Abstract
Background
Considerable progress has been made in our understanding of the biological basis for cancer therapy-induced mucosal barrier injury (mucositis). The last formal review of the subject by MASCC/ISOO was published in 2007; consequently, an update is timely.
Methods
Panel members reviewed the biomedical literature on mucositis pathobiology published between January 2005 and December 2011.
Results
Recent research has provided data on the contribution of tissue structure changes, inflammation and microbiome changes to the development of mucositis. Additional research has focused on targeted therapy-induced toxicity, toxicity clustering and the investigation of genetic polymorphisms in toxicity prediction. This review paper summarizes the recent evidence on these aspects of mucositis pathobiology.
Conclusion
The ultimate goal of mucositis researchers is to identify the most appropriate targets for therapeutic interventions and to be able to predict toxicity risk and personalize interventions to genetically suitable patients. Continuing research efforts are needed to further our understanding of mucositis pathobiology and the pharmacogenomics of toxicity.
Similar content being viewed by others
Introduction
Mucosal damage affecting the gastrointestinal tract is a common toxicity of anti-neoplastic drug or radiation therapy. Injury to the mouth [oral mucositis (OM)] is among one of the best studied side effects of cancer therapy. Ulcerations associated with OM result in significant pain which affects patients’ ability to eat, necessitates analgesic use, adversely affects quality of life and increases the cost whilst reducing tolerability of cancer treatment. Mucositis can thus have a profound negative effect on nutritional status, oral intake of food and medications and maintenance of oral health in patients. Clinically, the manifestations of OM form a continuum, where in its mild form it presents as erythematous atrophic lesions and in its severe form as ulcerative lesions which penetrate the submucosa. Loss of mucosal layer integrity in OM, especially in patients undergoing myeloablative therapy, represents a clinically significant risk factor for bacteraemia, fungaemia and sepsis [1, 2].
Mucositis is not limited to the mouth, and cytotoxic treatment can broadly impact various mucosal tissues. Over the last decade, the impact of injury to other areas of the gastrointestinal (GI) tract including the esophagus, stomach and small and large intestine has become increasingly recognized and better characterised. Symptoms include pain, ulceration, nausea and vomiting, diarrhoea and rectal bleeding [3, 4] and depend on the area affected. Systemic effects of oral and GI mucositis include fatigue, malnutrition, sepsis and occasionally death [4–6].
Mucositis of either the oral cavity or of the GI tract is associated with increased use of healthcare resources and not infrequently is a reason for hospital admission. As a result, the incremental cost of mucositis is significant and adds a measurable burden to resources required for the care of patients with cancer.
Our current understanding of this condition is largely based on OM animal models which described the multifactorial nature of the condition and implicates a cascade of events in multiple tissue regions [7–9]. These observations gave rise to the five-phase model of OM developed by Sonis, which describes the sequence of genetic and histopathological events following cytotoxic treatment. Subsequent studies confirmed the complexity of mucositis pathogenesis and implicated microvascular injury [10], proinflammatory cytokines [11–14], host–microbiome interactions [15–17] and extracellular matrix alterations [18, 19] .
This paper describes emerging areas in oral and GI mucositis research since the last review on pathobiology from the Mucositis Study Group of MASCC/ISOO [20] and provides an update on the pathobiology underlying mucosal toxicity of cytotoxic and targeted anti-cancer therapies.
Methodology
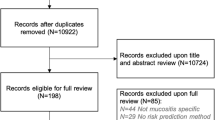
A literature search for relevant papers indexed in Medline was conducted using OVID/MEDLINE. The search included papers from January 2005 to December 2011. The key search terms included were: stomatitis, mucositis, mucous membrane, neoplasms, antineoplastic agents, hematopoietic stem cell transplantation, anticancer, tumour, chemotherapy, radiotherapy, oncology, metastases, leukemia, lymphoma and radiation therapy. A total of 282 papers were originally identified. Papers were evaluated for relevance qualitatively throughout the review process. One hundred twenty-two papers were excluded after evaluating the title/abstract and 162 retrieved for detailed analysis. A further 20 papers were excluded prior to review, 142 papers were sent out for review and 106 included in the final manuscript. Structured inclusion criteria for papers were not suitable for this review, and papers were selected based on relevance. All papers were reviewed by two independent reviewers and responses recorded on a specially designed review form. Upon completion of reviews, the emerging areas in mucositis pathobiology research were identified. The review findings were sorted under two sections: those which provide an update on the biological causes underpinning mucositis pathology in general, and those which provide an update on mucositis pathobiology due to particular cancer therapies.
