Abstract
Purpose
Approximately one in two cancer patients globally are under-treated for pain. Opioids and other analgesics represent the mainstay of cancer pain management; however, barriers to their use are well-documented. We evaluated whether acupuncture would be a preferable treatment option among cancer patients with attitudinal barriers to pharmacological pain management.
Methods
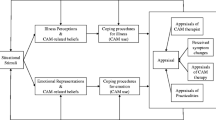
We conducted a cross-sectional survey of cancer patients at a tertiary urban cancer center and eleven suburban/rural hospitals in the Northeastern United States. We assessed attitudinal barriers to pharmacological pain management with the Barriers Questionnaire (BQ-13). The BQ-13 consists of two subscales: pain management beliefs and analgesic side effects. We also asked patients whether they prefer acupuncture, analgesics, or have no preference between these two modalities for pain management. Covariates included sociodemographics, clinical characteristics, and attitudes/beliefs about acupuncture. We used logistic regression to examine the association between attitudinal barriers and acupuncture preference.
Results
Among 628 patients, 197 (31.4%) preferred acupuncture for pain management, 146 (23.3%) preferred analgesics, and 285 (45.4%) had no preference. The highest reported attitudinal barriers were fear of addiction and fear of analgesic-associated constipation and nausea. Adjusting for covariates, we found that attitudinal barriers related to fear of analgesic side effects were significantly associated with acupuncture preference (adjusted odds ratio [AOR] 1.45, 95% confidence interval [CI] 1.17–1.81), but barriers related to pain management beliefs were not (AOR 1.17, 95% CI 0.91–1.51). Attitudes/beliefs about acupuncture (i.e., greater expected benefits, fewer perceived barriers, and more positive social norms) and female gender also predicted acupuncture preference, whereas race and educational status did not.
Conclusion
Acupuncture may be a preferable treatment option among cancer patients at risk of inadequately controlled pain due to fear of analgesic side effects. Evidence-based integration of acupuncture and analgesics, guided by patient treatment preferences, represents an essential aspect of patient-centered care and has potential to address unmet cancer pain management needs.
Similar content being viewed by others
Data availability
Dr. Jun J. Mao has full control of all primary data and agrees to allow the journal to review the data if requested.
References
Zylla D, Steele G, Gupta P (2017) A systematic review of the impact of pain on overall survival in patients with cancer. Support Care Cancer 25(5):1687–1698. https://doi.org/10.1007/s00520-017-3614-y
Deandrea S, Montanari M, Moja L, Apolone G (2008) Prevalence of undertreatment in cancer pain. A review of published literature. Ann Oncol 19(12):1985–1991. https://doi.org/10.1093/annonc/mdn419
Scarborough BM, Smith CB (2018) Optimal pain management for patients with cancer in the modern era. CA Cancer J Clin 68(3):182–196. https://doi.org/10.3322/caac.21453
Gunnarsdottir S, Sigurdardottir V, Kloke M, Radbruch L, Sabatowski R, Kaasa S, Klepstad P (2017) A multicenter study of attitudinal barriers to cancer pain management. Support Care Cancer 25(11):3595–3602. https://doi.org/10.1007/s00520-017-3791-8
Weiss SC, Emanuel LL, Fairclough DL, Emanuel EJ (2001) Understanding the experience of pain in terminally ill patients. Lancet 357(9265):1311–1315. https://doi.org/10.1016/s0140-6736(00)04515-3
Bulls HW, Hoogland AI, Craig D, Paice J, Chang YD, Oberoi-Jassal R, Rajasekhara S, Haas M, Bobonis M, Gonzalez BD, Portman D, Jim HSL (2019) Cancer and Opioids: Patient Experiences With Stigma (COPES)-a pilot study. J Pain Symptom Manag 57(4):816–819. https://doi.org/10.1016/j.jpainsymman.2019.01.013
Volkow ND, Icaza MEM, Poznyak V, Saxena S, Gerra G (2019) Addressing the opioid crisis globally. World Psychiatry 18(2):231–232. https://doi.org/10.1002/wps.20633
Morley KI, Ferris JA, Winstock AR, Lynskey MT (2017) Polysubstance use and misuse or abuse of prescription opioid analgesics: a multi-level analysis of international data. Pain 158(6):1138–1144. https://doi.org/10.1097/j.pain.0000000000000892
