Abstract
Background
Outcomes-based agreements (OBAs) have the potential to provide more timely patient access to novel therapies, although they are not suitable for every new medication or reimbursement scenario. The authors of this paper studied how to operationalize an OBA in oncology by leveraging existing real-world data (RWD) infrastructure in the province of Alberta.
Objective
The main objectives were to (1) evaluate which health outcomes in oncology are suitable for OBAs and whether they can be tracked with existing infrastructure, and (2) determine how RWD in oncology can be used to implement an OBA and the expected timing for delivery.
Methods
Using the Oncology Outcomes (O2) Group infrastructure and Alberta administrative data, a review of five key oncology outcomes was performed to determine suitability to support an OBA.
Results
Overall survival and time-to-next-treatment were determined as potentially suitable oncology outcomes for OBAs; progression-free survival, patient-reported outcomes, and return to work were deemed inadequate for OBAs at the current time due to data limitations.
Conclusions
Results indicate that it is feasible to leverage RWD to support OBAs in oncology in Alberta, with minimal additional data, resources, and infrastructure. The operational processes and steps to collect and analyze RWD for OBAs were identified, starting with performing an RWD feasibility study. The expected timeframe to fulfill the real-world evidence (RWE) requirements for an OBA is approximately 3 years for cancers with short trajectories.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
With the growing number of promising therapies with imperfect data, particularly in rare diseases and precision oncology, coupled with long reimbursement timelines, timely access to novel therapies has become increasingly challenging. Outcomes-based agreements (OBAs) have the potential to accelerate patients’ access to these therapies, while mitigating risk for payers [1, 2]. Traditionally, an OBA is an agreement between a manufacturer and a payer in which the manufacturer will issue a refund or rebate to the payer based on how well the therapy performs in a real-world patient population, measured against an agreed-upon, pre-defined set of benchmarks. OBAs are a strategy to address uncertainties that create access barriers; they are not a replacement for clinical trials, and they are not appropriate for all drugs or for all reimbursement scenarios.
The UK’s 2021 Commercial Framework for New Medicines advises that OBAs should “only be considered once simple discounts have been demonstrated to be unsuitable” [3]. Research conducted by the RWE & OBA Working Group, established in 2019 to explore the opportunity for RWE to support OBAs in Canada, suggests that OBAs offer the greatest benefit in the following circumstances [4]:
-
Variable response: When clinical trials suggest that only a limited proportion of patients (e.g., 50%) reach a desired health outcome, OBAs can reduce a payer’s risk by limiting ongoing reimbursement to patients who meet agreed-upon outcome criteria.
-
Limited data: When promising but incomplete early clinical trial data make it difficult to assess a drug’s performance, an OBA can provide access to patients with no suitable treatment alternatives.
-
Disputed therapeutic benefit: When stakeholders disagree on the magnitude of therapeutic benefit suggested by clinical trial data, an OBA can help patients access treatment earlier, with continued access dependent on proof of benefit.
As detailed in Health Canada’s proposed national strategy for high-cost drugs for rare diseases, the success of an OBA depends on clear, objective measures of benefit [5]. If the evidence ultimately reveals a more modest benefit than anticipated, OBAs allow for reduction or discontinuation of reimbursement, thus mitigating risk for public and private payers.
OBAs have gained ground internationally as a strategy for managing access and risk, but are still in their infancy in Canada. Recognized barriers include inconsistent availability of appropriate real-world data (RWD), potential increase in administrative burden, challenges in reaching agreement about the adjudication process to assess efficacy, and a lack of resources and infrastructure to implement such agreements. At the same time, Canada’s RWD infrastructure has been advancing, particularly in Alberta, which has been developing advanced infrastructure, broad data capture, and resources to support oncology analytics. The Oncology Outcomes (O2) group, a consortium of oncology research and clinical leaders, is playing a key role in this regard.
