Abstract
Purpose
Lung cancer (LC) is a highly prevalent disease with more survivors diagnosed and treated at earlier stages. There is a need to understand psychological and lifestyle behavior needs to design interventions for this population. Furthermore, understanding the needs and role of family caregivers, especially given the risks associated with second-hand smoke, is needed.
Methods
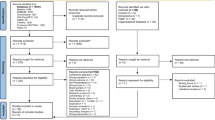
Thirty-one early-stage (stages I or IIA) LC survivors of (52% men) and 22 (50% women) caregivers (N = 53 total) completed surveys after surgery (baseline) and at 3- and 6-month follow-ups. Participants reported on psychological functioning, smoking, and physical activity (PA) as well as intervention preferences.
Results
Survivors reported low levels of psychological distress and 3% were current smokers during the study. Approximately 79% were sedentary and not meeting national PA guidelines. Caregivers also reported minimal psychological distress and were sedentary (62% not meeting guidelines), but a larger proportion continued to smoke following the survivor’s cancer diagnosis (14%). Both survivors and caregivers expressed interest in home-based PA interventions but differed regarding preferred format for delivery. Most (64%) caregivers preferred a dyadic format, where survivors and caregivers participate in the intervention together. However, most survivors preferred an individual or group format (57%) for intervention delivery.
Conclusion
Both LC survivors and family caregivers could benefit from PA interventions, and flexible, dyadic interventions could additionally support smoking cessation for family caregivers.

Similar content being viewed by others
Data availability
The corresponding author has full control of all primary data and will allow the journal to review the data if requested.
References
American Cancer Society (2019) Cancer facts and figures. In: Editor (eds) Book Cancer facts and figures. American Cancer Society, City
Howlader N, Noone A, Krapcho M, Miller D, Bishop K, Kosary C, Yu M, Ruhl J, Tatalovich Z, Mariotto A (2017) SEER cancer statistics review, 1975-2014. National Cancer Institute, Bethesda
Eberhardt W, Albain KS, Pass H, Putnam JB, Gregor A, Assamura H, Mornex F, Senan S, Belderbos J, Westeel V (2003) Induction treatment before surgery for non-small cell lung cancer. Lung Cancer 42:9–14
Carmack Taylor C, Badr H, Lee J, Fossella F, Pisters K, Gritz E, Schover L (2008) Lung cancer patients and their spouses: psychological and relationship functioning within 1 month of treatment initiation. Ann Behav Med 36:129–140
Bellizzi KM, Rowland JH, Jeffery DD, McNeel T (2005) Health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol 23:8884–8893
Richardson GE, Tucker MA, Venzon DJ, Linnoila RI, Phelps R, Phares JC, Edison M, Ihde DC, Johnson BE (1993) Smoking cessation after successful treatment of small-cell lung cancer is associated with fewer smoking-related second primary cancers. Ann Intern Med 119:383–390
Berg CJ, Thomas AN, Mertens AC, Schauer GL, Pinsker EA, Ahluwalia JS, Khuri FR (2013) Correlates of continued smoking versus cessation among survivors of smoking-related cancers. Psycho-Oncology 22:799–806
Walker MS, Vidrine DJ, Gritz ER, Larsen RJ, Yan Y, Govindan R, Fisher EB (2006) Smoking relapse during the first year after treatment for early-stage non–small-cell lung cancer. Cancer Epidemiol Biomark Prev 15:2370–2377
Emmons KM, McBride CM, Pulo E, Ollack KI, Clilpp E, Kuntz K, Marcus BH, Napolitano M, Onken J, Farraye F, Fletcher R (2005) Project PREVENT: a randomized trial to reduce multiple behavioral risk factors for colon cancer. Cancer Epidemiol 14:1453–1459
