Abstract
Purpose
Oral cryotherapy is an effective method to prevent oral mucositis (OM) induced by chemotherapeutic agents, such as melphalan (Mel). However, there is limited data about cryotherapy in allogeneic hematopoietic stem cell transplantation (allo-HSCT) recipients; thus, the current study aimed to examine the efficacy of cryotherapy among allo-HSCT recipients treated with Mel-containing regimens.
Methods
Medical records of 78 consecutive allo-HSCT recipients were retrospectively analyzed. Baseline characteristics and clinical courses between the patients who received cryotherapy (cryotherapy group, n = 42) and those who did not (control group, n = 36) were compared, especially focusing on methotrexate (MTX) use as a part of graft-versus-host disease (GVHD) prophylaxis.
Results
Binary logistic regression analysis revealed that a higher dose of Mel (OR, 3.82; 95%CI, 1.085–13.46; P = 0.037) or MTX use (OR, 7.61; 95% CI, 2.41–23.97; P < 0.001) was associated with the incidence of OM. MTX use was also significantly associated with the duration of OM (β = 0.515; 95% CI, 9.712–21.636; P < 0.001). Among 31 patients without MTX use, cryotherapy was associated with a significant reduction of OM development (0% in the cryotherapy group vs 35% in the control group, P = 0.021). We did not find such an association in 47 patients with MTX use.
Conclusion
Cryotherapy was useful to prevent the incidence of OM in allo-HSCT recipients in the cases without MTX for GVHD prophylaxis.
Similar content being viewed by others
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is one the most powerful treatment options that can provide a cure for patients with hematological malignancies and inherited hematopoietic disorders [1, 2]. To ensure engraftment of infused donor cells, allo-HSCT recipients undergo intensive chemotherapy and/or total body irradiation (TBI), which eradicates not only residual malignant cells but also immunocompetent cells [2]. These procedures result in various complications in the oral cavity, including ulceration, gingivitis, infections, and oral mucositis (OM) [3], with the incidence of OM ranging from 60 to 100% [4, 5]. Regimen-related OM, which is dependent on the component drugs and intensity of conditioning regimens [6], may be associated with an impairment of systemic physical conditions (i.e., focal pain, malnutrition, increased risk of infection, decreased activities of daily living), change of treatment schedule [7], and prolonged hospitalization [8].
The reported risk factors for developing OM include high-dose melphalan (Mel), TBI, body mass index ≥ 25, and presence of methylenetetrahydrofolate reductase 677 TT genotype, which is involved in folic acid metabolism [9]. In addition, the use of methotrexate (MTX), which is commonly administered to allo-HSCT patients as graft-versus-host disease (GVHD) prophylaxis, was recognized as another risk factor [10]. Therefore, folic acid (Leucovorin®) is sometimes initiated after MTX dose to reduce OM (known as leucovorin rescue) [11, 12], based on its reported efficacy [13].
To manage OM, palifermin (recombinant keratinocyte growth factor-1) and low-energy laser have been used [14,15,16,17]. In fact, palifermin treatment is the effective way to reduce the severity and the duration of OM for the hematologic cancer patients received intensive chemotherapy and radiotherapy. Low-energy laser is proved effective for the prevention of OM and the treatment of pain in the hematopoietic stem cell transplantation patients. In addition, a practice guideline from the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) recommended cryotherapy for managing OM [18]. Cryotherapy, which involved cooling the buccal mucosa using ice, ice water, or ice cream, reduced the dispersion of chemotherapeutic agents into the circulation due to constriction of the blood vessels in the oral mucosa. Previous reports and a meta-analysis of randomized controlled trials have confirmed the efficacy of cryotherapy in preventing OM among patients who received high-dose Mel [19,20,21,22].
In this retrospective analysis, we explored the incidence and duration of OM among allo-HSCT recipients following Mel-containing preparative regimens as well as the impact of the concomitant use of MTX and prophylactic cryotherapy.
