Abstract
Introduction
Oncology guidelines recommend participation in cancer rehabilitation or exercise services (CR/ES) to optimize survivorship. Yet, connecting the right survivor, with the right CR/ES, at the right time remains a challenge. The Exercise in Cancer Evaluation and Decision Support (EXCEEDS) algorithm was developed to enhance CR/ES clinical decision-making and facilitate access to CR/ES. We used Delphi methodology to evaluate usability, acceptability, and determine pragmatic implementation priorities.
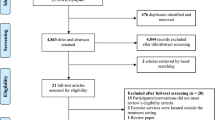
Methods
Participants completed three online questionnaires including (1) simulated case vignettes, (2) 4-item acceptability questionnaire (0–5 pts), and (3) series of items to rank algorithm implementation priorities (potential users, platforms, strategies). To evaluate usability, we used Chi-squared test to compare frequency of accurate pre-exercise medical clearance and CR/ES triage recommendations for case vignettes when using EXCEEDS vs. without. We calculated mean acceptability and inter-rater agreement overall and in 4 domains. We used the Eisenhower Prioritization Method to evaluate implementation priorities.
Results
Participants (N = 133) mostly represented the fields of rehabilitation (69%), oncology (25%), or exercise science (17%). When using EXCEEDS (vs. without), their recommendations were more likely to be guideline concordant for medical clearance (83.4% vs. 66.5%, X2 = 26.61, p < .0001) and CR/ES triage (60.9% vs. 51.1%, X2 = 73.79, p < .0001). Mean acceptability was M = 3.90 ± 0.47; inter-rater agreement was high for 3 of 4 domains. Implementation priorities include 1 potential user group, 2 platform types, and 9 implementation strategies.
Conclusion
This study demonstrates the EXCEEDS algorithm can be a pragmatic and acceptable clinical decision support tool for CR/ES recommendations. Future research is needed to evaluate algorithm usability and acceptability in real-world clinical pathways.



Similar content being viewed by others
Availability of data and coding
Data and coding available upon request.
References
Mctiernan A, Friedenreich CM, Katzmarzyk PT et al (2019) Physical activity in cancer prevention and survival: a systematic review. Med Sci Sports Exerc 51:1252–1261
Campbell KL, Winters-Stone KM, Wiskemann J, May AM, Schwartz AL, Courneya KS, Zucker DS, Matthews CE, Ligibel JA, Gerber LH, Morris GS, Patel AV, Hue TF, Perna FM, Schmitz KH (2019) Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc 51(11):2375–2390. https://doi.org/10.1249/MSS.0000000000002116
Avancini A, Pala V, Trestini I et al (2020) Exercise levels and preferences in cancer patients: a cross-sectional study. Int J Environ Res Public Health 17:5351. https://doi.org/10.3390/ijerph17155351
Covington K, Marshall T, Campbell G et al (2021) Development of the Exercise in Cancer Evaluation and Decision Support (EXCEEDS) algorithm. Support Care Cancer 29:6469–6480. https://doi.org/10.1007/s00520-021-06208-7
Sleight AG, Gerber LH, Marshall TF et al (2022) A systematic review of functional outcomes in cancer rehabilitation research. Arch Phys Med Rehabil. https://doi.org/10.1016/J.APMR.2022.01.142
Patel AV, Friedenreich CM, Moore SC et al (2019) American College of Sports Medicine roundtable report on physical activity, sedentary behavior, and cancer prevention and control. Med Sci Sports Exerc 51:2391–2402. https://doi.org/10.1249/MSS.0000000000002117
Faro JM, Mattocks KM, Mourao D et al (2021) (2021) Experiences and perceptions of referrals to a community-based physical activity program for cancer survivors: a qualitative exploration. BMC Heal Serv Res 211(21):1–10. https://doi.org/10.1186/S12913-021-06365-9
Hardcastle SJ, Maxwell-Smith C, Kamarova S et al (2018) Factors influencing non-participation in an exercise program and attitudes towards physical activity amongst cancer survivors. Support Care Cancer 26:1289–1295. https://doi.org/10.1007/s00520-017-3952-9
Stout NL, Brown JC, Schwartz AL et al (2020) An exercise oncology clinical pathway: screening and referral for personalized interventions. Cancer 126:2750–2758. https://doi.org/10.1002/cncr.32860
Mayer DK, Alfano CM (2019) Personalized risk-stratified cancer follow-up care: its potential for healthier survivors, happier clinicians, and lower costs. JNCI J Natl Cancer Inst 111:442–448. https://doi.org/10.1093/jnci/djy232
Schmitz KH, Campbell AM, Stuiver MM et al (2019) Exercise is medicine in oncology: engaging clinicians to help patients move through cancer. CA Cancer J Clin 69:468–484. https://doi.org/10.3322/caac.21579
