Abstract
Purpose
Sarcopenia is increasingly recognized as an independent risk factor for poor outcomes in patients undergoing hematopoietic stem cell transplantation (HSCT), and it is a potentially modifiable factor. The purpose of the present systematic review and meta-analysis is to summarize and integrate current evidence in this field.
Methods
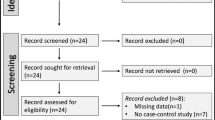
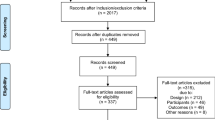
We searched EMBASE, MEDLINE, and Cochrane DSR through Ovid and PubMed websites to identify relevant studies. Studies evaluated sarcopenia before HSCT and reported associations between sarcopenia and post-transplant outcomes were included. Two authors independently applied eligibility criteria, assessed quality, and extracted data. Odds ratio (OR) and their 95% confidence intervals (CIs) were pooled to examine the association between sarcopenia and post-transplant outcomes by using the review manager 5.3 software.
Results
Seven retrospective cohort studies met our inclusion criteria. The overall quality of studies was low to moderate. Sarcopenia was associated with higher non-relapse mortality [odds ratio (OR) 1.97; 95% CI 1.45, 2.68; P < 0.0001; I2 = 0%] and shorter overall survival [odds ratio (OR) 0.44; 95% CI 0.26, 0.75; P = 0.002; I2 = 65%] in patients undergoing HSCT.
Conclusions
Clinicians could use sarcopenia to balance the risks and benefits of transplantation as early as possible; in addition, interventions can be used to prevent sarcopenia and improve physical function and quality of life. Well-designed, prospective, and large-scale clinical studies are needed to consolidate the evidence.



Similar content being viewed by others
References
Ljungman P, Bregni M, Brune M, Cornelissen J, de Witte T, Dini G, Einsele H, Gaspar HB, Gratwohl A, Passweg J, Peters C, Rocha V, Saccardi R, Schouten H, Sureda A, Tichelli A, Velardi A, Niederwieser D, European Group for Blood and Marrow Transplantation (2010) Allogeneic and autologous transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe 2009. Bone Marrow Transplant 45(2):219–234. https://doi.org/10.1038/bmt.2009.141
Passweg JR, Baldomero H, Bader P, Bonini C, Cesaro S, Dreger P, Duarte RF, Dufour C, Kuball J, Farge-Bancel D, Gennery A, Kröger N, Lanza F, Nagler A, Sureda A, Mohty M (2016) Hematopoietic stem cell transplantation in Europe 2014: more than 40 000 transplants annually. Bone Marrow Transplant 51(6):786–792. https://doi.org/10.1038/bmt.2016.20
Appelbaum FR (2008) What is the impact of hematopoietic cell transplantation (HCT) for older adults with acute myeloid leukemia (AML)? Best Pract Res Clin Haematol 21(4):667–675. https://doi.org/10.1016/j.beha.2008.06.005
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, Sandmaier B (2009) Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 15(3):367–369. https://doi.org/10.1016/j.bbmt.2008.12.497
Wingard JR, Majhail NS, Brazauskas R, Wang Z, Sobocinski KA, Jacobsohn D, Sorror ML, Horowitz MM, Bolwell B, Rizzo JD, Socié G (2011) Long-term survival and late deaths after allogeneic hematopoietic cell transplantation. J Clin Oncol 29(16):2230–2239. https://doi.org/10.1200/JCO.2010.33.7212
Ashton LJ, Le Marsney RE, Dodds AJ, Nivison-Smith I, Wilcox L, O'Brien TA et al (2014) A population-based cohort study of late mortality in adult autologous hematopoietic stem cell transplant recipients in Australia. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 20(7):937–945. https://doi.org/10.1016/j.bbmt.2014.03.006
Styczynski J, Tridello G, Koster L, Iacobelli S, van Biezen A, van der Werf S et al (2019) Death after hematopoietic stem cell transplantation: changes over calendar year time, infections and associated factors. Bone Marrow Transplant 55:126–136. https://doi.org/10.1038/s41409-019-0624-z
Cho SK, McCombs J, Punwani N, Lam J (2019) Complications and hospital costs during hematopoietic stem cell transplantation for non-Hodgkin lymphoma in the United States. Leuk Lymphoma:1–7. https://doi.org/10.1080/10428194.2019.1581932
Rivera-Franco MM, Leon-Rodriguez E, Castro-Saldana HL (2017) Costs of hematopoietic stem cell transplantation in a developing country. Int J Hematol 106(4):573–580. https://doi.org/10.1007/s12185-017-2278-1
Wais V, Bunjes D, Kuchenbauer F, Sorror ML (2018) Comorbidities, age, and other patient-related predictors of allogeneic hematopoietic cell transplantation outcomes. Expert Rev Hematol 11(10):805–816. https://doi.org/10.1080/17474086.2018.1509703
Dent E, Morley JE, Cruz-Jentoft AJ, Arai H, Kritchevsky SB, Guralnik J et al (2018) International Clinical Practice Guidelines for Sarcopenia (ICFSR): screening, diagnosis and management. The journal of nutrition, health & aging 22(10):1148–1161. https://doi.org/10.1007/s12603-018-1139-9
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age and ageing 48(1):16–31. https://doi.org/10.1093/ageing/afy169.