Compounding the aforementioned barriers, OBAs are confidential in Canada, and there are no publicly available examples for stakeholders to learn from. This study sought to fill this information gap by describing a feasible process for operationalizing the RWE requirements for an OBA.
The objectives of the study were to evaluate which health outcomes are suitable for OBAs in oncology and to examine if such health outcomes can be tracked using existing infrastructure in Alberta and Patient Support Programs (PSP). The study also explored the use of OBA data processes to facilitate the data tracking required to support an OBA.
Methods
The lead author and investigator of the analysis, Dr. Winson Cheung, is an academic researcher with a special interest in RWE. Dr. Cheung had the final input and authority in the interpretation of the findings and the content of this paper. The second author, Dr. Chris Cameron, is recognized as a global thought leader in health economics and outcomes research. The last two authors, Allison Wills and Arif Mitha, have expertise in outcomes-based agreement planning and implementation, and belong to the RWE & OBA Working Group, established in 2019 to explore the opportunity for RWE to support OBAs in Canada. Payers were not involved in the analysis at this stage and will be invited to comment on these findings at a future date. None of the authors received any direct compensation from industry for this work.
In 2019 and 2020, the RWE & OBA Working Group’s research and analysis led to the development of several tools to aid in the evaluation and implementation of OBAs, including a 7-step OBA implementation framework [4] and a Decision modelling tool: outcomes-based agreement vs. price discount contract [6].
The 7-step OBA implementation framework was used to support the research on RWE for OBAs. The framework includes the following steps:
-
1.
Determine if the drug is fit for OBA
-
2.
Negotiate OBA and design program
-
3.
Build OBA program
-
4.
Enroll doctors and patients in program
-
5.
Begin and monitor drug treatment
-
6.
Report and adjudicate
-
7.
Conduct annual review
The study investigators evaluated five health outcomes for suitability to support an OBA in oncology in Canada: (1) overall survival (OS), (2) time to next treatment (TTNT), (3) progression-free survival (PFS), (4) patient-reported outcomes (PROs), and (5) return to work.
The decision to include TTNT as an outcome of interest, in addition to the well-established OS and PFS, aligns with the increasing use of TTNT as a surrogate outcome in both clinical trials and RWE. A 2020 analysis of TTNT, in the context of cutaneous lymphoma, described TTNT as a useful surrogate endpoint for “duration of clinical benefit” that also accounts for patient tolerance and adherence [7]. A real-world analysis of 4729 advanced cancer patients, reported in the Journal of Clinical Oncology in 2016, concluded that “concordance of TTNT and OS for patients with biomarker-associated therapies validates the clinical utility of TTNT as a surrogate endpoint that can be assessed using EMR extracted data” [8].
It should be noted that the alignment of TTNT with PFS is not always perfect, and thus TTNT estimates may exceed the corresponding PFS estimates in settings that lead to delays in subsequent therapies [9].
The investigators also assessed whether health outcomes can be tracked by the O2 Group with existing infrastructure in Alberta and by PSP infrastructure at a national level. They outlined a process for using the O2 Group’s capabilities and Alberta administrative health data, and created two additional process designs that leveraged PSP infrastructure and data.
Results
Health outcomes suitable for OBAs in oncology
Two health outcomes, namely, OS and TTNT, were identified as suitable for the collection of RWD to support OBAs in oncology using administrative data (Table 1). These outcomes were deemed suitable based on criteria of data readiness (accessible for an OBA, complete, and accurate), data interpretation (health outcome is clear and simple), and data timeframe (can be collected in a reasonable timeframe). OS data are available through the Alberta Cancer Registry and Vital Statistics, have been used in published studies [2], and measure an objective event that can be easily and consistently interpreted. Diagnoses with relatively short anticipated OS timeframes could be suitable for an OBA. TTNT data are accessible through the Alberta Pharmaceutical Information Network (PIN) database containing all prescription data in the province for all payers and have been used in published studies [2, 10]. A coding algorithm must be developed to determine a specific treatment pattern, and data are generally accessible within 1 month of dispensing. Progression-free survival, patient-reported outcomes, and return to work were currently deemed not suitable outcomes due to data limitations. PROs have future potential for use in OBAs, but additional RWD collection activities would be required.