Coups EJ, Park BJ, Feinstein MB, Steingart RM, Egleston BL, Wilson DJ, Ostroff JS (2009) Physical activity among lung cancer survivors: changes across the cancer trajectory and associations with quality of life. Cancer Epidemiol Biomark Prev 18:664–672
Conn VS, Hafdahl AR, Porock DC, McDaniel R, Nielsen PJ (2006) A meta-analysis of exercise interventions among people treated for cancer. Support Care Cancer 14:699–712
Schmitz KH, Holtzman J, Courneya KS, Mâsse LC, Duval S, Kane R (2005) Controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. Cancer Epidemiol Biomark Prev 14:1588–1595
Badr H, Smith CB, Goldstein NE, Gomez JE, Redd WH (2015) Dyadic psychosocial intervention for advanced lung cancer patients and their family caregivers: results of a randomized pilot trial. Cancer 121:150–158
Blok AC, Blonquist TM, Nayak MM, Somayaji D, Crouter SE, Hayman LL, Colson YL, Bueno R, Emmons KM, Cooley ME (2018) Feasibility and acceptability of “healthy directions” a lifestyle intervention for adults with lung cancer. Psycho-Oncology 27:250–257
Marcus BH, Lewis BA, Hogan J, King TK, Albrecht AE, Bock B, Parisi AF, Niaura R, Abrams DB (2005) The efficacy of moderate-intensity exercise as an aid for smoking cessation in women: a randomized controlled trial. Nicotine Tob Res 7:871–880
Hall SM, Tunstall CD, Vila KL, Duffy J (1992) Weight gain prevention and smoking cessation: cautionary findings. Am J Public Health 82:799–803
Pirie PL, McBride CM, Hellerstedt W, Jeffery RW, Hatsukami D, Allen S, Lando H (1992) Smoking cessation in women concerned about weight. Am J Public Health 82:1238–1243
Ussher MH, Taylor A, Faulkner G (2012) Exercise interventions for smoking cessation. Cochrane Database Syst Rev 1
Mosher CE, Bakas T, Champion VL (2013) Physical health, mental health, and life changes among family caregivers of patients with lung cancer.(Article)(Report). Oncol Nurs Forum 40:53–61
Weaver KE, Rowland JH, Augustson E, Atienza AA (2011) Smoking concordance in lung and colorectal cancer patient-caregiver dyads and quality of life. Cancer Epidemiol Biomark Prev 20:239–248
Rha SY, Park Y, Song SK, Lee CE, Lee J (2015) Caregiving burden and health-promoting behaviors among the family caregivers of cancer patients. Eur J Oncol Nurs 19:174–181
Hewat RJ, Ellis DJ (1986) Similarities and differences between women who breastfeed for short and long duration. Midwifery 2:37–43
Wilson SE (2002) The health capital of families: an investigation of the inter-spousal correlation in health status. Soc Sci Med 55:1157–1172
Homish GG, Leonard KE (2005) Spousal influence on smoking behaviors in a US community sample of newly married couples. Soc Sci Med 61:2557–2567
Mendoza TR, Wang XS, Lu C, Palos GR, Liao Z, Mobley GM, Kapoor S, Cleeland CS (2011) Measuring the symptom burden of lung cancer: the validity and utility of the lung cancer module of the M. D. Anderson Symptom Inventory. Oncologist 16:217–227
Schalet BD, Pilkonis PA, Yu L, Dodds N, Johnston KL, Yount S, Riley W, Cella D (2016) Clinical validity of PROMIS depression, anxiety, and anger across diverse clinical samples. J Clin Epidemiol 73:119–127
Christianson SMJ (2012) The Impact of Event Scale - Revised (IES-R), Medsurg Nurs 21
Godin G, Shephard R (1985) A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 10:141–146
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, Olson RD (2018) The physical activity guidelines for Americans. Jama 320:2020–2028
Ryan RM, Deci EL (2000)Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 55:68–78
Williams GC, Freedman ZR, Deci EL (1998) Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care 21:1644–1651