Daly LE, Ryan AM, Power DG (2016) Response to “Loss of muscle mass during chemotherapy is predictive for poor survival of patients with metastatic colorectal cancer”. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 34(31):3816–3817. https://doi.org/10.1200/jco.2016.68.8010
Nakamura N, Hara T, Shibata Y, Matsumoto T, Nakamura H, Ninomiya S, Kito Y, Kitagawa J, Kanemura N, Goto N, Shiraki M, Miyazaki T, Takeuchi T, Shimizu M, Tsurumi H (2015) Sarcopenia is an independent prognostic factor in male patients with diffuse large B-cell lymphoma. Ann Hematol 94(12):2043–2053. https://doi.org/10.1007/s00277-015-2499-4
Yang M, Shen Y, Tan L, Li W (2019) Prognostic value of sarcopenia in lung cancer: a systematic review and meta-analysis. Chest. 156(1):101–111. https://doi.org/10.1016/j.chest.2019.04.115
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62(10):1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons; 2011
Lo CK, Mertz D, Loeb M (2014) Newcastle-Ottawa scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol 14:45. https://doi.org/10.1186/1471-2288-14-45
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ (Clinical research ed) 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Ando T, Fujisawa S, Sakuma T, Teshigawara H, Matsumura A, Suzuki T et al (2017) Value of computed tomography-defined sarcopenia: a prognostic predictor of non-relapse mortality following allogeneic hematopoietic stem cell transplantation in patients with acute myeloid leukemia and myelodysplastic syndrome. Blood 130(Supplement 1):4562–. https://doi.org/10.1182/blood.V130.Suppl_1.4562.4562.
Armenian SH, Xiao M, Berano Teh J, Lee B, Chang HA, Mascarenhas K et al (2019) Impact of sarcopenia on adverse outcomes after allogeneic hematopoietic cell transplantation. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djy231
Caram MV, Bellile EL, Englesbe MJ, Terjimanian M, Wang SC, Griggs JJ, Couriel D (2015) Sarcopenia is associated with autologous transplant-related outcomes in patients with lymphoma. Leuk Lymphoma 56(10):2855–2862. https://doi.org/10.3109/10428194.2015.1014359
DeFilipp Z, Troschel FM, Qualls DA, Li S, Kuklinski MW, Kempner ME et al (2018) Evolution of body composition following autologous and allogeneic hematopoietic cell transplantation: incidence of sarcopenia and association with clinical outcomes. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation 24(8):1741–1747. https://doi.org/10.1016/j.bbmt.2018.02.016
Kim SJ, Kim Y, Hwang DY, Hyun SY, Jang JE, Lee JY et al (2013) Low psoas muscle/BMI ratio is a bad prognostic index of non-relapse survival after allogeneic stem cell transplantation. Blood Conference: 55th Annual Meeting of the American Society of Hematology, ASH 122:21
Kurosawa S, Takeuchi Y, Matsui M, Tsukada M, Iwama K, Yamada K et al (2018) Clinical impact of pre-transplant intramuscular adipose tissue content on outcome of cord blood transplantation. Blood 132(Suppl. 1). https://doi.org/10.1182/blood-2018-99-110691.