Results
Overview of the emerging mediators of toxicity
Individual patients often demonstrate different degrees of mucosal injury across anatomic sites within the gastrointestinal tract. This observation has led to a burst in research activity which is focused on identifying and exploring the biological controllers and mediators unique to specific mucosal tissues.
Tissue structure
Cell kinetics
Cytotoxic agents induce cell death in both tumour and healthy tissues via apoptosis [21]. Rapidly proliferating cells are more susceptible meaning the oral and GI mucosa is particularly vulnerable [22]. There are differences in susceptibility along the alimentary tract with early damage occurring in the small intestine and to a lesser extent in the colon (day 2–3), and later damage in the oral cavity (day 7–10). There is an increase in the number of cells undergoing apoptosis throughout the alimentary tract corresponding with a decrease in the number of cells that are mitotically active [23–27]. Early studies investigating the effect of epidermal growth factor (EGF) on mucositis have shown that EGF stimulated epithelial cell proliferation and significantly increased the severity of mucositis indicating the importance of renewal rate of the epithelium in determining susceptibility of the mucosa to injury. It is well established clinically that oral mucositis encompasses apoptosis in the basal layer of the buccal and gut mucosa [23, 27, 28]. More recently, it has been shown that radiotherapy-induced glossitis is associated with endothelial cell apoptosis in local tissues, and this was correlated with the Oral Mucositis Index [29]. In the small intestine, studies have demonstrated that chemotherapy causes crypt hypoplasia, followed by rebound crypt hyperplasia and finally restoration of normal tissue [23, 27, 30]. Some agents with anti-apoptotic properties have shown ability to alleviate mucositis severity in animal models, including AMP-18 [31] and minocycline [32]. These studies yet again highlight the importance of intricate regulation of cell kinetics in maintaining mucosal layer integrity and demonstrate its contribution to mucosal injury following cytotoxic drugs.
The extracellular matrix (ECM) plays a significant role in signalling between tissues and is a complex structural network of fibrous proteins, proteoglycans and glycoproteins [33]. It is vital for maintenance of normal tissue morphology and wound healing. Until recently, cancer therapy-induced changes in ECM proteins and their subsequent effect on cell kinetics had not been well characterised. In a recent study by Al-Dasooqi and colleagues, ECM protein expression and its effects on cell kinetics were investigated. The findings indicated substantial augmentation in cell kinetics, particularly cell cytostasis and substantial apoptosis was noted, in response to irinotecan. Furthermore, this was accompanied by a decrease in fibronectin early on following treatment and an increase in collagen deposits during the period of maximal damage [18]. The changes in ECM expression were attributed to deregulated expression of matrix metalloproteinases following chemotherapy [18, 19]. These studies suggest that treatment aimed at maintaining extracellular tissue compartments may be an effective intervention for chemotherapy-induced intestinal injury.
In addition to its impact on kinetics, earlier studies by Afshar et al. demonstrated the importance of the ECM in affecting epithelial differentiation during healing [36, 36]. It seems likely that among its functions, the ECM mediates mesenchymal–epithelial communication.