Materials and Methods
Study design, setting, and participants
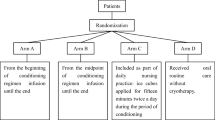
This pre–post study recruited 93 patients who underwent allo-HSCT following Mel-containing conditioning regimens at Kyushu University hospital from April 2014 to December 2018. Among them, 12 patients with insufficient data and 3 patients who had undergone multiple allo-HSCT were excluded; thus, the remaining 78 patients were eligible for OM assessment in this study.
Cryotherapy was introduced at our institute in June 2018 to prevent Mel-induced OM. We compared the baseline characteristics and clinical courses between patients who underwent treatment, including prophylactic cryotherapy after June 2018 (cryotherapy group, n = 42) and those who did not prophylactic cryotherapy before May 2018 (control group, n = 36). We retrospectively reviewed their medical records and collected the following information: age, sex, underlying diseases, conditioning regimen, TBI, graft source, Mel dose, MTX use, leucovorin rescue, number of teeth, usage of denture, and incidence and duration of OM. The primary objective of this study was to evaluate the protective effect of cryotherapy for OM in allo-HSCT recipients following Mel-containing preparative regimens with or without short-term MTX. This study was approved by the Kyushu University Institutional Review Board for Clinical Research (approval number: 2021–417).
Transplant procedures
All 78 patients received fludarabine/Mel-based conditioning regimens. In addition, patients either received 6.4–12.8 mg/kg of busulfan (n = 9), cytarabine (n = 18), cyclophosphamide (n = 1), anti-thymocyte globulin (n = 9), or 2 Gy (n = 38), 4 Gy (n = 18), and 12 Gy (n = 1) of TBI. Consequently, 5.13% (4/78) patients received myeloablative conditioning. Calcineurin inhibitors (cyclosporin or tacrolimus) were used as the backbone of GVHD prophylaxis; short-term MTX, mycophenolate mofetil, and methylprednisolone were administered in 47, 21, and 10 cases, respectively.
As bacterial prophylaxis, oral levofloxacin (500 mg/day) was generally administered from the beginning of the conditioning regimen to engraftment. Oral fluconazole or intravenous echinocandins (micafungin or caspofungin) and oral acyclovir were routinely given as prophylaxis for fungal infections and herpes simplex virus reactivation, respectively.
Evaluation of OM and intervention
By using the National Cancer Institute Common Toxicity Criteria (NCI-CTCAE) version (v) 3.0 (Table 1), the status of the oral mucosa was assessed everyday by the nurses and at least once a week by three dentists from the beginning of the conditioning regimen until engraftment or OM resolution. The duration of OM was defined as the time taken to progress from Grade 1 to Grade 3 according to NCI-CTCAE v3.0. Conventional oral care, including low-energy laser, was administered by dentists as needed.
Cryotherapy
Patients used ice cubes for cryotherapy. The ice cubes were contained in clean plastic cups. Patients could buy in the shop and stored in the freezer. Patients kept the ice cube in the mouth and spat the ice cube. They continued with this for a total of 90 min before and after Mel administration on 3 and 2 day before allo-HSCT.
Statistical analysis
Age, number of teeth, and duration of oral mucositis were examined using the student’s t-test. Fisher’s exact test was used to analyze sex, TBI, Mel dose, MTX use, leucovorin rescue, denture usage, and OM incidence. Pearson’s Chi-square test was conducted to compare the underlying diseases and graft source.
Odds ratios (ORs) for the incidence of OM were calculated using a binary logistic regression analysis. We added age (continuous), sex (0: man, 1: woman), Mel dose (0: 80 mg/m2, 1: 140 mg/m2), MTX (0: no, 1: yes), TBI (0: no, 1: yes), cryotherapy (0: no, 1: yes), and leucovorin rescue (0: no, 1: yes) as independent variables for the binomial logistic regression analysis.
In addition, a multiple regression analysis was performed to identify the factors associated with the duration of OM; the independent variables used were age (continuous), sex (0: man, 1: woman), Mel dose (0: 80 mg/m2, 1: 140 mg/m2), MTX (0: no, 1: yes), TBI (0: no, 1: yes), cryotherapy (0: no, 1: yes) and leucovorin rescue (0: no, 1: yes).