Data processes to operationalize RWD for OBAs in oncology
Three data processes were identified to operationalize RWD for OBAs in oncology: (1) administrative data, (2) administrative data with PSP support, and (3) PSP data (see Table 2). Three data elements are managed within each process: (1) data planning, (2) data capture, and (3) data analysis.
Data planning
When considering an OBA, an RWD feasibility study is advised. This can be conducted by either a manufacturer, a payer, or both, in collaboration with a data expert. The aim of the feasibility study is to determine if the appropriate health outcomes data can be collected to meet the needs of an OBA for a specific drug scenario. The feasibility study seeks to answer the following questions:
-
1.
Which health outcomes measurements could be used for the drug of interest?
-
2.
What RWD is available and what data sources are most appropriate to measure the identified health outcomes?
-
3.
Regarding the identified health outcomes:
-
(a)
Does the data source have the required data quality to support the OBA?
-
(b)
Is the patient population sufficient to allow for the analysis of the outcomes?
-
(c)
What is the anticipated time to complete the data component of the OBA, including data capture and results generation?
-
(a)
The findings of the feasibility study should serve as a key input when payers and manufacturers are designing OBAs and can provide important insights on OBA design methodology. Feasibility discussions can happen early, including prior to drug launch. Ethics approval may be required to use certain data sets for the feasibility study and for the OBA.
Data capture
Elements that impact the way data are captured and populated in databases include (1) the patient registry, (2) drug distribution, and (3) the health outcomes data source. Depending on the scenarios for different drugs, three processes were developed to enable data capture for the purpose of measuring health outcomes for an OBA (Table 2).
Process 1: Administrative data: Administrative data refer to data that are populated during regular clinical or administrative processes. Process 1 provides an OBA strategy that uses only administrative data. For OS and TTNT, the benefits of this process include.
-
1.
Administrative data are already being captured in regular clinical or administrative processes and populated in administrative data sources. No additional infrastructure or processes are required for the purposes of OBA data collection.
-
2.
There is no additional work for doctors or patients for the data collection required for an OBA.
However, the use of only administrative data also has limitations: there are fewer controls for patient eligibility, which could lead to a wider scope of patients being prescribed the drug than intended within the OBA criteria. As such, the use of administrative data exclusively may not be appropriate for all OBAs, and additional data process options were designed (process 2 and process 3).
Process 2: Administrative data and PSP infrastructure: Process 2 combines administrative data with PSP infrastructure support. The PSP infrastructure is used to create a patient registry, which makes it possible to align patient eligibility with the OBA criteria. As in process 1, administrative data are also used as the health outcomes data source.
Process 3: PSP data and infrastructure: Process 3 uses PSP infrastructure for the patient registry and PSP data as the health outcome data source. The use of PSP infrastructure and data in OBAs offers several unique advantages compared to administrative data:
-
1.
The use of a PSP registry allows for greater oversight and control of patient eligibility.
-
2.
If the PSP is used for all data capture activities (process 3), it can potentially be scaled to the national level and include all payers.
-
3.
The PSP is flexible and can be customized to meet the needs of the OBA.
However, the use of PSP infrastructure for OBA data collection would entail additional work for doctors and patients. Also, PSPs need to be strategically set up at the outset to capture data to support a potential OBA. A key consideration is that the PSP must enable the collection of high-quality data that meet the requirements of payers and manufacturers.
Data analysis
Data should be accessed and analyzed by data experts, with results aggregated and reported as specified in the OBA. This includes PSP data, which can be analyzed by a third-party data expert such as the O2 group.