Levesque C, Williams GC, Elliot D, Pickering MA, Bodenhamer B, Finley PJ (2007) Validating the theoretical structure of the treatment self- regulation questionnaire (TSRQ) across three different health behaviors. Health Educ Res 22:691–702
Williams GC, McGregor H, Sharp D, Kouides RW, Levesque CS, Ryan RM, Deci EL (2006) A self-determination multiple risk intervention trial to improve smokers’ health, J Gen Intern Med
Ottenbacher AJ, Day RS, Taylor WC, Sharma SV, Sloane R, Snyder DC, Kraus WE, Demark-Wahnefried W (2011) Exercise among breast and prostate cancer survivors—what are their barriers? J Cancer Surviv 5:413–419
Blaney JM, Lowe-Strong A, Rankin-Watt J, Campbell A, Gracey JH (2013) Cancer survivors’ exercise barriers, facilitators and preferences in the context of fatigue, quality of life and physical activity participation: a questionnaire-survey. Psychooncology 22:186–194
Trinidad DR, Pérez-Stable EJ, White MM, Emery SL, Messer K (2011) A nationwide analysis of US racial/ethnic disparities in smoking behaviors, smoking cessation, and cessation-related factors. Am J Public Health 101:699–706
Cesario A, Ferri L, Galetta D, Pasqua F, Bonassi S, Clini E, Biscione G, Cardaci V, di Toro S, Zarzana A, Margaritora S, Piraino A, Russo P, Sterzi S, Granone P (2007)Post-operative respiratory rehabilitation after lung resection for non-small cell lung cancer. Lung Cancer 57:175–180
Nightingale CL, Steffen LE, Tooze JA, Petty W, Danhauer SC, Badr H, Weaver KE (2019) Lung cancer patient and caregiver health vulnerabilities and interest in health promotion interventions: an exploratory study. Glob Adv Health Med 8
Cooley EM, Finn TK, Wang PQ, Roper LK, Morones LS, Shi LL, Litrownik LD, Marcoux LJ, Zaner LK, Hayman LL (2013) Health behaviors, readiness to change, and interest in health promotion programs among smokers with lung cancer and their family members: a pilot study. Cancer Nurs 36:145–154
Milbury K, Chaoul A, Engle R, Liao Z, Yang C, Carmack C, Shannon V, Spelman A, Wangyal T, Cohen L (2015)Couple-based Tibetan yoga program for lung cancer patients and their caregivers. Psychooncology 24:117–120
Milbury K, Mallaiah S, Lopez G, Liao Z, Yang C, Carmack C, Chaoul A, Spelman A, Cohen L (2015) Vivekananda yoga program for patients with advanced lung cancer and their family caregivers. Integr Cancer Ther 14:446–451
Bendixen M, Jørgensen OD, Kronborg C, Andersen C, Licht PB (2016) Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol 17:836–844
Demmy TL, Nwogu C (2008) Is video-assisted thoracic surgery lobectomy better? Quality of life considerations. Ann Thorac Surg 85:S719–S728
Ellis L, Canchola AJ, Spiegel D, Ladabaum U, Haile R, Gomez SL (2018) Racial and ethnic disparities in cancer survival: the contribution of tumor, sociodemographic, institutional, and neighborhood characteristics. J Clin Oncol 36:25–33
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Badr and Flores and Ms. Roddy declare that they have no conflict of interest.
Dr. Burt reports a financial relationship with Bayou Surgical Equity and I.P. and grants from Momotero-gene, outside the submitted work.
Informed consent
All persons gave their informed consent prior to their inclusion in the study.
Involving human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roddy, M.K., Flores, R.M., Burt, B. et al. Lifestyle behaviors and intervention preferences of early-stage lung cancer survivors and their family caregivers. Support Care Cancer 29, 1465–1475 (2021). https://doi.org/10.1007/s00520-020-05632-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05632-5