Furthermore, we performed a subgroup analysis that focused on the concomitant use of MTX. This study analyzed the relationship between the incidence and duration of OM and the effectiveness of cryotherapy by dividing the patients into two groups based on the usage of Methotrexate.
All analyses were performed using the SPSS software program (version 28.0, IBM Japan, Tokyo). Statistical significance was defined as a P value < 0.05.
Results
Characteristics of participants
As shown in Table 2, there was no difference in the patient characteristics between the cryotherapy group (n = 42) and control group (n = 36), except for the use of TBI (85.7% vs 58.3%, P = 0.007). Neutrophil engraftment was 18.4 ± 5.4 days in the cryotherapy group and 18.8 ± 5.4 days in the control group (P = 0.756).
Incidence of OM and its risk factors
The incidence of OM was 47.6% (20/42) in the cryotherapy group and 55.6% (20/36) in the control group. In the cryotherapy group, the maximum grade of OM was 1 in 4.76% patients, 2 in 11.9%, 3 in 31.0%, and 4 in 0%. Whereas, in the control group, the maximum grade of OM was 1 in 8.33% patients, 2 in 19.4%, 3 in 27.8%, and 4 in 0%. We calculated ORs for the incidence of OM using binary logistic regression analysis and disclosed that high-dose Mel (140 mg/m2) (OR, 3.82; 95% CI, 1.09–13.46; P = 0.037) and MTX use (OR, 7.61; 95% CI, 2.41–23.97; P < 0.001) were statistically significantly correlated with OM development (Table 3). The protective effect of cryotherapy was not evident.
Duration of OM and its risk factors
Next, we evaluated the duration of OM and its related factors. The median duration of OM was 7.0 days (range, 6.41–14.87 days) in the cryotherapy group and 7.0 days (range, 5.97–17.26 days) in the control group. Table 4 shows the risk factors of the duration of OM, as determined using the multiple regression analysis (R2 = 0.265). MTX use was significantly associated with the longer duration of OM (β = 0.515; 95%CI, 9.712–21.636; P < 0.001). Cryotherapy did not have impact on the duration of OM.
Subgroup analysis based on the MTX use
Since both Mel and MTX cause OM, and cryotherapy was adapted only for the duration of Mel administration, we further performed a subgroup analysis that focused on the concomitant use of MTX. Cryotherapy had a positive impact on OM prophylaxis in patients who were treated with Mel but not with MTX; no patient developed OM in the cryotherapy group (n = 14), whereas 6 out of 17 (35.3%) patients developed OM in the control group (P = 0.021) (Table 5). The cryotherapy group included a higher proportion of older patients with TBI use than the control group, indicating its robust efficacy in preventing OM in this cohort.
Among 47 patients who were treated with both Mel and MTX, 28 underwent prophylactic cryotherapy (Table 5). Leucovorin rescue was used for seven patients (25%) in the cryotherapy group and three patients (16%) in the control group (P = 0.718). The incidence of OM (20 of 28, 71% vs 14 of 19 74%, P = 0.865) and its duration (22.4 ± 11.0 days vs 26.2 ± 18.5 days, P = 0.451) were comparable between the two groups.
