others
References
Resnick DK, Watters WC (2007) Lumbar disc arthroplasty: a critical review. Clin Neurosurg 54:83–87
Singh K, Vaccaro AR, Albert TJ (2004) Assessing the potential impact of total disc arthroplasty on surgeon practice patterns in North America. Spine J 4:195S–201S. doi:10.1016/j.spinee.2004.07.009
Richards O, Choi D, Timothy J (2012) Cervical arthroplasty: the beginning, the middle, the end? Br J Neurosurg 26:2–6. doi:10(3109/02688697).2011.595846
Denaro V, Papalia R, Denaro L, Di Martino A, Maffulli N (2009) Cervical spinal disc replacement. J Bone Jt Surg Br 91:713–719. doi:10.1302/0301-620X.91B6.22025
Goffin J, Van Calenbergh F, van Loon J, Casey A, Kehr P, Liebig K, Lind B, Logroscino C, Sgrambiglia R, Pointillart V (2003) Intermediate follow-up after treatment of degenerative disc disease with the Bryan Cervical Disc Prosthesis: single-level and bi-level. Spine (Phila Pa 1976) 28:2673–2678. doi:10.1097/01.BRS.0000099392.90849.AA
Beaurain J, Bernard P, Dufour T, Fuentes JM, Hovorka I, Huppert J, Steib JP, Vital JM, Aubourg L, Vila T (2009) Intermediate clinical and radiological results of cervical TDR (Mobi-C) with up to 2 years of follow-up. Eur Spine J 18:841–850. doi:10.1007/s00586-009-1017-6
Ahn PG, Kim KN, Moon SW, Kim KS (2009) Changes in cervical range of motion and sagittal alignment in early and late phases after total disc replacement: radiographic follow-up exceeding 2 years. J Neurosurg Spine 11:688–695. doi:10.3171/2009.7.SPINE0946
Coric D, Nunley PD, Guyer RD, Musante D, Carmody CN, Gordon CR, Lauryssen C, Ohnmeiss DD, Boltes MO (2011) Prospective, randomized, multicenter study of cervical arthroplasty: 269 patients from the Kineflex|C artificial disc investigational device exemption study with a minimum 2-year follow-up: clinical article. J Neurosurg Spine 15:348–358. doi:10.3171/2011.5.SPINE10769
Schluessmann E, Aghayev E, Staub L, Moulin P, Zweig T, Roder C, SWISSspine (2010) SWISSspine: The case of a governmentally required HTA-registry for total disc arthroplasty. Results of cervical disc prostheses. Spine (Phila Pa 1976) 35(24):E1397–1405
IEFO (2012) www.memdoc.org. University of Bern, Switzerland
McAfee PC, Cunningham BW, Devine J, Williams E, Yu-Yahiro J (2003) Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech 16:384–389
Upadhyaya CD, Wu JC, Trost G, Haid RW, Traynelis VC, Tay B, Coric D, Mummaneni PV (2012) Analysis of the three United States Food and Drug Administration investigational device exemption cervical arthroplasty trials. J Neurosurg Spine 16:216–228. doi:10.3171/2011.6.SPINE10623
Coric D, Cassis J, Carew JD, Boltes MO (2010) Prospective study of cervical arthroplasty in 98 patients involved in 1 of 3 separate investigational device exemption studies from a single investigational site with a minimum 2-year follow-up. Clin article. J Neurosurg Spine 13:715–721. doi:10.3171/2010.5.SPINE09852
Ren X, Wang W, Chu T, Wang J, Li C, Jiang T (2011) The intermediate clinical outcome and its limitations of Bryan cervical arthroplasty for treatment of cervical disc herniation. J Spinal Disord Tech 24:221–229. doi:10.1097/BSD.0b013e3181e9f309
Peng CW, Yue WM, Basit A, Guo CM, Tow BP, Chen JL, Nidu M, Yeo W, Tan SB (2011) Intermediate results of the prestige LP cervical disc replacement: clinical and radiological analysis with minimum two-year follow-up. Spine (Phila Pa 1976) 36:E105–E111. doi:10.1097/BRS.0b013e3181d76f99
