Abstract
Purpose
To investigate the effect of two different types of music on anxiety, nausea, and satisfaction levels in cancer patients receiving chemotherapy (CT) for the first time.
Methods
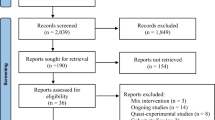
The study was conducted as a single-blind, pre-test, post-test, three-group randomized controlled trial in an outpatient CT unit between August 2022 and February 2023. A simple (computer-based) and stratified (age and gender) randomization method was used to assign 75 patients to the relaxing music group (RMG), Turkish classical music group (TCMG), and control group (CG) (n = 25 each). The primary outcome was the change in anxiety levels measured by Spielberger’s State Anxiety Inventory before (T0) and after (T1) CT session. Secondary outcomes were the change in the severity of nausea from T0 to T1 and the level of satisfaction at T1.
Results
The groups were similar in terms of baseline sociodemographic and health-related characteristics. Anxiety levels were lower than the baseline in RMG and TCMG in comparison to CG, and repeated measures analysis showed a significant group × time interaction (p = 0.001, F = 210.221, η2 = 0.745). Nausea severity increased from T0 to T1 for CG but decreased for RMG and TCMG with a significant group × time interaction (p = 0.001, F = 100.785, η2 = 0.583). The satisfaction level was significantly higher in TCMG than in CG and RMG (8.64 ± 0.95 vs. 7.88 ± 0.72, and 7.00 ± 0.70, respectively).
Conclusion
Music may be an effective non-pharmacologic option to relieve patients’ anxiety and nausea during first-time CT. Larger, multicenter studies evaluating the long-term effect of music are needed to confirm these findings.
Trial registration
clinicaltrials.gov (NCT05687838)/2022-13/18


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Siegel RL, Miller KD, Wagle NS, Jemal A (2023) Cancer statistics, 2023. CA Cancer J Clin 73(1):17–48. https://doi.org/10.3322/caac.21763
Kutluk T, Ahmed F, Cemaloğlu M et al (2021) Progress in palliative care for cancer in Turkey: a review of the literature. Ecancermedicalscience 15:1321. https://doi.org/10.3332/ecancer.2021.1321
Anand U, Dey A, Chandel AKS et al (2022) Cancer chemotherapy and beyond: current status, drug candidates, associated risks and progress in targeted therapeutics. Genes Dis 10(4):1367–1401. https://doi.org/10.1016/j.gendis.2022.02.007
Roe H, Lennan E (2014) Role of nurses in the assessment and management of chemotherapy-related side effects in cancer patients. Nursing: Res Rev 4:103–115. https://doi.org/10.2147/NRR.S41845
Debela DT, Muzazu SG, Heraro KD et al (2021) New approaches and procedures for cancer treatment: current perspectives. SAGE Open Med 9:20503121211034366. https://doi.org/10.1177/20503121211034366
Devlin EJ, Denson LA, Whitford HS (2017) Cancer treatment side effects: a meta-analysis of the relationship between response expectancies and experience. J Pain Symptom Manage 54(2):245–258.e2. https://doi.org/10.1016/j.jpainsymman.2017.03.017
Parás-Bravo P, Paz-Zulueta M, Boixadera-Planas E et al (2020) Cancer patients and anxiety: a gender perspective. Int J Environ Res Public Health 17(4):1302. https://doi.org/10.3390/ijerph17041302
Naser AY, Hameed AN, Mustafa N et al (2021) Depression and anxiety in patients with cancer: a cross-sectional study. Front Psychol 12:585534. https://doi.org/10.3389/fpsyg.2021.585534
Charalambous A, Giannakopoulou M, Bozas E, Paikousis L (2015) A randomized controlled trial for the effectiveness of progressive muscle relaxation and guided ımagery as anxiety reducing ınterventions in breast and prostate cancer patients undergoing chemotherapy. Evid Based Complement Alternat Med 2015:270876. https://doi.org/10.1155/2015/270876
Bakhiet TE, Ali SM, Bakhiet AM (2021) Prevalence of depression and anxiety among adult patients undergoing chemotherapy in Khartoum, Sudan: a cross-sectional study. J Affect Disord 6:100218. https://doi.org/10.1016/j.jadr.2021.100218
Pandey M, Sarita GP, Devi N, Thomas BC, Hussain BM, Krishnan R (2006) Distress, anxiety, and depression in cancer patients undergoing chemotherapy. World J Surg Oncol 4(68):26. https://doi.org/10.1186/1477-7819-4-68