Discussion
Cryotherapy is reportedly effective in preventing severe OM in patients treated with cytotoxic agents, especially high-dose Mel [23,24,25,26], in the setting of auto-HSCT. In addition, some previous studies have revealed that cryotherapy significantly reduced the incidence of all-grade OM [27] or moderate-to-severe OM [22, 28] even in allo-HSCT recipients. However, the efficacy of cryotherapy among allo-HSCT recipients was still controversial, presumably due to the variety of conditioning regimens, graft sources, and immunosuppressants used for GVHD prophylaxis. Therefore, in the current study, we assessed the impact of cryotherapy on OM development in 78 patients receiving Mel-based conditioning followed by the first allo-HSCT. Ice cubes were applied to the oral mucosa of the patients for a total of 90 min (30 min before, 30 min during administration, and 30 min after Mel administration); however, the most optimal timing and duration of oral cryotherapy remain unclear. A previous study revealed that 60-min cryotherapy had similar efficacy to 120-min cryotherapy [29]. Therefore, the best method of oral cryotherapy should be explored to prevent OM using different conditions (i.e., timing of cryotherapy and time and/or materials of cooling). Although various scales for the assessment of the severity of OM were available [30, 31], we adopted the NCI-CTCAE v3.0. instead of the latest v5.0. The latter allowed non-specialists of oral care to evaluate OM more easily by using pain and oral intake but not objectively about the degree of mucosal damage. To avoid the differences in proficiency among evaluators may affect the results, professional dentists with similar skill levels were engaged in this study. This was reconfirmed by performing daily assessment by non-specialists.
In this study, we aimed to determine whether cryotherapy was effective in patients with OM. First, we considered the risk factors that had an influence on the incidence and duration of OM. These analyses revealed that MTX was the risk factor for the incidence and duration of OM, and Mel was the risk factor for the incidence of OM. MTX, an inhibitor of folic acid metabolism, has reportedly altered the diversity and components of the gut and/or oral microbiota [32,33,34] and also caused mucositis similar to folic acid deficiency [35]. Another previous report demonstrated that MTX-containing GVHD prophylaxis resulted in more severe and prolonged OM than the non-MTX sirolimus-based method by inhibiting the repair of oral mucosa [36]. Therefore, we performed an additional analysis based on the MTX use to clarify the efficacy of cryotherapy in a more homogenous subgroup. Notably, the preventive effect of cryotherapy against OM development was evident in allo-HSCT recipients without MTX use. Regarding the patients who received short-term MTX, a shorter duration of OM was noted in the cryotherapy group than that in the control group; however, this difference was not significant.
Therefore, a future study should investigate the hypothesis that cryotherapy at the time of MTX administration contributes to the reduction and/or shortening of severe OM, although a prospective randomized study subjected to patients with myeloablative conditioning has failed [37]. Besides cryotherapy, alternative treatment strategies, including leucovorin rescue [12, 13], low-energy laser [38], and palifermin [15, 16], have emerged for managing OM. A combined use of these options with cryotherapy might succeed in reducing OM development even in patients with both Mel-based conditioning and MTX-containing GVHD prophylaxis.
There are several limitations in this study. First, it had a pre–post design; thus, patients analyzed in each group received allo-HSCT at different times. Although baseline characteristics were almost comparable between the two groups, differences may have existed in supportive care (e.g., antibiotics and antifungal agents). Second, our study was a single-center retrospective analysis with a small number of Japanese patients. We evaluated OM by using common scale NCI-CTCAE v3.0. However, this study was a retrospective study and we could not investigate the reliability and validity before the target period. Thus, the results should be interpreted cautiously. Third, this is an unavoidable problem for a study with a pre–post design, future studies should conduct randomized control trials to determine the effectiveness of cryotherapy for OM. At last, this study did not adequately assess the impact of cryotherapy on subjective conditions, including oral pain and quality of life-based patients’ satisfaction.
Conclusion
This study revealed the usefulness of cryotherapy in preventing OM in allo-HSCT recipients without MTX use. Future randomized controlled studies with a larger number of patients are needed to confirm our findings.
Data availability
The data that support the findings of this study are available on request from the corresponding author, S.M.