Goffin J, van Loon J, Van Calenbergh F, Lipscomb B (2010) A clinical analysis of 4- and 6-year follow-up results after cervical disc replacement surgery using the Bryan cervical disc prosthesis. J Neurosurg Spine 12:261–269. doi:10.3171/2009.9.SPINE09129
Quan GM, Vital JM, Hansen S, Pointillart V (2011) Eight-year clinical and radiological follow-up of the Bryan cervical disc arthroplasty. Spine (Phila Pa 1976) 36:639–646. doi:10.1097/BRS.0b013e3181dc9b51
Chen J, Wang X, Bai W, Shen X, Yuan W (2012) Prevalence of heterotopic ossification after cervical total disc arthroplasty: a meta-analysis. Eur Spine J 21:674–680. doi:10.1007/s00586-011-2094-x
Mehren C, Suchomel P, Grochulla F, Barsa P, Sourkova P, Hradil J, Korge A, Mayer HM (2006) Heterotopic ossification in total cervical artificial disc replacement. Spine (Phila Pa 1976) 31:2802–2806. doi:10.1097/01.brs.0000245852.70594.d5
Leung C, Casey AT, Goffin J, Kehr P, Liebig K, Lind B, Logroscino C, Pointillart V (2005) Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial. Neurosurgery 57:759–763 (Discussion 759–763)
Lee JH, Jung TG, Kim HS, Jang JS, Lee SH (2010) Analysis of the incidence and clinical effect of the heterotopic ossification in a single-level cervical artificial disc replacement. Spine J 10:676–682. doi:10.1016/j.spinee.2010.04.017
Yi S, Kim KN, Yang MS, Yang JW, Kim H, Ha Y, do Yoon H, Shin HC (2010) Difference in occurrence of heterotopic ossification according to prosthesis type in the cervical artificial disc replacement. Spine (Phila Pa 1976) 35:1556–1561. doi:10.1097/BRS.0b013e3181c6526b
Suchomel P, Jurak L, Benes V 3rd, Brabec R, Bradac O, Elgawhary S (2010) Clinical results and development of heterotopic ossification in total cervical disc replacement during a 4-year follow-up. Eur Spine J 19:307–315. doi:10.1007/s00586-009-1259-3
Heidecke V, Burkert W, Brucke M, Rainov NG (2008) Intervertebral disc replacement for cervical degenerative disease—clinical results and functional outcome at two years in patients implanted with the Bryan cervical disc prosthesis. Acta neurochirurgica 150:453–459. doi:10.1007/s00701-008-1552-7 (Discussion 459)
Walraevens J, Demaerel P, Suetens P, Van Calenbergh F, van Loon J, Vander Sloten J, Goffin J (2010) Longitudinal prospective long-term radiographic follow-up after treatment of single-level cervical disk disease with the Bryan cervical disc. Neurosurgery 67:679–687. doi:10.1227/01.NEU.0000377039.89725.F3 (Discussion 687)
Kim HK, Kim MH, Cho DS, Kim SH (2009) Surgical outcome of cervical arthroplasty using bryan(r). J Korean Neurosurg Soc 46:532–537. doi:10.3340/jkns.2009.46.6.532
Wenger M, Hoonacker P, Zachee B, Lange R, Markwalder TM (2009) Bryan cervical disc prostheses: preservation of function over time. J Clin Neurosci 16:220–225. doi:10.1016/j.jocn.2008.01.021
Yu L, Song Y, Yang X, Lv C (2011) Systematic review and meta-analysis of randomized controlled trials: comparison of total disk replacement with anterior cervical decompression and fusion. Orthopedics 34:e651–e658. doi:10.3928/01477447-20110826-09
Mummaneni PV, Robinson JC, Haid RW Jr (2007) Cervical arthroplasty with the Prestige LP cervical disc. Neurosurgery 60:310–314. doi:10.1227/01.NEU.0000255376.42099.13 (Discussion 314–315)
Murrey D, Janssen M, Delamarter R, Goldstein J, Zigler J, Tay B, Darden B (2009) Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J 9:275–286. doi:10.1016/j.spinee.2008.05.006
Anderson PA, Sasso RC, Riew KD (2008) Comparison of adverse events between the Bryan artificial cervical disc and anterior cervical arthrodesis. Spine (Phila Pa 1976) 33:1305–1312. doi:10.1097/BRS.0b013e31817329a1