Baqutayan SM (2012) The effect of anxiety on breast cancer patients. Indian J Psychol Med 34(2):119–123. https://doi.org/10.4103/0253-7176.101774
El Kheir DYM, Ibrahim AHM (2019) Epidemiological assessment of distress during chemotherapy: who is affected? J Taibah Univ Med Sci 14(5):448–453. https://doi.org/10.1016/j.jtumed.2019.08.004
Dadkhah B, Anisi E, Mozaffari N, Amani F, Pourghasemian M (2019) Effect of music therapy with periorbital massage on chemotherapy-ınduced nausea and vomiting ın gastrointestinal cancer: a randomized controlled trail. J Caring Sci 8(3):165–171. https://doi.org/10.15171/jcs.2019.02415
Lin MF, Hsieh YJ, Hsu YY, Fetzer S, Hsu MC (2011) A randomised controlled trial of the effect of music therapy and verbal relaxation on chemotherapy-induced anxiety. J Clin Nurs 20(7-8):988–999. https://doi.org/10.1111/j.1365-2702.2010.03525.x
Vichaya EG, Chiu GS, Krukowski K et al (2015) Mechanisms of chemotherapy-induced behavioral toxicities. Front Neurosci 9:131. https://doi.org/10.3389/fnins.2015.00131
Sakamoto R, Koyama A (2020) Effective therapy against severe anxiety caused by cancer: a case report and review of the literature. Cureus 12(6):e8414. https://doi.org/10.7759/cureus.8414
Traeger L, Greer JA, Fernandez-Robles C, Temel JS, Pirl WF (2012) Evidence-based treatment of anxiety in patients with cancer. J Clin Oncol 30(11):1197–1205. https://doi.org/10.1200/JCO.2011.39.5632
Forbes E, Baker AL, Britton B et al (2020) Non-pharmacological approaches to procedural anxiety reduction for patients undergoing radiotherapy for cancer: systematic review protocol. BMJ Open 10(10):e035155. https://doi.org/10.1136/bmjopen-2019-035155
Bradt J, Dileo C, Myers-Coffman K, Biondo J (2021) Music interventions for improving psychological and physical outcomes in people with cancer. Cochrane Database Syst Rev 10(10):CD006911. https://doi.org/10.1002/14651858.CD006911.pub4
Gupta A, Bhushan B, Behera L (2018) Short-term enhancement of cognitive functions and music: a three-channel model. Sci Rep 8(1):15528. https://doi.org/10.1038/s41598-018-33618-1
Wilkins RW, Hodges DA, Laurienti PJ, Steen M, Burdette JH (2014) Network science and the effects of music preference on functional brain connectivity: from Beethoven to Eminem. Sci Rep 4:6130. https://doi.org/10.1038/srep06130
Tang H, Chen L, Wang Y, Zhang Y, Yang N, Yang N (2021) The efficacy of music therapy to relieve pain, anxiety, and promote sleep quality, in patients with small cell lung cancer receiving platinum-based chemotherapy. Support Care Cancer 29(12):7299–7306. https://doi.org/10.1007/s00520-021-06152-6
Nguyen KT, Xiao J, Chan DNS, Zhang M, Chan CWH (2022) Effects of music intervention on anxiety, depression, and quality of life of cancer patients receiving chemotherapy: a systematic review and meta-analysis. Support Care Cancer 30(7):5615–5626. https://doi.org/10.1007/s00520-022-06881-2
Al-Jubouri MBA, Isam SR, Hussein SM, Machuca-Contreras F (2021) Recitation of quran and music to reduce chemotherapy-induced anxiety among adult patients with cancer: a clinical trial. Nurs Open 8(4):1606–1614. https://doi.org/10.1002/nop2.781
Singh A, Soni A, Saluja S (2013) Essentials of sample size calculation. Curr Med Res Pract 3:97–99 http://www.cmrpjournal.org/text.asp?2013/3/2/97/300688
Vieillard S, Gilet AL (2013) Age-related differences in affective responses to and memory for emotions conveyed by music: a cross-sectional study. Front Psychol 4:711. https://doi.org/10.3389/fpsyg.2013.00711
Feizpour A, Parkington HC, Mansouri FA (2020) Cognitive sex differences in effects of music in Wisconsin Card Sorting Test. Psychology of Music 48(2):252–265. https://doi.org/10.1177/0305735618795030
Garland T (2014) Self-regulation ınterventions and strategies: keeping the body, mind & emotions on task in children with autism, ADHD or sensory disorders. Pesi Publishing & Media, USA
O'Kelly J, James L, Palaniappan R, Taborin J, Fachner J, Magee WL (2013) Neurophysiological and behavioral responses to music therapy in vegetative and minimally conscious states. Front Hum Neurosci 7:884. https://doi.org/10.3389/fnhum.2013.00884
MusiCure (2005). Evidence based music and films by composer Niels Eje. https://musicure.dk/en/home Accessed 30 August 2022.