References
Jenq RR, van den Brink MR (2010) Allogeneic hematopoietic stem cell transplantation: individualized stem cell and immune therapy of cancer. Nat Rev Cancer 10:213–221. https://doi.org/10.1038/nrc2804
Copelan EA, Chojecki A, Lazarus HM, Avalos BR (2019) Allogeneic hematopoietic cell transplantation; the current renaissance. Blood Rev 34:34–44. https://doi.org/10.1016/j.blre.2018.11.001
Bollero P, Passarelli PC, D'Addona A, Pasquantonio G, Mancini M, Condò R, Cerroni L (2018) Oral management of adult patients undergoing hematopoietic stem cell transplantation. Eur Rev Med Pharmacol Sci 22:876–887. https://doi.org/10.26355/eurrev_201802_14365
Chaudhy HM, Bruce AJ, Wolf RC, Litzow MR, Hogan WJ, Patnaik MS, Kremers WK, Phillips GL, Hashmi SK (2016) The incidence and severity of oral mucositis among allogeneic hematopoietic stem cell transplantation patients: a systematic review. Biol Blood Marrow Transplant 22:605–616. https://doi.org/10.1016/j.bbmt.2015.09.014
Shouval R, Kouniavski E, Fein J, Danylesko I, Shem-Tov N, Geva M, Yerushalmi R, Shimoni A, Nagler A (2019) Risk factors and implications of oral mucositis in recipients of allogeneic hematopoietic stem cell transplantation. Eur J Haematol 103:402–409. https://doi.org/10.1111/ejh.13299
Valeh M, Kargar M, Mansouri A, Kamranzadeh H, Gholami K, Heidari K, Hajibabaei M (2018) Factors affecting the incidence and severity of oral mucositis following hematopoietic stem cell transplantation. Int J Hematol Oncol Stem Cell Res 12:142–152
Patel P, Robinson PD, Baggott C, Gibson P, Ljungman G, Massey N, Ottaviani G, Phillips R, Revon-Rivière G, Treister N, White M, Cabral S, Dupuis L, Sung L (2021) Clinical practice guideline for the prevention of oral and oropharyngeal mucositis in pediatric cancer and hematopoietic stem cell transplant patients: 2021 update. Eur J Cancer 154:92–101. https://doi.org/10.1016/j.ejca.2021.05.013
Elting LS, Cooksley C, Chambers M, Cantor SB, Manzullo E, Rubenstein EB (2003) The burdens of cancer therapy. Clinical and economic outcomes of chemotherapy-induced mucositis. Cancer 98:1531–1539. https://doi.org/10.1002/cncr.11671
Robien K, Schubert MM, Bruemmer B, Lloid ME, Potter JD, Ulrich CM (2004) Predictors of oral mucositis in patients receiving hematopoietic cell transplants for chronic myelogenous leukemia. J Clin Oncol 22:1268–1275. https://doi.org/10.1200/JCO.2004.05.147
Valer JB, Curra M, Gabriel AF, Schmidt TR, Ferreira MBC, Roesler R, Evangelista JMC, Martins MAT, Gregianin L, Martins MD (2021) Oral mucositis in childhood cancer patients receiving high-dose methotrexate: prevalence, relationship with other toxicities and methotrexate elimination. Int J Paediatr Dent 31:238–246. https://doi.org/10.1111/ipd.12718
Oosterom N, de Jonge R, Smith DEC, Pieters R, Tissing WJ E, Fiocco M, van Zelst BD, van den Heuvel-Eibrink MM, Heil SG. (2019) Changes in intracellular folate metabolism during high-dose methotrexate and leucovorin rescue therapy in children with acute lymphoblastic leukemia. PLoS One 14: e0221591. https://doi.org/10.1371/journal.pone.0221591
AlJohani NI (2021) Role of folinic acid in methotrexate-based prophylaxis of graft-versus-host disease following hematopoietic stem cell transplantation. Hematology 26:620–627. https://doi.org/10.1080/16078454.2021.1966222