Coletta AM, Campbell A, Morris GS, Schmitz KH (2020) Synergy between licensed rehabilitation professionals and clinical exercise physiologists: optimizing patient care for cancer rehabilitation. Semin Oncol Nurs 36:150975. https://doi.org/10.1016/j.soncn.2019.150975
Stout NL, Santa Mina D, Lyons KD, et al (2020) A systematic review of rehabilitation and exercise recommendations in oncology guidelines. CA Cancer J Clin caac.21639. https://doi.org/10.3322/caac.21639
Shallwani SM, King J, Thomas R et al (2019) Methodological quality of clinical practice guidelines with physical activity recommendations for people diagnosed with cancer: a systematic critical appraisal using the AGREE II tool. PLoS ONE 14:e0214846. https://doi.org/10.1371/JOURNAL.PONE.0214846
Nadler M, Bainbridge D, Tomasone J et al (2017) Oncology care provider perspectives on exercise promotion in people with cancer: an examination of knowledge, practices, barriers, and facilitators. Support Care Cancer 25:2297–2304. https://doi.org/10.1007/s00520-017-3640-9
Pergolotti M, Deal AM, Lavery J et al (2015) The prevalence of potentially modifiable functional deficits and the subsequent use of occupational and physical therapy by older adults with cancer. J Geriatr Oncol 6:194–201. https://doi.org/10.1016/j.jgo.2015.01.004
Brick R, Bender C, Skidmore E (2021) Impact of cancer and cancer-related treatments on participation restrictions. Br J Occup Ther 84:222–229. https://doi.org/10.1177/0308022620923858
Alfano CM, Jefford M, Maher J et al (2019) Building personalized cancer follow-up care pathways in the United States: lessons learned from implementation in England, Northern Ireland, and Australia. Am Soc Clin Oncol Educ B 39:625–639. https://doi.org/10.1200/edbk_238267
Osheroff JA, Teich JM, Middleton B et al (2007) A roadmap for national action on clinical decision support. J Am Med Informatics Assoc 14:141–145. https://doi.org/10.1197/jamia.M2334
Sittig DF, Wright A, Osheroff JA et al (2008) Grand challenges in clinical decision support. J Biomed Inform 41:387–392. https://doi.org/10.1016/j.jbi.2007.09.003
Pawloski PA, Brooks GA, Nielsen ME, Olson-Bullis BA (2019) A systematic review of clinical decision support systems for clinical oncology practice. JNCCN J Natl Compr Cancer Netw 17:331–338
Ligibel JA, Bohlke K, May AM, et al (2022) Exercise, diet, and weight management during cancer treatment: ASCO guideline. 101200/JCO2200687.
(2018) Using Prioritization Matrices to Inform UX Decisions. https://www.nngroup.com/articles/prioritization-matrices/. Accessed 14 Oct 2020
Powell BJ, Waltz TJ, Chinman MJ et al (2015) A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci 10:21. https://doi.org/10.1186/s13012-015-0209-1
Damschroder LJ, Aron DC, Keith RE et al (2009) Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 4:50. https://doi.org/10.1186/1748-5908-4-50
Knoerl R, Mazzola E, Hong F et al (2021) Exploring the impact of a decision support algorithm to improve clinicians’ chemotherapy-induced peripheral neuropathy assessment and management practices: a two-phase, longitudinal study. BMC Cancer 21:236. https://doi.org/10.1186/s12885-021-07965-8
Khairat S, Marc D, Crosby W, Al Sanousi A (2018) Reasons for physicians not adopting clinical decision support systems: critical analysis. J Med Internet Res 20. https://doi.org/10.2196/medinform.8912
Birko S, Dove ES, Özdemir V, Dalal K (2015) Evaluation of nine consensus indices in delphi foresight research and their dependency on Delphi survey characteristics: a simulation study and debate on delphi design and interpretation. PLoS ONE 10:1–14. https://doi.org/10.1371/journal.pone.0135162
Hsu CC, Sandford BA (2007) The Delphi technique: making sense of consensus. Pract Assessment, Res Eval 12:1–8. https://doi.org/10.4135/9781412961288.n107
Trevelyan EG, Robinson N (2015) Delphi methodology in health research: how to do it? Eur J Integr Med 7:423–428. https://doi.org/10.1016/j.eujim.2015.07.002
Chang AM, Gardner GE, Duffield C, Ramis M-A (2010) A Delphi study to validate an advanced practice nursing tool. J Adv Nurs 66:2320–2330. https://doi.org/10.1111/j.1365-2648.2010.05367.x
Hagen NA, Stiles C, Nekolaichuk C et al (2008) The Alberta breakthrough pain assessment tool for cancer patients: a validation study using a Delphi process and patient think-aloud interviews. J Pain Symptom Manage 35:136–152. https://doi.org/10.1016/j.jpainsymman.2007.03.016
Boyer L, Pepin J, Dubois S et al (2020) Adaptation and validation of a nursing competencies framework for clinical practice on a continuum of care from childhood to adulthood: a Delphi study. Nurse Educ Today 93:104530. https://doi.org/10.1016/j.nedt.2020.104530