Epithelial junctional integrity
Tight junctions play a vital role in maintaining epithelial layer integrity and function. These are intercellular occluding junctions which act as a selectively permeable barrier to fluid flow between cells. A variety of physiological and pharmacological stimuli can modulate the barrier properties of tight junctions leading to intestinal hyperpermeability. Tight junction functions have been shown to be altered in many acute and chronic diseases of the gut. Recent experimental studies have demonstrated a reduced expression of the tight junction proteins claudin-1, occludin and zonula occludin during the acute phase of mucositis [36, 37]. A number of studies have demonstrated a change in tight junction permeability due to TNF-α and IL-1β [38–41]. Moreover, these changes in tight junctions were prevented by MEK-1, MEK-2, JNK and NFкB inhibitors [36]. It is unknown to what extent tight junction alterations contribute to the clinical manifestations of mucositis, however, a novel peptide derived from the 18-kDA antrum mucosal protein (AMP-18) has been shown to attenuate oral mucositis, possibly as a result of its tight junction-protective properties in an animal model of acute radiation injury [31]. Intestinal permeability testing has also been suggested as an indicator of toxicity [42].
Inflammation
According to the five-phase model for mucositis development, it has been suggested that the transcription factor NFкB acts as a ‘gatekeeper’ for various pathways (one of which are the pro-inflammatory cytokines). Logan and colleagues (2008) demonstrated that peaks in NFкB expression preceded peaks in pro-inflammatory cytokines in oral and intestinal tissue following chemotherapy [43]. Once pro-inflammatory cytokines are upregulated, they have been suggested to provide positive feedback by activating NFкB and amplifying injurious pathways [44, 45]. NFкB has also been shown to upregulate cyclooxygenase-2 (COX-2), an inducible enzyme involved in inflammation through its role in prostaglandin production. COX-2 expression was shown to dramatically increase, particularly in submucosal fibroblasts and endothelial cells of the oral mucosa, 10 and 16 days after targeted radiation [46]. Furthermore, changes in COX-2 expression paralleled with the development of ulcerative mucositis, suggesting an amplification role for this enzyme [46]. These results have also been demonstrated clinically where a statistically significant increase in NFкB and COX-2 was noted in the oral mucosa of patients undergoing chemotherapy [47]. However, the selective COX-2 inhibitor celecoxib was found ineffective for the treatment of oral mucositis in a preclinical model [48].
In recent years, it has been shown that pro-inflammatory cytokines play a key role in both oral and GI toxicities. Gene expression and tissue levels of TNF-α and IL-1β were shown to closely correlate with oral and gut mucosa injury following radiation [8, 12, 49]. The pro-inflammatory cytokines TNF, IL-1β and IL-6 were also associated with the development of chemotherapy-induced GI mucositis [11, 50, 51]. Furthermore, elevated levels of pro-inflammatory cytokines, in particular TNF, IL-1β and IL-6, have been identified as being excellent markers of the inflammatory response induced by chemotherapy [51]. Anti-inflammatory agents directed at pro-inflammatory cytokine inhibition have shown promise for reducing mucositis severity in animal models; however, results are not uniformly positive [48, 52, 53].
Few studies have looked specifically at anti-inflammatory cytokines and toxicities, but these have demonstrated a shift in the balance between pro and anti-inflammatory cytokines with a net shift towards pro-inflammatory cytokines [54]. IL-10 is one of the more researched anti-inflammatory cytokines in mucositis. DeKoning and colleagues demonstrated that IL-10-deficient mice experience an increased weight loss and more severe intestinal damage following methotrexate treatment in comparison to wild-type controls [55]. Furthermore, cytokines directed at inhibiting pro-inflammatory cytokines may be useful as interventions for mucositis [56]. For example, IL-11, a cytokine secreted by bone marrow stromal cells, has demonstrated ability to reduce the severity of GI mucositis in an animal model, although this was not seen clinically [57, 58]. The putative mechanism of action of IL-11 is partly through its ability to inhibit cytokine release and downregulate inflammatory mediators such as TNF. Another anti-inflammatory agent known as anti-inflammatory amino acid decapeptide (RDP58) also inhibits the production of certain cytokines and has demonstrated effectiveness in ameliorating symptoms (primarily diarrhoea) and intestinal inflammation in mice following chemotherapy [59].
Microbiome changes
Observations noting shifts in the oral and GI flora of myelosuppressed patients were reported almost 50 years ago [60]. Their impact on the oral mucosa was reported thereafter [61]. Additional studies have continued to investigate shifts in the ecological balance of the oral and gut flora following anti-cancer treatment [16, 17, 62–66].