Sugita J, Matushita T, Kashiwazaki H, Kosugi M, Takahashi S, Wakasa K, Shiratori S, Ibata M, Shono Y, Shigematsu A, Obara M, Fujimoto K, Endo T, Nishino M, Kondo T, Hashino S, Tanaka J, Asaka M, Imamura M (2012) Efficacy of folinic acid in preventing oral mucositis in allogeneic hematopoietic stem cell transplant patients receiving MTX as prophylaxis for GVHD. Bone Marrow Transplant 47:258–264. https://doi.org/10.1038/bmt.2011.53
Brennan MT, Hasséus B, Hovan AJ, Raber-Durlacher JE, Blijlevens NM, Huysmans MC, Garming Legert K, Johansson JE, Moore CG, von Bültzingslöwen I (2018) Impact of oral side effects from conditioning therapy before hematopoietic stem cell transplantation: protocol for a multicenter study. JMIR Res Protoc 7:e103. https://doi.org/10.2196/resprot.8982
Blijlevens N, Sonis S (2006) Palifermin (recombinant keratinocyte growth factor-1):a pleiotropic growth factor with multiple biological activities in preventing chemotherapy- and radiotherapy-induced mucositis. Ann Oncol 18:817–826. https://doi.org/10.1093/annonc/mdl332
Spielberger R, Stiff P, Bensinger W, Gentile T, Weisdorf D, Kewalramani T, Shea T, Yanovich S, Hansen K, Noga S, McCarty J, LeMaistre CF, Sung EC, Blazar BR, Elhardt D, Chen MG, Emmanouilides C (2004) Palifermin for oral mucositis after intensive therapy for hematologic cancers. N Engl J Med 351:2590–2598. https://doi.org/10.1056/NEJMoa040125
Zadik Y, Arany PR, Fregnani ER, Bossi P, Antunes HS, Bensadoun RJ, Gueiros LA, Majorana A, Nair RG, Ranna V, Tissing WJE, Vaddi A, Lubart R, Migliorati CA, Lalla RV, Cheng KKF, Elad S; Mucositis Study Group of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) (2019) Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer 27:3969-3983. https://doi.org/10.1007/s00520-019-04890-2
Elad S, Cheng KKF, Lalla RV, Yarom N, Hong C, Logan RM, Bowen J, Gibson R, Saunders DP, Zadik Y, Ariyawardana A, Correa ME, Ranna V, Bossi P; Mucositis Guidelines Leadership Group of the Multinational Association of Supportive Care in Cancer and International Society of Oral Oncology (MASCC/ISOO) (2020) MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 126:4423-4431.https://doi.org/10.1002/cncr.33100
Lilleby K, Garcia P, Gooley T, McDonnnell P, Taber R, Holmberg L, Maloney DG, Press OW, Bensinger W (2006) A prospective, randomized study of cryotherapy during administration of high-dose melphalan to decrease the severity and duration of oral mucositis in patients with multiple myeloma undergoing autologous peripheral blood stem cell transplantation. Bone Marrow Transplant 37:1031–1035. https://doi.org/10.1038/sj.bmt.1705384
Lu Y, Zhu X, Ma Q, Wang J, Jiang P, Teng S, Zhou L, Wu D, Wang H (2020) Oral cryotherapy for oral mucositis management in patients receiving allogeneic hematopoietic stem cell transplantation: a prospective randomized study. Support Care Cancer 28:1747–1754. https://doi.org/10.1007/s00520-019-04966-z
Peterson DE, Ohrn K, Bowen J, Fliedner M, Lees J, Loprinzi C, Mori T, Osaguona A, Weikel DS, Elad S, Lalla RV; Mucositis Study Group of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) (2013) Systematic review of oral cryotherapy for management of oral mucositis caused by cancer therapy. Support Care Cancer 21:327-332.https://doi.org/10.1007/s00520-012-1562-0
Wang L, Gu Z, Zhai R, Zhao S, Luo L, Li D, Zhao X, Wei H, Pang Z, Wang L, Liu D, Wang Q, Gao C (2015) Efficacy of oral cryotherapy on oral mucositis prevention in patients with hematological malignancies undergoing hematopoietic stem cell transplantation: a meta-analysis of randomized controlled trials. PLoS One 10: e0128763. https://doi.org/10.1371/journal.pone.0128763. eCollection 2015
