Abstract
Purpose
To analyze the level of family resilience in Chinese gynecological cancer survivors and determine whether perceived spousal support plays a mediating role in the relationship between dyadic communication quality and family resilience, enhance the confidence of families in coping with the disease together, and thus promote psychosocial adaptation to cancer.
Methods
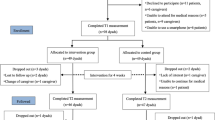
A total of 348 gynecologic cancer survivors were selected from a gynecologic ward in a public hospital in Shandong Province, China. All participants completed the Sociodemographic and Clinical Characteristics Questionnaire, Couples’ Communication Quality Scale (CCQS), Perceived Social Support Scale (PSSS), and Family Hardiness Index (FHI). The mediating effect of perceived spousal support was estimated using the bootstrap method via IBM SPSS AMOS 21.0.
Results
The mean FHI score was 53.03 ± 9.34 points, showing moderate levels of family resilience. Family resilience was shown to be significantly positively associated with both perceived spousal support and dyadic communication quality (both p < 0.01). Furthermore, perceived spousal support was shown to partially mediate the relationship between communication quality and family resilience (β = 0.141; 95% confidence interval: 0.063–0.243).
Conclusion
The level of family resilience in survivors of gynecologic cancer needs to be further improved, and perceived spousal support partially mediates the relationship between dyadic communication quality and family resilience within this population. Therefore, dyadic communication quality and subjective perceived spousal support should be enhanced for gynecologic cancer survivors to increase their family resilience.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca Cancer J Clin 71(3):209–249
Wang X, Chen C, Liu P et al (2018) The morbidity of sexual dysfunction of 125 chinese women following different types of radical hysterectomy for gynaecological malignancies. Arch Gynecol Obstet 297(2):459–466
Secoșan C, BalintPirtea O et al (2019) Surgically induced menopause-a practical review of literature. Medicina (Kaunas) 55(8):482
La Rosa VL, Garzon S, Gullo G et al (2020) Fertility preservation in women affected by gynaecological cancer: the importance of an integrated gynaecological and psychological approach. Ecancermedicalscience 14:1035
Beesley VL, Alemayehu C, Webb PM (2018) A systematic literature review of the prevalence of and risk factors for supportive care needs among women with gynaecological cancer and their caregivers. Support Care Cancer 26(3):701–710
Faller H, Brähler E, Härter M et al (2017) Unmet needs for information and psychosocial support in relation to quality of life and emotional distress: a comparison between gynecological and breast cancer patients. Patient Educ Couns 100(10):1934–1942
Tsai LY, Wang KL, Liang SY et al (2017) The lived experience of gynecologic cancer survivors in taiwan. J Nurs Res 25(6):447–454
Sekse R, Dunberger G, Olesen ML et al (2019) Lived experiences and quality of life after gynaecological cancer-an integrative review. J Clin Nurs 28(9–10):1393–1421
Walsh F (1996) The concept of family resilience: crisis and challenge. Fam Process 35(3):261–281
Li Y, Qiao Y, Luan X et al (2019) Family resilience and psychological well-being among Chinese breast cancer survivors and their caregivers. Eur J Cancer Care (Engl) 28(2):e12984
Zhuo R, Yu Y, Shi X (2022) Family resilience and adolescent mental health during covid-19: a moderated mediation model. Int J Environ Res Public Health 19(8):4801
Li Y, Wang K, Yin Y et al (2018) Relationships between family resilience, breast cancer survivors’ individual resilience, and caregiver burden: a cross-sectional study. Int J Nurs Stud 88:79–84
Buzzanell PM (2010) Resilience: talking, resisting, and imagining new normalcies into being. J Commun 60(1):1–22
Lucas K, Buzzanell P (2012) Memorable messages of hard times:constructing short and long-term resiliencies through family communication. J Fam Commun 3(12):189–208
Lillie HM, Chernichky-Karcher S, Venetis MK (2021) Dyadic coping and discrete emotions during covid-19: connecting the communication theory of resilience with relational uncertainty. J Soc Pers Relat 38(026540752110093026SI):1844–1868
Lillie HM, Venetis MK, Chernichky-Karcher SM (2018) “he would never let me just give up”: communicatively constructing dyadic resilience in the experience of breast cancer. Health Commun 33(12):1516–1524
Venetis M, Chernichky-Karcher S, Lillie H (2020) Communicating resilience: predictors and outcomes of dyadic communication resilience processes among both cancer patients and cancer partners. J Appl Commun Res 1(48):49–69
Black K, Lobo M (2008) A conceptual review of family resilience factors. J Fam Nurs 14(1):33–55
Zimet GD, Powell SS, Farley GK et al (1990) Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess 55(3–4):610–617
Haber MG, Cohen JL, Lucas T et al (2007) The relationship between self-reported received and perceived social support: a meta-analytic review. Am J Community Psychol 39(1–2):133–144
Teskereci G, Kulakaç O (2018) Life experiences of caregivers of women with gynaecological cancer: a mixed-methods systematic review. Eur J Cancer Care (Engl) 27(1)