Neto AC, Del Guerra Carvalho Moraes B, Rocha IMG, Bezerra FA, Medeiros GOC, Alves LBO et al (2018) Association of sarcopenia with toxicities and survival after autologous hematopoietic stem cell transplantation for adults with lymphomas. Blood 132(Suppl. 1). https://doi.org/10.1182/blood-2018-99-117717.
Lindstrom I, Protto S, Khan N, Sillanpaa N, Hernesniemi J, Oksala N (2019) Developing sarcopenia predicts long-term mortality after elective endovascular aortic aneurysm repair. J Vasc Surg. https://doi.org/10.1016/j.jvs.2019.05.060
Jones SE, Maddocks M, Kon SS, Canavan JL, Nolan CM, Clark AL, Polkey MI, Man WD (2015) Sarcopenia in COPD: prevalence, clinical correlates and response to pulmonary rehabilitation. Thorax 70(3):213–218. https://doi.org/10.1136/thoraxjnl-2014-206440
Nakashima Y, Saeki H, Nakanishi R, Sugiyama M, Kurashige J, Oki E, Maehara Y (2018) Assessment of sarcopenia as a predictor of poor outcomes after esophagectomy in elderly patients with esophageal Cancer. Ann Surg 267(6):1100–1104. https://doi.org/10.1097/sla.0000000000002252
Yumioka T, Honda M, Nishikawa R, Teraoka S, Kimura Y, Iwamoto H, Morizane S, Hikita K, Takenaka A (2019) Sarcopenia as a significant predictive factor of neutropenia and overall survival in urothelial carcinoma patients underwent gemcitabine and cisplatin or carboplatin. Int J Clin Oncol 25:158–164. https://doi.org/10.1007/s10147-019-01544-5
Naumann P, Eberlein J, Farnia B, Hackert T, Debus J, Combs SE (2019) Continued weight loss and sarcopenia predict poor outcomes in locally advanced pancreatic cancer treated with chemoradiation. Cancers 11:5. https://doi.org/10.3390/cancers11050709
Argiles JM, Busquets S, Felipe A, Lopez-Soriano FJ (2005) Molecular mechanisms involved in muscle wasting in cancer and ageing: cachexia versus sarcopenia. Int J Biochem Cell Biol 37(5):1084–1104. https://doi.org/10.1016/j.biocel.2004.10.003
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, Abellan van Kan G, Andrieu S, Bauer J, Breuille D, Cederholm T, Chandler J, de Meynard C, Donini L, Harris T, Kannt A, Keime Guibert F, onder G, Papanicolaou D, Rolland Y, Rooks D, Sieber C, Souhami E, Verlaan S, Zamboni M (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 12(4):249–256. https://doi.org/10.1016/j.jamda.2011.01.003
Pamoukdjian F, Bouillet T, Levy V, Soussan M, Zelek L, Paillaud E (2018) Prevalence and predictive value of pre-therapeutic sarcopenia in cancer patients: a systematic review. Clinical nutrition (Edinburgh, Scotland) 37(4):1101–1113. https://doi.org/10.1016/j.clnu.2017.07.010
Han X, Kilfoy B, Zheng T, Holford TR, Zhu C, Zhu Y, Zhang Y (2008) Lymphoma survival patterns by WHO subtype in the United States, 1973-2003. Cancer causes & control : CCC 19(8):841–858. https://doi.org/10.1007/s10552-008-9147-4
Lee K, Shin Y, Huh J, Sung YS, Lee IS, Yoon KH, Kim KW (2019) Recent issues on body composition imaging for sarcopenia evaluation. Korean J Radiol 20(2):205–217. https://doi.org/10.3348/kjr.2018.0479
Prado CM, Birdsell LA, Baracos VE (2009) The emerging role of computerized tomography in assessing cancer cachexia. Current opinion in supportive and palliative care 3(4):269–275. https://doi.org/10.1097/SPC.0b013e328331124a
Nishimura JM, Ansari AZ, D'Souza DM, Moffatt-Bruce SD, Merritt RE, Kneuertz PJ (2019) Computed tomography-assessed skeletal muscle mass as a predictor of outcomes in lung cancer surgery. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2019.04.090
Elsawy M, Sorror ML (2016) Up-to-date tools for risk assessment before allogeneic hematopoietic cell transplantation. Bone Marrow Transplant 51(10):1283–1300. https://doi.org/10.1038/bmt.2016.141
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS et al (2014) Sarcopenia in Asia: Consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc 15(2):95–101. https://doi.org/10.1016/j.jamda.2013.11.025.