Marchesi F, Tendas A, Giannarelli D, Viggiani C, Gumenyuk S, Renzi D, Franceschini L, Caffarella G, Rizzo M, Palombi F, Pisani F, Romano A, Spadea A, Papa E, Canfora M, Pignatelli A, Cantonetti M, Arcese W, Mengarelli A (2017) Cryotherapy reduces oral mucositis and febrile episodes in myeloma patients treated with high-dose melphalan and autologous stem cell transplant: a prospective, randomized study. Bone Marrow Transplant 52:154–156. https://doi.org/10.1038/bmt.2016.207
Askarifar M, Lakdizaji S, Ramzi M, Rahmani A, Jabbarzadeh F (2016) The effects of oral cryotherapy on chemotherapy-induced oral mucositis in patients undergoing autologous transplantation of blood stem cells: a clinical trial. Iran Red Crescent Med J 18:e24775. https://doi.org/10.5812/ircmj.24775. eCollection 2016 Apr
Salvador P, Azusano C, Wang L, Howell D (2012) A pilot randomized controlled trial of an oral care intervention to reduce mucositis severity in stem cell transplant patients. J Pain Symptom Manage 44:64–73. https://doi.org/10.1016/j.jpainsymman.2011.08.012
Svanberg A, Ohrn K, Birgegård G (2010) Oral cryotherapy reduces mucositis and improves nutrition-a randomized controlled trial. J Clin Nurs 19:2146–2151. https://doi.org/10.1111/j.1365-2702.2010.03255.x
Vokurka S, Svoboda T, Jungova A, Karas M, Koza V (2012) Oral cryotherapy can significantly reduce oral mucositis but not acute GVHD incidence in Flu/Mel conditioning allo-SCT. Bone Marrow Transplant 47:739–741. https://doi.org/10.1038/bmt.2011.156
Aisa Y, Mori T, Kudo M, Yashima T, Kondo S, Yokoyama A, Ikeda Y, Okamoto S (2005) Oral cryotherapy for the prevention of high-dose melphalan-induced stomatitis in allogeneic hematopoietic stem cell transplant recipients. Support Care Cancer 13:266–269. https://doi.org/10.1007/s00520-004-0726-y
Mori T, Yamazaki R, Aisa Y, Nakazato T, Kudo M, Yashima T, Kondo S, Ikeda Y, Okamoto S (2006) Brief oral cryotherapy for the prevention of high-dose melphalan-induced stomatitis in allogeneic hematopoietic stem cell transplant recipients. Support Care Cancer 14:392–395. https://doi.org/10.1007/s00520-005-0016-3
Quinn B, Potting CM, Stone R, Blijlevens NM, Fliedner M, Margulies A, Sharp L (2008) Guidelines for the assessment of oral mucositis in adult chemotherapy, radiotherapy and hematopoietic stem cell transplant patients. Eur J Cancer 44:61–72. https://doi.org/10.1016/j.ejca.2007.09.014
Baysal E, Sari D (2019) Effects of cryotherapy in preventing oral mucositis in hematopoietic stem cell transplantation patients: literature review. Complement Ther Clin Pract 35:342–347. https://doi.org/10.1016/j.ctcp.2019.03.017
Zhang X, Zhang X, Zhang D, Jia H, Feng Q, Wang D, Liang D, Wu X, Li J, Tang L, Li Y, Lan Z, Chen B, Li Y, Zhong H, Xie H, Jie Z, Chen W, Tang S, Xu X, Wang X, Cai X, Liu S, Xia Y, Li J, Qiao X, Al-Aama JY, Chen H, Wang L, Wu QJ, Zhang F, Zheng W, Li Y, Zhang M, Luo G, Xue W, Xiao L, Li J, Chen W, Xu X, Yin Y, Yang H, Wang J, Kristiansen K, Liu L, Li T, Huang Q, Li Y, Wang J (2015) The oral and gut microbiomes are perturbed in rheumatoid arthritis and partly normalized after treatment. Nat Med 21:895–905. https://doi.org/10.1038/nm.3914
Zhou B, Xia X, Wang P, Chen S, Yu C, Huang R, Zhang R, Wang Y, Lu L, Yuan F, Tian Y, Fan Y, Zhang X, Shu Y, Zhang S, Bai D, Wu L, Xu H, Yang L (2018) Induction and amelioration of methotrexate-induced gastrointestinal toxicity are related to immune response and gut microbiota. EBioMedicine 33:122–133. https://doi.org/10.1016/j.ebiom.2018.06.029