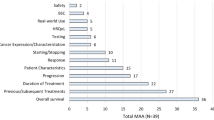
Total estimated time required for the RWD component of an OBA—2.5 to 3 years
The total estimated timeframe required to complete the RWD component of an OBA is 2.5–3 years when using OS or TTNT in Alberta (Fig. 1). For both OS and TTNT, patients are recruited over a 12-month period and then monitored for an additional 12 months after initiation of therapy.
For OS using process 1 (see Table 2, Fig. 1), the following estimated timeline was developed: 12 months for a sufficient number of patients to start on drug; 12 months to monitor patients; 6 months for data collection logistics to receive information on survival status; 3 months for analysis and reporting by a team with data expertise. This resulted in a total approximate timeframe of 2 years and 9 months. This timeframe aligns with the oncology OBA process presented in an Australian study [11]. For TTNT using process 1 (see Table 2, Fig. 1), the following estimated timeline was developed: 12 months for a sufficient number of patients to start on drug; 12 months to monitor patients; 1 month for data collection logistics in the pharmacy PIN system; 3 months for analysis and reporting by a team with data expertise. This resulted in a total approximate timeframe of 2 years and 4 months.
Discussion
This research has found that it is feasible to operationalize an OBA in oncology using Alberta administrative health data with minimal additional data resources, although administrative support to conduct the analyses would still be required. For stakeholders exploring the value of OBAs for a novel medication, this analysis can serve as a “proof of concept” model that demonstrates feasibility under some circumstances.
The health outcomes of OS and TTNT, which are already being collected in Alberta, were found to be suitable to support an OBA, with data management support from the O2 group. Three operational processes to collect, analyze, and report RWD for OBAs were identified, using administrative health data, PSP infrastructure, and PSP data. All processes start with an RWD feasibility study conducted by a team with data expertise. An estimated timeframe to conduct the RWD component of an OBA is 2.5–3 years.
Insights from this research may be valuable to the Canadian Agency for Drugs and Technologies in Health (CADTH) and Institut national d'excellence en santé et en services sociaux (INESSS), which provide research and analysis to support decisions about new therapies. Manufacturers, provincial drug plans, and private insurers that are considering implementing OBAs in oncology may also benefit from the findings shared here. When exploring the feasibility of OBAs, it will be important for payers and other stakeholders to quantify and manage the administrative burden to ensure it does not cancel the benefits of OBAs.
Conclusions
The findings from this study should enhance Canadian stakeholders’ understanding of how an OBA in oncology can be operationalized using administrative data and the time it will take to complete an OBA using existing RWD infrastructure.
It should be noted that this analysis addresses only one barrier to OBA implementation, namely, the availability of appropriate RWD. Further research is needed to explore and address additional potential barriers such as administrative burden and efficacy of adjudication processes. Future research should also focus on how OBAs can be operationalized at a pan-Canadian level and in therapeutic areas outside oncology, such as rare diseases.
Data Availability
Aggregate-level data analysed in this study are available on request from the corresponding author. Individual-level data are not publicly available due to Canadian data privacy laws governing personal health information.