Sinha IP, Smyth RL, Williamson PR (2011) Using the Delphi technique to determine which outcomes to measure in clinical trials: recommendations for the future based on a systematic review of existing studies. PLoS Med 8:e1000393. https://doi.org/10.1371/journal.pmed.1000393
Qualtrics (2020) Qualtrics XM
Weiner BJ, Lewis CC, Stanick C et al (2017) Psychometric assessment of three newly developed implementation outcome measures. Implement Sci 12:108. https://doi.org/10.1186/s13012-017-0635-3
Schmitz KH (2011) Exercise for secondary prevention of breast cancer: moving from evidence to changing clinical practice. Cancer Prev Res 4:476–480. https://doi.org/10.1158/1940-6207.capr-11-0097
Mazo C, Kearns C, Mooney C, Gallagher WM (2020) Clinical decision support systems in breast cancer: a systematic review. Cancers (Basel) 12
Hardcastle SJ, Kane R, Chivers P et al (2018) Knowledge, attitudes, and practice of oncologists and oncology health care providers in promoting physical activity to cancer survivors: an international survey. Support Care Cancer 26:3711–3719. https://doi.org/10.1007/s00520-018-4230-1
Yang DD, Hausien O, Aqeel M et al (2017) Physical activity levels and barriers to exercise referral among patients with cancer. Patient Educ Couns 100:1402–1407. https://doi.org/10.1016/j.pec.2017.01.019
Jyothi NS, Parkavi A (2016) A study on task management system. In: International Conference on Research Advances in Integrated Navigation Systems (RAINS) 2016, pp 1–6. https://doi.org/10.1109/RAINS.2016.7764421
Bratterud H, Burgess M, Fasy BT, et al (2020) The Sung diagram: revitalizing the Eisenhower matrix. In: Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). Springer, pp 498–502
Kleynen M, Braun SM, Bleijlevens MH et al (2014) Using a Delphi technique to seek consensus regarding definitions, descriptions and classification of terms related to implicit and explicit forms of motor learning. PLoS ONE 9. https://doi.org/10.1371/journal.pone.0100227
Vogel C, Zwolinsky S, Griffiths C et al (2019) A Delphi study to build consensus on the definition and use of big data in obesity research. Int J Obes 43:2573–2586. https://doi.org/10.1038/s41366-018-0313-9
Fong AJ, Sabiston CM, Nadler MB, Sussman J, Langley H, Holden R, Stokes-Noonan M, Tomasone JR (2021) Development of an evidence-informed recommendation guide to facilitate physical activity counseling between oncology care providers and patients in Canada. Transl Behav Med 11(4):930–940. https://doi.org/10.1093/tbm/ibaa127
Gonzalez BD (2018) Promise of mobile health technology to reduce disparities in patients with cancer and survivors. JCO Clin Cancer Informatics 1–9. https://doi.org/10.1200/CCI.17.00141
Dicker AP, Jim HSL (2018) Intersection of digital health and oncology. JCO Clin cancer informatics 2:1–4. https://doi.org/10.1200/CCI.18.00070
Acknowledgements
We would like to thank additional members of the American Congress of Rehabilitation Medicine’s Cancer Rehabilitation Networking Group for their contributions and support. We would also like to thank Dr. Catherine Alfano for her role in algorithm development, and the following colleagues for their help with recruitment: Dr. Michelle Nadler, Dr. Terence Pugh, Dr. Michael Stubblefield, and Dr. Keith Thraen-Borowski.
Funding
Dr. Williams is supported in part by the National Cancer Institute of the National Institutes of Health (K08CA234225). The authors declare no additional funds, grants or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Dr. Wood led all aspects of the study as PhD dissertation. Drs. Pergolotti, Sharp, Leach, and Bundy served as dissertation committee members and reviewed and advised the study at each stage. The remaining authors participated in algorithm development or assisted with recruitment and aspects of study design.
Corresponding author
Ethics declarations
Ethics approval
The Colorado State University Institutional Review Board has declared the study as exempt from review (protocol #: 20-10145H).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
N/A
Competing interests
Authors, Wood, Pergolotti, and Kendig receive salaries from Select Medical. The remaining authors have no relevant financial or non-financial interested to disclose. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wood, K.C., Pergolotti, M., Marshall, T. et al. Usability, acceptability, and implementation strategies for the Exercise in Cancer Evaluation and Decision Support (EXCEEDS) algorithm: a Delphi study. Support Care Cancer 30, 7407–7418 (2022). https://doi.org/10.1007/s00520-022-07164-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07164-6