Adam R, Bond C, Murchie P (2015) Educational interventions for cancer pain. A systematic review of systematic reviews with nested narrative review of randomized controlled trials. Patient Educ Couns 98(3):269–282. https://doi.org/10.1016/j.pec.2014.11.003
Oldenmenger WH, Geerling JI, Mostovaya I, Vissers KCP, de Graeff A, Reyners AKL, van der Linden YM (2018) A systematic review of the effectiveness of patient-based educational interventions to improve cancer-related pain. Cancer Treat Rev 63:96–103. https://doi.org/10.1016/j.ctrv.2017.12.005
Oldenmenger WH, Sillevis Smitt PA, van Dooren S, Stoter G, van der Rijt CC (2009) A systematic review on barriers hindering adequate cancer pain management and interventions to reduce them: a critical appraisal. Eur J Cancer 45(8):1370–1380. https://doi.org/10.1016/j.ejca.2009.01.007
Paice JA, Portenoy R, Lacchetti C, Campbell T, Cheville A, Citron M, Constine LS, Cooper A, Glare P, Keefe F, Koyyalagunta L, Levy M, Miaskowski C, Otis-Green S, Sloan P, Bruera E (2016) Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 34(27):3325–3345. https://doi.org/10.1200/JCO.2016.68.5206
Non-medical treatments for pain. American Cancer Society. https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/pain/non-medical-treatments-for-cancer-pain.html. Accessed July 15, 2018
Clinical practice guidelines in oncology: adult cancer pain. National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/pdf/pain.pdf. Accessed July 15, 2018
Yun H, Sun L, Mao JJ (2017) Growth of integrative medicine at leading cancer centers between 2009 and 2016: a systematic analysis of NCI-designated comprehensive cancer center websites. J Natl Cancer Inst Monogr 2017(52). https://doi.org/10.1093/jncimonographs/lgx004
Grant SJ, Hunter J, Seely D, Balneaves LG, Rossi E, Bao T (2019) Integrative oncology: international perspectives. Integrative Cancer Ther 18:1534735418823266. https://doi.org/10.1177/1534735418823266
Lim MY, Huang J, Zhao B, Ha L (2015) Current status of acupuncture and moxibustion in China. Chin Med 10:12. https://doi.org/10.1186/s13020-015-0041-1
Vickers AJ, Cronin AM, Maschino AC, Lewith G, MacPherson H, Foster NE, Sherman KJ, Witt CM, Linde K, Acupuncture Trialists C (2012) Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med 172(19):1444–1453. https://doi.org/10.1001/archinternmed.2012.3654
Zia FZ, Olaku O, Bao T, Berger A, Deng G, Yin Fan A, Garcia MK, Herman PM, Kaptchuk TJ, Ladas EJ, Langevin HM, Lao L, Lu W, Napadow V, Niemtzow RC, Vickers AJ, Shelley Wang X, Witt CM, Mao JJ (2017) The National Cancer Institute’s conference on acupuncture for symptom management in oncology: state of the science, evidence, and research gaps. J Natl Cancer Inst Monogr 2017(52). https://doi.org/10.1093/jncimonographs/lgx005
Vickers AJ, Vertosick EA, Lewith G, MacPherson H, Foster NE, Sherman KJ, Irnich D, Witt CM, Linde K, Acupuncture Trialists C (2018) Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain 19(5):455–474. https://doi.org/10.1016/j.jpain.2017.11.005
Hershman DL, Unger JM, Greenlee H, Capodice JL, Lew DL, Darke AK, Kengla AT, Melnik MK, Jorgensen CW, Kreisle WH, Minasian LM, Fisch MJ, Henry NL, Crew KD (2018) Effect of acupuncture vs sham acupuncture or waitlist control on joint pain related to aromatase inhibitors among women with early-stage breast cancer: a randomized clinical trial. JAMA 320(2):167–176. https://doi.org/10.1001/jama.2018.8907
Mao JJ, Palmer CS, Healy KE, Desai K, Amsterdam J (2011) Complementary and alternative medicine use among cancer survivors: a population-based study. J Cancer Survivorship : Res Pract 5(1):8–17. https://doi.org/10.1007/s11764-010-0153-7
Hopton A, Thomas K, MacPherson H (2013) The acceptability of acupuncture for low back pain: a qualitative study of patient's experiences nested within a randomised controlled trial. PLoS One 8(2):e56806. https://doi.org/10.1371/journal.pone.0056806
Bishop FL, Barlow F, Coghlan B, Lee P, Lewith GT (2011) Patients as healthcare consumers in the public and private sectors: a qualitative study of acupuncture in the UK. BMC Health Serv Res 11:129. https://doi.org/10.1186/1472-6963-11-129
Zhang Y, Lao L, Chen H, Ceballos R (2012) Acupuncture use among American adults: what acupuncture practitioners can learn from National Health Interview Survey 2007? Evid Based Complement Alternat Med 2012:710750–710758. https://doi.org/10.1155/2012/710750
