Abstract
Background
Noninvasive biomarkers of intestinal inflammation can reduce the number of endoscopies in children with inflammatory bowel disease (IBD). This study aimed to prospectively investigate the usefulness of fecal calprotectin (FCP) and fecal immunochemical test (FIT) in pediatric IBD.
Methods
Patients aged 6–17 years who underwent ileocolonoscopy for established or suspected IBD were eligible for this study. Fecal samples for FCP and FIT were collected before colonoscopy.
Results
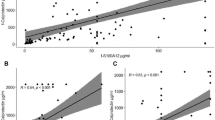
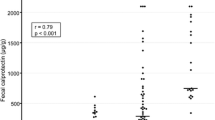
A total of 251 samples were analyzed: 88 from ulcerative colitis (UC), 74 from Crohn’s disease (CD), 75 from healthy controls (HC), and 14 from children with functional gastrointestinal disorders and normal colonoscopy (NC). At IBD diagnosis, both FCP and FIT were significantly higher in the newly diagnosed UC/CD group than in the HC/NC group (P < 0.001). The optimal cutoffs of FCP and FIT to predict IBD diagnosis were 217 mg/kg and 87 ng/mL, respectively. Patients without mucosal healing (MH) showed higher FCP and FIT than those with MH in both UC and CD (P < 0.001). The FCP increased exponentially as the endoscopic activity score increased. The optimal cutoff values of FCP and FIT for predicting MH were 161 mg/kg and 106 ng/mL for UC and 367 mg/kg and 57 ng/mL for CD, respectively. FCP showed better specificity than the FIT. Patients with CD and normal ileocolonoscopy had elevated FCP during active small intestinal inflammation.
Conclusions
Both FCP and FIT correlate well with endoscopic activity in pediatric patients with IBD. The FCP is a superior marker for predicting MH.




Similar content being viewed by others
References
Roseth AG, Schmidt PN, Fagerhol MK. Correlation between faecal excretion of indium-111-labelled granulocytes and calprotectin, a granulocyte marker protein, in patients with inflammatory bowel disease. Scand J Gastroenterol. 1999;34:50–4.
Oliva S, Thomson M, de Ridder L, et al. Endoscopy in pediatric inflammatory bowel disease: a position paper on behalf of the porto ibd group of the european society for pediatric gastroenterology, hepatology and nutrition. J Pediatr Gastroenterol Nutr. 2018;67:414–30.
Mamula P, Markowitz JE, Neiswender K, et al. Success rate and duration of paediatric outpatient colonoscopy. Dig Liver Dis. 2005;37:877–81.
Tibble JA, Sigthorsson G, Foster R, et al. Use of surrogate markers of inflammation and Rome criteria to distinguish organic from nonorganic intestinal disease. Gastroenterology. 2002;123:450–60.
Burri E, Beglinger C, von Felten S, et al. Fecal calprotectin and the clinical activity index are both useful to monitor medical treatment in patients with ulcerative colitis. Dig Dis Sci. 2015;60:485–91.
Schoepfer AM, Beglinger C, Straumann A, et al. Fecal calprotectin more accurately reflects endoscopic activity of ulcerative colitis than the Lichtiger Index, C-reactive protein, platelets, hemoglobin, and blood leukocytes. Inflamm Bowel Dis. 2013;19:332–41.
D’Haens G, Ferrante M, Vermeire S, et al. Fecal calprotectin is a surrogate marker for endoscopic lesions in inflammatory bowel disease. Inflamm Bowel Dis. 2012;18:2218–24.
Sipponen T, Savilahti E, Kolho KL, et al. Crohn’s disease activity assessed by fecal calprotectin and lactoferrin: correlation with Crohn’s disease activity index and endoscopic findings. Inflamm Bowel Dis. 2008;14:40–6.
Sipponen T, Kolho KL. Fecal calprotectin in diagnosis and clinical assessment of inflammatory bowel disease. Scand J Gastroenterol. 2015;50:74–80.
Mooiweer E, Fidder HH, Siersema PD, et al. Fecal hemoglobin and calprotectin are equally effective in identifying patients with inflammatory bowel disease with active endoscopic inflammation. Inflamm Bowel Dis. 2014;20:307–14.
Takashima S, Kato J, Hiraoka S, et al. Evaluation of mucosal healing in ulcerative colitis by fecal calprotectin vs. fecal immunochemical test. Am J Gastroenterol. 2015;110:873–80.
Henderson P, Anderson NH, Wilson DC. The diagnostic accuracy of fecal calprotectin during the investigation of suspected pediatric inflammatory bowel disease: a systematic review and meta-analysis. Am J Gastroenterol. 2014;109:637–45.
Kittanakom S, Shajib MS, Garvie K, et al. Comparison of fecal calprotectin methods for predicting relapse of pediatric inflammatory bowel disease. Can J Gastroenterol Hepatol. 2017;2017:1450970.
Oyaert M, Boel A, Jacobs J, et al. Analytical performance and diagnostic accuracy of six different faecal calprotectin assays in inflammatory bowel disease. Clin Chem Lab Med (CCLM). 2017. https://doi.org/10.1515/cclm-2016-1012.
Levine A, Koletzko S, Turner D, et al. ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr. 2014;58:795–806.
Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987;317:1625–9.
Lobaton T, Bessissow T, De Hertogh G, et al. The modified mayo endoscopic score (MMES): a new index for the assessment of extension and severity of endoscopic activity in ulcerative colitis patients. J Crohns Colitis. 2015;9:846–52.
Turner D, Hyams J, Markowitz J, et al. Appraisal of the pediatric ulcerative colitis activity index (PUCAI). Inflamm Bowel Dis. 2009;15:1218–23.