Van der Beek JN, Oosterom N, Pieters R, de Jonge R, van den Heuvel-Eibrink MM, Heil SG (2019) The effect of leucovorin rescue therapy on methotrexate-induced oral mucositis in the treatment of paediatric ALL: a systematic review. Crit Rev Oncol Hematol 142:1–8. https://doi.org/10.1016/j.critrevonc.2019.07.003
Shea B, Swinden MV, Ghogomu ET, Ortiz Z, Katchamart W, Rader T, Bombardier C, Wells GA, Tugwell P (2014) Folic and acid folinic acid for reducing side effects in patients receiving methotrexate for rheumatoid arthritis. J Rheumatol 41:1049–1060. https://doi.org/10.3899/jrheum.130738
Cutler C, Li S, Kim HT, Laglenne P, Szeto KC, Hoffmeister L, Harrison MJ, Ho V, Alyea E, Lee SJ, Soiffer R, Sonis S, Antin JH (2005) Mucositis after allogeneic hematopoietic stem cell transplantation: a cohort study of methotrexate- and non-methotrexate-containing graft-versus-host disease prophylaxis regimens. Biol Blood Marrow Transplant 11:383–388. https://doi.org/10.1016/j.bbmt.2005.02.006
Gori E, Arpinati M, Bonifazi F, Errico A, Mega A, Alberani F, Sabbi V, Costazza G, Leanza S, Borrelli C, Berni M, Feraut C, Polato E, Altieri MC, Pirola E, Loddo MC, Banfi M, Barzetti L, Calza S, Brignoli C, Bandini G, De Vivo A, Bosi A, Baccarani M (2007) Cryotherapy in the prevention of oral mucositis in patients receiving low-dose methotrexate following myeloablative allogeneic stem cell transplantation: a prospective randomized study of the Gruppo Italiano Trapianto di Midollo Osseo nurses group. Bone Marrow Transplant 39:347–352. https://doi.org/10.1038/sj.bmt.1705590
de Paula EF, Bezinelli LM, da Graça Lopes RM, Nascimento Sobrinho JJ, Hamerschlak N, Correa L (2015) Efficacy of cryotherapy associated with laser therapy for decreasing severity of melphalan-induced oral mucositis during hematological stem-cell transplantation: a prospective clinical study. Hematol Oncol 33:152–158. https://doi.org/10.1002/hon.2133
Funding
This work was supported by JSPS KAKENHI Grant Number JP 22K17473.
Author information
Authors and Affiliations
Contributions
Saori Oku, Toshiko Futatsuki, and Shinsuke Mizutani contributed to the study conception and study design. Material preparation and data collection was performed by Saori Oku, Toshiko Futatsuki, Yoshiko Imamura, Haruna Hikita, Akemi Inada, and Yasuo Mori. Saori Oku, Toshiko Futatsuki, and Shinsuke Mizutani were involved in statistical analysis. The first draft of the manuscript was written by Saori Oku, Toshiko Futatsuki, Shinsuke Mizutani, Yasuo Mori, and Haruhiko Kashiwazaki, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Kyushu university hospital (approval number: 2021–417).
Consent to participate
No consent to participate was needed because of the retrospective nature of this study.
We announce the information of this research at our web site.
Consent to publish
The authors affirm that human research participants provided informed consent for publication.
Competing interests
All authors have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oku, S., Futatsuki, T., Imamura, Y. et al. Protective effect of cryotherapy against oral mucositis among allogeneic hematopoietic stem cell transplant recipients using melphalan-based conditioning. Support Care Cancer 31, 521 (2023). https://doi.org/10.1007/s00520-023-07989-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07989-9