Dalal S, Bruera E (2013) Access to opioid analgesics and pain relief for patients with cancer. Nat Rev Clin Oncol 10(2):108–116. https://doi.org/10.1038/nrclinonc.2012.237
King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, Sibbald B, Lai R (2005) Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials. Health Technol Assess (Winchester, England) 9(35):1–186 iii-iv
Montori VM, Brito JP, Murad MH (2013) The optimal practice of evidence-based medicine: incorporating patient preferences in practice guidelines. JAMA 310(23):2503–2504. https://doi.org/10.1001/jama.2013.281422
Boyd-Seale D, Wilkie DJ, Kim YO, Suarez ML, Lee H, Molokie R, Zhao Z, Zong S (2010) Pain barriers: psychometrics of a 13-item questionnaire. Nurs Res 59(2):93–101. https://doi.org/10.1097/NNR.0b013e3181d1a6de
Stein KD, Alcaraz KI, Kamson C, Fallon EA, Smith TG (2016) Sociodemographic inequalities in barriers to cancer pain management: a report from the American Cancer Society’s Study of Cancer Survivors-II (SCS-II). Psycho-oncology 25(10):1212–1221. https://doi.org/10.1002/pon.4218
Meghani SH, Thompson AM, Chittams J, Bruner DW, Riegel B (2015) Adherence to analgesics for cancer pain: a comparative study of African Americans and Whites using an electronic monitoring device. J Pain 16(9):825–835. https://doi.org/10.1016/j.jpain.2015.05.009
Mao JJ, Palmer SC, Desai K, Li SQ, Armstrong K, Xie SX (2012) Development and validation of an instrument for measuring attitudes and beliefs about complementary and alternative medicine (CAM) use among cancer patients. Evid Based Complement Alternat Med 2012:798098–798098. https://doi.org/10.1155/2012/798098
He Y, Guo X, May BH, Zhang AL, Liu Y, Lu C, Mao JJ, Xue CC, Zhang H (2019) Clinical evidence for association of acupuncture and acupressure with improved cancer pain: a systematic review and meta-analysis. JAMA Oncol 6:271. https://doi.org/10.1001/jamaoncol.2019.5233
Paley CA, Johnson MI, Tashani OA, Bagnall AM (2015) Acupuncture for cancer pain in adults. Cochrane Database System Rev 10:Cd007753. https://doi.org/10.1002/14651858.CD007753.pub3
Chiu HY, Hsieh YJ, Tsai PS (2017) Systematic review and meta-analysis of acupuncture to reduce cancer-related pain. Euro J Cancer Care 26(2). https://doi.org/10.1111/ecc.12457
Deng G, Bao T, Mao JJ (2018) Understanding the benefits of acupuncture treatment for cancer pain management. Oncology (Williston Park, NY) 32(6):310–316
Lu W, Rosenthal DS (2010) Recent advances in oncology acupuncture and safety considerations in practice. Curr Treat Options in Oncol 11(3–4):141–146. https://doi.org/10.1007/s11864-010-0126-0
Judson PL, Abdallah R, Xiong Y, Ebbert J, Lancaster JM (2017) Complementary and alternative medicine use in individuals presenting for care at a comprehensive cancer center. Integrative Cancer Ther 16(1):96–103. https://doi.org/10.1177/1534735416660384
The use of complementary and alternative medicine in the United States. The National Center for Integrative and Complementary Health https://nccih.nih.gov/sites/nccam.nih.gov/files/camuse.pdf. Accessed August 24, 2018
Bartley EJ, Fillingim RB (2013) Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth 111(1):52–58. https://doi.org/10.1093/bja/aet127
Paller CJ, Campbell CM, Edwards RR, Dobs AS (2009) Sex-based differences in pain perception and treatment. Pain Med (Malden, Mass) 10(2):289–299. https://doi.org/10.1111/j.1526-4637.2008.00558.x
Valeberg BT, Miaskowski C, Hanestad BR, Bjordal K, Moum T, Rustoen T (2008) Prevalence rates for and predictors of self-reported adherence of oncology outpatients with analgesic medications. Clin J Pain 24(7):627–636. https://doi.org/10.1097/AJP.0b013e31816fe020
Cleeland CS, Gonin R, Hatfield AK, Edmonson JH, Blum RH, Stewart JA, Pandya KJ (1994) Pain and its treatment in outpatients with metastatic cancer. N Engl J Med 330(9):592–596. https://doi.org/10.1056/nejm199403033300902
Kligler B, Buonora M, Gabison J, Jacobs E, Karasz A, McKee MD (2015) “I felt like it was God’s hands putting the needles in”: a qualitative analysis of the experience of acupuncture for chronic pain in a low-income, ethnically diverse, and medically underserved patient population. J Alternative Complement Med (New York, NY) 21(11):713–719. https://doi.org/10.1089/acm.2014.0376