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. Journal of the American Medical Directors Association 12(4):249–56. https://doi.org/10.1016/j.jamda.2011.01.003.
Gerrie AS, Plantinga P, Nishikawa K, Hung S, Kadgien J, Chernoff B et al (2016) Implementation of a physician-prescribed exercise program as standard of care in allogeneic stem cell transplant (SCT) patients (pts) in British Columbia: a pilot study. Blood 128:22
Gevedon AJ, Monfreda JK (2014) Physical therapy during the hemopoietic stem cell transplant process to improve quality of life. Biol Blood Marrow Transplan 1:S198
van der Meij BS, De Groot LM, Deutz NEP, Engelen M (2019) Effects of acute oral feeding on protein metabolism and muscle protein synthesis in individuals with cancer. Nutrition (Burbank, Los Angeles County, Calif) 110531:67–68. https://doi.org/10.1016/j.nut.2019.06.012
Takekiyo T, Dozono K, Mitsuishi T, Murayama Y, Maeda A, Nakano N, Kubota A, Tokunaga M, Takeuchi S, Takatsuka Y, Utsunomiya A (2015) Effect of exercise therapy on muscle mass and physical functioning in patients undergoing allogeneic hematopoietic stem cell transplantation. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer 23(4):985–992
Author information
Authors and Affiliations
Contributions
Idea and protocol writing were performed by Birong Dong and Shuli Jia. Literature search, data collection, and analysis were performed by Shuli Jia, Runjuan Qiao, Yuting Xiao, and Dan Qin. Methodology: Birong Dong, Shuli Jia, Wanyu Zhao, and Yunli Zhao. The first draft of the manuscript was written by Shuli Jia, and all authors commented on previous versions of the manuscript. The revised draft of the manuscript was written by Shuli Jia and Xiaolei Liu. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was not necessary as no human subjects were involved in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1
Appendix 1
Medline (via ovid) search strategy
-
1.
exp. Sarcopenia/ or exp. Muscular Atrophy/
-
2.
(“Muscular Atrophy” or Sarcopenia or Sarcopenias or Sarcopenic or presarcopenia or Sarcopenia or “low muscle mass” or “ low muscle function” or “ muscle weakness” or “muscle loss”).af.
-
3.
1 or 2
-
4.
exp. Hematologic Neoplasms/
-
5.
(Hematolog* or hamatolog*).mp.
-
6.
(carcin* or cancer* or neoplas* or tumour* or tumor* or malig*).mp.
-
7.
3 and 4
-
8.
(leukenia or lymphoma or “myelodysplastic syndromes” or MDS or myeloma).af.
-
9.
4 or 6 or 7
-
10.
exp. Hematopoietic Stem Cell Transplantation/ or exp. Bone Marrow Transplantation/ or exp. Peripheral Blood Stem Cell Transplantation/
-
11.
(“Bone Marrow Cell” or “Bone Marrow” or “Peripheral Stem Cell” or “ Peripheral Blood Stem Cell” or “hematopoietic Stem Cell” or “hamatopoietic Stem Cell” or stem cell*).af.
-
12.
Transpl*.af
-
13.
10 and 11
-
14.
(HCT or HSCT).af.
-
15.
9 or 12 or 13
-
16.
3 and 8 and 14
Rights and permissions
About this article
Cite this article
Jia, S., Qiao, R., Xiao, Y. et al. Prognostic value of sarcopenia in survivors of hematological malignances undergoing a hematopoietic stem cell transplantation: a systematic review and meta-analysis. Support Care Cancer 28, 3533–3542 (2020). https://doi.org/10.1007/s00520-020-05359-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05359-3