Daperno M, D’Haens G, Van Assche G, et al. Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: the SES-CD. Gastrointest Endosc. 2004;60:505–12.
Gralnek IM, Defranchis R, Seidman E, et al. Development of a capsule endoscopy scoring index for small bowel mucosal inflammatory change. Aliment Pharmacol Ther. 2008;27:146–54.
Cotter J, de Dias Castro F, Magalhaes J, et al. Validation of the Lewis score for the evaluation of small-bowel Crohn’s disease activity. Endoscopy. 2015;47:330–5.
Turner D, Griffiths AM, Walters TD, et al. Mathematical weighting of the pediatric Crohn’s disease activity index (PCDAI) and comparison with its other short versions. Inflamm Bowel Dis. 2012;18:55–62.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Ryu DG, Kim HW, Park SB, et al. Clinical implications of fecal calprotectin and fecal immunochemical test on mucosal status in patients with ulcerative colitis. Medicine (Baltimore). 2019;98:e17080.
Canani RB, Terrin G, Rapacciuolo L, et al. Faecal calprotectin as reliable non-invasive marker to assess the severity of mucosal inflammation in children with inflammatory bowel disease. Dig Liver Dis. 2008;40:547–53.
Hiraoka S, Inokuchi T, Nakarai A, et al. Fecal immunochemical test and fecal calprotectin results show different profiles in disease monitoring for ulcerative colitis. Gut Liver. 2018;12:142–8.
Dai C, Jiang M, Sun MJ, et al. Fecal immunochemical test for predicting mucosal healing in ulcerative colitis patients: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2018;33:990–7.
Naganuma M, Kobayashi T, Nasuno M, et al. Significance of conducting 2 types of fecal tests in patients with ulcerative colitis. Clin Gastroenterol Hepatol. 2020;18:1102-1111 e5.
Ryu DG, Kim HW, Park SB, et al. Assessment of disease activity by fecal immunochemical test in ulcerative colitis. World J Gastroenterol. 2016;22:10617–24.
van Rheenen PF, Aloi M, Assa A, et al. The medical management of paediatric Crohn’s disease: an ECCO-ESPGHAN guideline update. J Crohns Colitis. 2020. https://doi.org/10.1093/ecco-jcc/jjaa161.
Schoepfer AM, Beglinger C, Straumann A, et al. Fecal calprotectin correlates more closely with the simple endoscopic score for Crohn’s disease (SES-CD) than CRP, blood leukocytes, and the CDAI. Am J Gastroenterol. 2010;105:162–9.
Sipponen T, Karkkainen P, Savilahti E, et al. Correlation of faecal calprotectin and lactoferrin with an endoscopic score for Crohn’s disease and histological findings. Aliment Pharmacol Ther. 2008;28:1221–9.
Jones J, Loftus EV Jr, Panaccione R, et al. Relationships between disease activity and serum and fecal biomarkers in patients with Crohn’s disease. Clin Gastroenterol Hepatol. 2008;6:1218–24.
Weinstein-Nakar I, Focht G, Church P, et al. associations among mucosal and transmural healing and fecal level of calprotectin in children with Crohn’s disease. Clin Gastroenterol Hepatol. 2018;16:1089-1097 e4.
Arai T, Takeuchi K, Miyamura M, et al. Level of fecal calprotectin correlates with severity of small bowel Crohn’s disease, measured by balloon-assisted enteroscopy and computed tomography enterography. Clin Gastroenterol Hepatol. 2017;15:56–62.
Acknowledgements
We express our sincere gratitude to Dr. Sachiko Nishina (Division of Ophthalmology, National Center for Child Health and Development, Tokyo, Japan) for their valuable assistance in collecting fecal samples. We would like to thank Editage (www.editage.com) for English language editing.
Funding
This work was supported, in part, by a Grant-in-Aid from the National Center for Child Health and Development from the Ministry of Health, Labour and Welfare of Japan (No. 2019A-3), by Health and Labour Sciences Research Grants for studies on intractable diseases from the Ministry of Health, Labour and Welfare of Japan (No. 20FC1037), and by a research grant from Nippon Kayaku in stool bacterial cultures. Thermo Fisher Scientific also supported this study for fecal calprotectin measurements.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hiroshi Nakase has received support from AbbVie GK., Kissei Pharmaceutical Co., Ltd., Kyorin Pharmaceutical Co.,Ltd., Mitsubishi Tanabe Pharma Corporation, Janssen Pharmaceutical K.K, Takeda Pharmaceutical Co.,Ltd., Pfizer Inc, Celgene Corporation., EA Pharma Co.,Ltd., Zeria Pharmaceutical CO.,Ltd., Mochida Pharmaceutical Co.,Ltd., Nippon Kayaku Co.,Ltd., Daiichi Sankyo Company, Limited., JIMRO Co.,Ltd., as well as grants for commissioned/joint research from Hoya Group Pentax Medical, Mitsubishi Tanabe Pharma Corporation, Pfizer Inc, AbbVie GK., Mochida Pharmaceutical Co.,Ltd. Katsuhiro Arai received honoraria for consulting and lecture from EA Pharma Co., Ltd., Mitsubishi Tanabe Pharma Corporation, and a research grant from AstraZeneca K.K. Toshiaki Shimizu is an endowed chair of Taiko Pharmaceutical and has received a research grant from the Food Science Institute Foundation and a scholarship grant from JCR Pharmaceuticals Co., Ltd. Other authors declare that they have no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shimizu, H., Ebana, R., Kudo, T. et al. Both fecal calprotectin and fecal immunochemical tests are useful in children with inflammatory bowel disease. J Gastroenterol 57, 344–356 (2022). https://doi.org/10.1007/s00535-022-01856-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-022-01856-w