McKee MD, Kligler B, Blank AE, Fletcher J, Jeffres A, Casalaina W, Biryukov F (2012) The ADDOPT study (Acupuncture to Decrease Disparities in Outcomes of Pain Treatment): feasibility of offering acupuncture in the community health center setting. J Alternative Complement Med (New York, NY) 18(9):839–843. https://doi.org/10.1089/acm.2011.0193
Chao MT, Schillinger D, Nguyen U, Santana T, Liu R, Gregorich S, Hecht FM (2019) A randomized clinical trial of group acupuncture for painful diabetic neuropathy among diverse safety net patients. Pain medicine (Malden, Mass). doi:https://doi.org/10.1093/pm/pnz117
Liou KT, Hung TKW, Meghani SH, Epstein AS, Li QS, Romero SAD, Cohen RB, Mao JJ (2019) What if acupuncture were covered by insurance for pain management? A cross-sectional study of cancer patients at one academic center and 11 community hospitals. Pain medicine (Malden, Mass). doi:https://doi.org/10.1093/pm/pnz087
Meghani SH, Byun E, Gallagher RM (2012) Time to take stock: a meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med (Malden, Mass) 13(2):150–174. https://doi.org/10.1111/j.1526-4637.2011.01310.x
Meghani SH, Kang Y, Chittams J, McMenamin E, Mao JJ, Fudin J (2014) African Americans with cancer pain are more likely to receive an analgesic with toxic metabolite despite clinical risks: a mediation analysis study. J Clin Oncol 32(25):2773–2779. https://doi.org/10.1200/jco.2013.54.7992
Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH (2017) Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database System Rev 4:Cd011279. https://doi.org/10.1002/14651858.CD011279.pub3
Garland EL, Brintz CE, Hanley AW, Roseen EJ, Atchley RM, Gaylord SA, Faurot KR, Yaffe J, Fiander M, Keefe FJ (2019) Mind-body therapies for opioid-treated pain: a systematic review and meta-analysis. JAMA Intern Med 180:91. https://doi.org/10.1001/jamainternmed.2019.4917
Sindt JE, Brogan SE (2016) Interventional treatments of cancer pain. Anesthesiol Clin 34(2):317–339. https://doi.org/10.1016/j.anclin.2016.01.004
Weeks J (2016) Influential U.S. medical organizations call for insurance coverage of non-pharmacologic approaches to pain. J Alternative Complement Med (New York, NY) 22(12):947–949. https://doi.org/10.1089/acm.2016.29016.jjw
National Association of Attorneys General - joint letter to America’s health insurance plans re: prescription opioid epidemic. (September 18, 2017). http://www.naag.org/naag/media/naag-news/attorneys-general-urge-health-insurance-companies-to-reduce-provider-incentives-for-prescribing-pain-killers.php. Accessed August 23, 2018
Pain management best practices inter-agency task force report: updates, gaps, inconsistencies, and recommendations. Retrieved from U. S. Department of Health and Human Services website: https://www.hhs.gov/ash/advisory-committees/pain/reports/index.html. Report published on May 9, 2019
Kwon JH (2014) Overcoming barriers in cancer pain management. J Clin Oncol 32(16):1727–1733. https://doi.org/10.1200/jco.2013.52.4827
Acknowledgments
The authors would like to thank the patients, oncologists, nurses, and clinical staff at all study sites for their contributions to this study.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent official views of the National Institutes of Health.
Funding
Research related to the development of this paper was supported in part by the National Cancer Institute grants to the University of Pennsylvania Abramson Cancer Center (2P30CA016520-40) and the Memorial Sloan Kettering Cancer Center (3P30CA008748-50), the Byrne Fund, and the Translational and Integrative Medicine Research Fund at Memorial Sloan Kettering Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Jun J. Mao reports grants from Tibet Cheezheng Tibetan Medicine Co., Ltd. and Zhongke Health International LLC for work unrelated to this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liou, K.T., Trevino, K.M., Meghani, S.H. et al. Fear of analgesic side effects predicts preference for acupuncture: a cross-sectional study of cancer patients with pain in the USA. Support Care Cancer 29, 427–435 (2021). https://doi.org/10.1007/s00520-020-05504-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05504-y