Teo I, Cheung YB, Lim T et al (2018) The relationship between symptom prevalence, body image, and quality of life in asian gynecologic cancer patients. Psychooncology 27(1):69–74
Burleson BR (2003) The experience and effects of emotional support: what the study of cultural and gender differences can tell us about close relationships, emotion, and interpersonal communication. Pers Relatsh 10(1):1–23
Park YS, Kim BS (2008) Asian and European American cultural values and communication styles among Asian American and European American college students. Cultur Divers Ethnic Minor Psychol 14(1):47–56
Kline R (2015) Concepts and tools. In: Kenny D, Little T (eds) Principles and practice of structural equation modeling, 4th edn. Guilford Publications, New York, pp 14–16
Clark LA, Watson D (1995) Constructing validity: basic issues in objective scale development. Psychol Assess 7(3):309–319
Chen XX, Li YJ, Sun HF et al (2023) Development of couples’ communication quality scale for gynecological cancer patients and the best of its reliability and validity. Chin J Prac Nurs 2(39):55–60
Ban Y, Li M, Yu M et al (2021) The effect of fear of progression on quality of life among breast cancer patients: the mediating role of social support. Health Qual Life Outcomes 19(1):178
Mccubbin H, Thompson A, Mccubbin M (1996) Family assessment: resiliency, coping and adaptation: inventories for research and practice Wisconsin. University of Wisconsin, Madison
Liu Y, Yang JQ, Ye BL et al (2014) Reliability and valldity of the Chinese version of family hardiness index. J Nurs Adm 11(14):770–772
Peng Y, Wang J, Sun G et al (2021) Family hardiness in patients with heart failure: exploring protective factors and identifying the mediator. Psychol Res Behav Manag 14:355–364
Aquil A, El KO, El AN et al (2021) Body image dissatisfaction and lower self-esteem as major predictors of poor sleep quality in gynecological cancer patients after surgery: cross-sectional study. Bmc Womens Health 21(1):229
Catona D, Greene K, Venetis MK et al (2022) Conflicting views during gynecologic cancer care: a comparison of patients’ and caregivers’ perceptions of burden. Support Care Cancer 30(9):7755–7762
Lheureux S, Gourley C, Vergote I et al (2019) Epithelial ovarian cancer. Lancet 393(10177):1240–1253
Wong P, Liamputtong P, Koch S et al (2019) The impact of social support networks on family resilience in an australian intensive care unit: a constructivist grounded theory. J Nurs Scholarsh 51(1):68–80
Yuan Q, Fan Z, Leng J (2022) The effect of emotional reactivity on marital quality in Chinese Couples: the mediating role of perceived partner responsiveness. Front Psychol 12:787899
Badr H (2017) New frontiers in couple-based interventions in cancer care: refining the prescription for spousal communication. Acta Oncol 56(2):139–145
Manne SL, Kashy DA, Kissane DW et al (2019) The course and predictors of perceived unsupportive responses by family and friends among women newly diagnosed with gynecological cancers. Transl Behav Med 9(4):682–692
Fahmer N, Faller H, Engehausen D et al (2022) Patients’ challenges, competencies, and perceived support in dealing with information needs - a qualitative analysis in patients with breast and gynecological cancer. Patient Educ Couns 105(7):2382–2390
Walsh F (2003) Family resilience: a framework for clinical practice. Fam Process 42(1):1–18
Henry CS, Morris AS, Harrist AW (2015) Family resilience: moving into the third wave. Fam Relat 64(1):22–43
Lim JW, Shon EJ (2018) The dyadic effects of family cohesion and communication on health-related quality of life: the moderating role of sex. Cancer Nurs 41(2):156–165
Kelley H, Thibaut J (1978) Interpersonal relations: a theory of interdependence. Wiley, New York
Wei M, Su JC, Carrera S et al (2013) Suppression and interpersonal harmony: a cross-cultural comparison between chinese and european americans. J Couns Psychol 60(4):625–633
Acknowledgements
The authors would like to thank the medical staff and all participants.
Author information
Authors and Affiliations
Contributions
Xiaoxin Chen: study conception/design; data collection/analysis; drafting of manuscript. Yingju Li and Hanfei Sun: study conception/design. Tianyi Wang and Xiaoxiang Xu: data collection. Min Li: supervision and critical revisions for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical approval was obtained from the Research Ethics Committee of the School of Nursing and Rehabilitation, Shandong University (approval number: 2022-R-069). We made it clear to the participants that participation in this study was voluntary and that they were free to withdraw from the study at any time and for any reason, without penalty. The research should not result in any undue discomfort to participants. All information provided by the participants remained confidential and anonymous. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Information is anonymized, and the submission does not include images that may identify the person.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, X., Li, Y., Sun, H. et al. Dyadic communication quality and family resilience in gynecologic cancer survivors: a study on the mediating role of perceived spousal support. Support Care Cancer 31, 68 (2023). https://doi.org/10.1007/s00520-022-07492-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-022-07492-7