Abbreviations
- OBAs :
-
Outcomes-based agreements
- RWD :
-
Real-world data
- RWE :
-
Real-world evidence
- O2 Group :
-
Oncology Outcomes (O2) group
- PSP :
-
Patient support programs
- OS :
-
Overall survival
- TTNT :
-
Time to next treatment
- PFS :
-
Progression-free survival
- PROs :
-
Patient-reported outcomes
- PIN :
-
Alberta Pharmaceutical Information Network
- CADTH :
-
Canadian Agency for Drugs and Technologies in Health
- INESSS :
-
Institut national d’excellence en santé et en services sociaux
References
Facey KM, Espin J, Kent E, Link A, Nicod E, O’Leary A, Xoxi E, van de Vijver I, Zaremba A, Benisheva T, Vagoras A, Upadhyaya S (2021) Implementing outcomes-based managed entry agreements for rare disease treatments: nusinersen and tisagenlecleucel. Pharmacoeconomics 39:1021–1044
O’Sullivan DE, Cheung WY, Syed IA, Moldaver D, Shanahan MK, Bebb DG, Sit C, Brenner DR, Boyne DJ (2021) Real-world treatment patterns, clinical outcomes, and health care resource utilization in extensive-stage small cell lung cancer in Canada. Curr Oncol 28(4):3091–3103
NHS commercial framework for new medicines.https://www.england.nhs.uk/publication/nhs-commercial-framework-for-new-medicines/. Accessed on 24 Jan 2022
RWE and OBA Working Group. 2019 Research and Outputs Executive Summary. https://static1.squarespace.com/static/58fd16af1b631b1afffae9e0/t/5f8e437dd9a86a5bd6b09076/1603158910148/2019_Nov_RWE_OBA_WorkingGroup_ExecSummary.pdf Accessed on 17 Dec 2021
Building a national strategy for high-cost drugs for rare diseases. Government of Canada. January 2021. https://www.canada.ca/content/dam/hc-sc/documents/services/health-related-consultation/National-Strategy-High-Cost-Drugs-eng.pdf. Accessed on 24 Jan 2022
RWE and OBA Working Group. 2020 Research and Outputs Executive Summary. https://static1.squarespace.com/static/58fd16af1b631b1afffae9e0/t/5fa9c557b874e907d317c5dd/1604961623504/2020_RWE_OBA_WorkingGroup_ExecSummary.pdf. Accessed on 17 Dec 2021
Campbell BA, Scarisbrick JJ, Youn HK, Wilcox A, McCormack C, Prince HM (2020) Time to next treatment as a meaningful endpoint for trials of primary cutaneous lymphoma. Cancers (Basel) 12(8):2311
Marshall J, Schwartzberg LS, Bepler G, Spetzler D, El-Deiry WS, Xiao N, Reddy SK, Kim ES, Poste GH, Raghavan D (2016) Novel panomic validation of time to next treatment (TNT) as an effective surrogate outcome measure in 4,729 patients. J Clin Oncol 34:15_suppl, 11521–11521
Walker B, Boyd M, Aguilar K, Davies K, Espirito J, Frytak J, Robert N (2021) Comparisons of real-world time-to-event end points in oncology research. JCO Clin Cancer Inform 5:45–46
Tay J, Chen G, Cowling T, Shaw E, Farris M, Liu F, Jimenez-Zepeda V (2019) Early mortality following diagnosis of multiple myeloma from 2011 to 2016 in Alberta, Canada: initial results from the population-based Identifying Outcomes in Real-World Multiple Myeloma (INFORMM) study. J Clin Oncol 37(15):e19509
Tuffaha HW, Scuffham PA (2018) The Australian managed entry scheme: are we getting it right? Pharmacoeconomics 36(5):555–565
Funding
20Sense’s role in this work was supported by the RWE & OBA Working Group. The group included market access, RWE, and patient support program (PSP) professionals from AstraZeneca, Bayer, BioScript Solutions, Janssen, Novartis, Pfizer, and 20Sense.
Author information
Authors and Affiliations
Contributions
W.Y.C., C.C., A.M., and A.W. contributed to the conception of the project. C.C., A.M., and A.W. wrote sections of the manuscript. W.C., C.C., A.M., and A.W. critically revised the work and edited the entire manuscript and approved the final manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
C.C. is an employee and shareholder of EVERSANA Life Science Services LLC. W.Y.C is Principal Director and Co-Founder of O2. A.M. is employed by 20Sense, A.W. is a shareholder and is employed by 20Sense; both are co-chairs of the Real-World Evidence and Outcomes-Based Agreements Working Group.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cheung, W.Y., Cameron, C., Mitha, A. et al. Building infrastructure for outcomes-based agreements in Canada: can administrative health data be used to support an outcomes-based agreement in oncology?. Support Care Cancer 31, 5 (2023). https://doi.org/10.1007/s00520-022-07486-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-022-07486-5