Bozkurt B, Ayangil R, Holzapfel A (2014) Computational analysis of Turkish makam music: review of state-of-the-art and challenges. J New Music Res 43(1):3–23. https://doi.org/10.1080/09298215.2013.865760
Yıldırım M (2021) Music healing: history, development, application in addictions and music therapy applications in Turkey. Turk Acad Res 6(2):477–497. https://doi.org/10.30622/tarr.935092
Spielberger CD (1983) Manual for the State-Trait Inventory STAI (Form Y). Mind Garden, Palo Alto, CA
Bakeman R (2005) Recommended effect size statistics for repeated measures designs. Behav Res Methods 37(3):379–384. https://doi.org/10.3758/BF03192707
Jagiello R, Pomper U, Yoneya M et al (2019) Rapid brain responses to familiar vs. unfamiliar music – an EEG and pupillometry study. Sci Rep 9:15570. https://doi.org/10.1038/s41598-019-51759-9
Meltzer B, Reichenbach CS, Braiman C, Schiff ND, Hudspeth AJ, Reichenbach T (2015) The steady-state response of the cerebral cortex to the beat of music reflects both the comprehension of music and attention. Front Hum Neurosci 9:436. https://doi.org/10.3389/fnhum.2015.00436
Kumagai Y, Arvaneh M, Tanaka T (2017) Familiarity affects entrainment of EEG in music listening. Front Hum Neurosci 11:384. https://doi.org/10.3389/fnhum.2017.00384
Abdolreza Gharehbagh Z, Mansourzadeh A, Montazeri Khadem A, Saeidi M (2022) Reflections on using open-ended questions. Med Educ Bull 3(2):475–482. https://doi.org/10.22034/meb.2022.333518.1054
Bradt J, Dileo C, Myers-Coffman K, Biondo J (2021) Music interventions for improving psychological and physical outcomes in people with cancer. Cochrane Database Syst Rev 10(10):CD006911. https://doi.org/10.1002/14651858.CD006911.pub4
Bro ML, Johansen C, Vuust P et al (2019) Effects of live music during chemotherapy in lymphoma patients: a randomized, controlled, multi-center trial. Support Care Cancer 27(10):3887–3896. https://doi.org/10.1007/s00520-019-04666-8
Coronado AC, Tran K, Chadder J et al (2017) The experience of patients with cancer during diagnosis and treatment planning: a descriptive study of Canadian survey results. Curr Oncol 24(5):332–337. https://doi.org/10.3747/co.24.3782
Derry HM, Epstein AS, Lichtenthal WG, Prigerson HG (2019) Emotions in the room: common emotional reactions to discussions of poor prognosis and tools to address them. Expert Rev Anticancer Ther 19(8):689–696. https://doi.org/10.1080/14737140.2019.1651648
Pasyar N, Rambod M, Zahedi F, Ramzi M (2022) Pain, fatigue, nausea, and vomiting as the predictors of anxiety in patients undergoing hematopoietic stem cell transplantation: a prospective cohort study. Support Care Cancer 30(7):5871–5879. https://doi.org/10.1007/s00520-022-06997-5
Roila F, Molassiotis A, Herrstedt J et al (2016) 2016 MASCC and ESMO guideline update for the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting and of nausea and vomiting in advanced cancer patients. Ann Oncol 27(suppl 5):v119–v133. https://doi.org/10.1093/annonc/mdw270
Acknowledgements
The authors thank the patients who agreed to participate in this study and the CT nurses who contributed to the implementation of the study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, intervention, and data collection were performed by ÖED and DAD. The full manuscript was written by ÖED, DAD, SP, and YY, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the Declaration of Helsinki. Ethics committee approval was obtained from the Clinical Research Ethics Committee at Bursa Uludağ University School of Medicine (Decision number: 2022-13/18); other required permissions were granted by the institution where the study was conducted. Before baseline measurements and group assignments were done, each participant was informed about the study, and written informed consent for participation was obtained. Participation was voluntary. Participants had the right to leave the study at any time without affecting their treatment or services in any way. Patients’ privacy was protected by ensuring anonymity and withholding personal information throughout the research process. The study protocol was registered on ClinicalTrails.gov (Registration number: NCT05687838).
Consent for publication
N/A.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dallı, Ö.E., Doğan, D.A., Pehlivan, S. et al. The effect of two different types of music played to cancer patients during chemotherapy on anxiety, nausea, and satisfaction levels. Support Care Cancer 31, 710 (2023). https://doi.org/10.1007/s00520-023-08165-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-08165-9