Jiang H, Zhu Z, Qiu Y, Qian B, Qiu X, Ji M (2012) Cervical disc arthroplasty versus fusion for single-level symptomatic cervical disc disease: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 132:141–151. doi:10.1007/s00402-011-1401-7
Barrey C, Campana S, Persohn S, Perrin G, Skalli W (2012) Cervical disc prosthesis versus arthrodesis using one-level, hybrid and two-level constructs: an in vitro investigation. Eur Spine J 21:432–442. doi:10.1007/s00586-011-1974-4
Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, Van Calenbergh F, van Loon J (2004) Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech 17:79–85
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Jt Surg Am 81:519–528
Nunley PD, Jawahar A, Kerr EJ 3rd, Gordon CJ, Cavanaugh DA, Birdsong EM, Stocks M, Danielson G (2012) Factors affecting the incidence of symptomatic adjacent-level disease in cervical spine after total disc arthroplasty: 2- to 4-year follow-up of 3 prospective randomized trials. Spine (Phila Pa 1976) 37:445–451. doi:10.1097/BRS.0b013e31822174b3
Yang B, Li H, Zhang T, He X, Xu S (2012) The incidence of adjacent segment degeneration after cervical disc arthroplasty (CDA): a meta analysis of randomized controlled trials. PLoS One 7:e35032. doi:10.1371/journal.pone.0035032
Aghayev E, Henning J, Munting E, Diel P, Moulin P, Roder C, Swissspine, Spine Tango Registry groups (2012) Comparative effectiveness research across two spine registries. Eur Spine J 21:1640–1647. doi:10.1007/s00586-012-2256-5
Aghayev E, Roder C, Zweig T, Etter C, Schwarzenbach O (2010) Benchmarking in the SWISSspine Registry: results of 52 dynardi lumbar total disc replacements compared with the data pool of 431 other lumbar disc prostheses. Eur Spine J 19(12):2190–2199. doi:10.1007/s00586-010-1550-3
Acknowledgments
The authors are thankful to the SWISSspine registry group who made this research possible by populating the database with their valuable and much appreciated entries. Among others, the data of following colleagues were used in the study: Bärlocher C (n = 45), Sgier F (n = 40), Hasdemir M (n = 21), Etter C (n = 14), Markwalder T (n = 14), Favre J (n = 12), Ramadan A (n = 12), Wernli F (n = 12), Maestretti G (n = 10), Porchet F (n = 10), Baur M (n = 9), Cathrein P (n = 8), Hausmann O (n = 8), Grob D (n = 8), Otten P (n = 8), Tessitore E (n = 8), Heimberger K (n = 7), Bothmann M (n = 6), Ebeling U (n = 5), Scheufler KM (n = 5), Uehlinger K (n = 5), Aebi M (n = 4), Boos N (n = 4), Hamburger C (n = 4), Kast E (n = 4), Schaeren S (n = 4), Forster T (n = 3), Hora J (n = 3), Min K (n = 3), Morard M (n = 3), Moulin P (n = 3), Stoll TM (n = 3), Steinsiepe F (n = 3), Berlemann U (n = 2), Boscherini D (n = 2), Heini P (n = 2), Kraus U (n = 2), Marchesi D (n = 2), Martinez R (n = 2), Oberle J (n = 2), Renella R (n = 2), Schwarzenbach O (n = 2), Bartanusz V (n = 1), Binggeli R (n = 1), Bongioanni F (n = 1), Jeanneret B (n = 1), Kroeber M (n = 1), Schianchi P (n = 1). Funded by the AO Foundation start-up-grant S-10-41A.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the SWISSspine Registry Group.
Rights and permissions
About this article
Cite this article
Aghayev, E., Bärlocher, C., Sgier, F. et al. Five-year results of cervical disc prostheses in the SWISSspine registry. Eur Spine J 22, 1723–1730 (2013). https://doi.org/10.1007/s00586-013-2770-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2770-0