Abstract
Purpose
The association between intraoperative hypotension and perioperative acute ischemic stroke is not well described. We hypothesized that intraoperative hypotension would be associated with perioperative acute ischemic stroke.
Methods
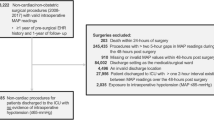
Four-year retrospective cohort study of elective non-cardiovascular, non-neurological surgical patients. Characteristics of patients who had perioperative acute ischemic stroke were compared against those of patients who did not have acute ischemic stroke. Multivariable logistic regression was used to determine whether hypotension was independently associated with increased odds of perioperative acute ischemic stroke.
Results
Thirty-four of 9816 patients (0.3%) who met study inclusion criteria had perioperative acute ischemic stroke. Stroke patients were older and had more comorbidities including hypertension, coronary artery disease, diabetes mellitus, active tobacco use, chronic obstructive pulmonary disease, cerebral vascular disease, atrial fibrillation, and peripheral vascular disease (all P < 0.05). MAP < 65 mmHg was not associated with increased odds of acute ischemic stroke when modeled as a continuous or categorical variable. MAP < 60 mmHg for more than 20 min was independently associated with increased odds of acute ischemic stroke, OR = 2.67 [95% CI = 1.21 to 5.88, P = 0.02].
Conclusion
Our analysis suggests that when MAP is less than 60 mmHg for more than 20 min, there is increased odds of acute ischemic stroke. Further studies are needed to determine what MAP should be targeted during surgery to optimize cerebral perfusion and limit ischemic stroke risk.

Similar content being viewed by others
References
Mashour GA, Shanks AM, Kheterpal S. Perioperative stroke and associated mortality after noncardiac, nonneurologic surgery. Anesthesiology. 2011;114:1289–96.
Bateman BT, Schumacher HC, Wang S, Shaefi S, Berman MF. Perioperative acute ischemic stroke in noncardiac and nonvascular surgery: incidence, risk factors, and outcomes. Anesthesiology. 2009;110:231–8.
Al-Hader R, Al-Robaidi K, Jovin T, Jadhav A, Wechsler LR, Thirumala PD. The incidence of perioperative stroke: estimate using state and national databases and systematic review. J Stroke. 2019;21:290–301.
Neuro VI. Perioperative covert stroke in patients undergoing non-cardiac surgery (NeuroVISION): a prospective cohort study. Lancet. 2019;394:1022–9.
Ahuja S, Mascha EJ, Yang D, Maheshwari K, Cohen B, Khanna AK, Ruetzler K, Turan A, Sessler DI. Associations of intraoperative radial arterial systolic, diastolic, mean, and pulse pressures with myocardial and acute kidney injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology. 2020;132:291–306.
Salmasi V, Maheshwari K, Yang D, Mascha EJ, Singh A, Sessler DI, Kurz A. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology. 2017;126:47–65.
Haller G, Bampoe S, Cook T, Fleisher LA, Grocott MPW, Neuman M, Story D, Myles PS, St EPCG. Systematic review and consensus definitions for the standardised endpoints in perioperative medicine initiative: clinical indicators. Br J Anaesth. 2019;123:228–37.
Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, Elkind MS, George MG, Hamdan AD, Higashida RT, Hoh BL, Janis LS, Kase CS, Kleindorfer DO, Lee JM, Moseley ME, Peterson ED, Turan TN, Valderrama AL, Vinters HV, American Heart Association Stroke Council CoCS, Anesthesia, Council on Cardiovascular R, Intervention, Council on C, Stroke N, Council on E, Prevention, Council on Peripheral Vascular D, Council on Nutrition PA, Metabolism. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064–89.
Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18:800–4.
Wesselink EM, Kappen TH, Torn HM, Slooter AJC, van Klei WA. Intraoperative hypotension and the risk of postoperative adverse outcomes: a systematic review. Br J Anaesth. 2018;121:706–21.
Bijker JB, Persoon S, Peelen LM, Moons KG, Kalkman CJ, Kappelle LJ, van Klei WA. Intraoperative hypotension and perioperative ischemic stroke after general surgery: a nested case-control study. Anesthesiology. 2012;116:658–64.
Sabate S, Mases A, Guilera N, Canet J, Castillo J, Orrego C, Sabate A, Fita G, Parramon F, Paniagua P, Rodriguez A, Sabate M, Group A. Incidence and predictors of major perioperative adverse cardiac and cerebrovascular events in non-cardiac surgery. Br J Anaesth. 2011;107:879–90.
Gregory A, Stapelfeldt WH, Khanna AK, Smischney NJ, Boero IJ, Chen Q, Stevens M, Shaw AD. Intraoperative hypotension is associated with adverse clinical outcomes after noncardiac surgery. Anesth Analg. 2020. https://doi.org/10.1213/ANE.0000000000005250 (Online ahead of print. PMID: 33177322).
Drummond JC. Blood pressure and the brain: how low can you go? Anesth Analg. 2019;128:759–71.
Joshi B, Ono M, Brown C, Brady K, Easley RB, Yenokyan G, Gottesman RF, Hogue CW. Predicting the limits of cerebral autoregulation during cardiopulmonary bypass. Anesth Analg. 2012;114:503–10.
Brady KM, Hudson A, Hood R, DeCaria B, Lewis C, Hogue CW. Personalizing the definition of hypotension to protect the brain. Anesthesiology. 2020;132:170–9.
Mathis MR, Naik BI, Freundlich RE, Shanks AM, Heung M, Kim M, Burns ML, Colquhoun DA, Rangrass G, Janda A, Engoren MC, Saager L, Tremper KK, Kheterpal S, Aziz MF, Coffman T, Durieux ME, Levy WJ, Schonberger RB, Soto R, Wilczak J, Berman MF, Berris J, Biggs DA, Coles P, Craft RM, Cummings KC, Ellis TA 2nd, Fleishut PM, Helsten DL, Jameson LC, van Klei WA, Kooij F, LaGorio J, Lins S, Miller SA, Molina S, Nair B, Paganelli WC, Peterson W, Tom S, Wanderer JP, Wedeven C, Multicenter Perioperative Outcomes Group I. Preoperative risk and the association between hypotension and postoperative acute kidney injury. Anesthesiology. 2020;132:461–75.
Haubrich C, Wendt A, Diehl RR, Klotzsch C. Dynamic autoregulation testing in the posterior cerebral artery. Stroke. 2004;35:848–52.
Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, Pessin MS, Lamy C, Mas JL, Caplan LR. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334:494–500.
Pierik R, Uyttenboogaart M, Erasmus ME, Scheeren TWL, van den Bergh WM. Distribution of perioperative stroke in cardiac surgery. Eur J Neurol. 2019;26:184–90.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Mazzeffi, M., Chow, J.H., Anders, M. et al. Intraoperative hypotension and perioperative acute ischemic stroke in patients having major elective non-cardiovascular non-neurological surgery. J Anesth 35, 246–253 (2021). https://doi.org/10.1007/s00540-021-02901-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-021-02901-3