Oral flora
Changes in shifts in the oral bacterial flora associated with neutropenia and mucosal surface changes are well documented [67]. Furthermore, OM has been identified as an independent risk factor for the development of infections [68, 69]. A recent study by Napenas and colleagues (2010) studied the profile of the oral bacterial flora following anthracycline therapy in an outpatient cancer population. They found that over 60 % of bacterial flora identified on patients’ buccal mucosa was exclusively seen post-chemotherapy suggesting an alteration in the nature of oral flora [65]. Shifts in oral bacterial flora in cancer patients have also been attributed to antibiotic use [70], neutropenia [71] and xerostomia [70]. Bacterial substitution (of mainly coagulase-negative staphylococci for streptococci) has also been reported on the oral mucosa after hematopoietic cell transplantation, and this was clearly associated with OM [70]. Other reports note that quantitative mucosal changes in oral bacteria follow, rather than precede, the development of OM. This suggests that components of the oral flora colonize ulcerative lesions and may aggravate their severity, but are unlikely to be their primary etiology [72]. The failure of most antimicrobial interventions tested for oral mucositis also supports the notion that the microbial flora are not a primary causative factor for oral mucositis [73].
Gut microbiome
The gut microbiota and its influence on GI mucositis is becoming an increasingly recognised field of research [16, 74]. It was previously believed that the gut microbiota plays little role in the pathobiology of mucositis, with bacterial translocation being a secondary outcome of mucosal layer degradation following inflammation and apoptosis. However, recent studies have shown a shift from commensal bacteria, in particular Bifidobacterium spp., towards Salmonella spp. and Escherichia coli following chemotherapy treatment [15]. Stringer and colleagues (2009) demonstrated that decreases in commensal bacteria, represented by Bifidobacterium spp., inversely followed the pattern of diarrhoea induced by chemotherapy. These results strongly suggest a role for gut microbiome changes in diarrhoea induction. It is not yet clear how commensal bacteria influence the different stages of mucositis development; however, it has been suggested that these are capable of influencing inflammatory processes, intestinal permeability, mucus layer composition, epithelial repair mechanisms and regulation of immune effector molecules including Toll-like receptors [66]. A possible explanation for these observations requiring additional investigation is that clinical manifestations of diarrhoea are not exclusively the result of mucositis and that, as in the non-oncology population, disruptions in the normal microbial flora may result in disturbed bowel function. Data supporting such a hypothesis have been derived from intervention studies using probiotic factors, which have proven effective in reducing cancer therapy-induced diarrhoea in the preclinical and clinical settings [75, 76]. An additional factor affecting the role of the microbiota may be the effect of the tumour on the immune response. Gibson and colleagues demonstrated that tumour-bearing rats experienced greater toxicity to irinotecan than non-tumour-bearing rats [27].
An association between GI mucositis and systemic infection has been well established and confirmed by recent studies [77]. Clinical data consistently demonstrate that chemotherapy cycles complicated by mucositis are associated with significantly higher risk of infections and use of antibiotics [1]. Furthermore, the most frequently occurring infection in cycles complicated by mucositis involves gram-positive cocci, an infection which accounts for three of every four episodes of bacteraemia in patients treated for haematological malignancies [78]. The ulcerative phase of mucositis has been suggested to be a major contributor, allowing the translocation of residential microorganisms and their products from the alimentary tract into the bloodstream. This is reported to most probably occur at the periodontium, other soft tissues of the oral cavity, oesophagus, ileum, cecum and rectum [77].
Targeted anti-cancer agents and mucosal injury
The early promise that targeted therapies would increase cure rates while minimising toxicity has not been completely fulfilled [79]. Toxicities include those due to the presence of target receptors on healthy tissues, the promiscuous cross-reactivity of tyrosine kinase inhibitors and the adverse effects of immunostimulation. Both stomatitis and diarrhoea have been reported. Among patients receiving certain mTOR inhibitors to treat various solid tumours, the rate of stomatitis was 66 % [80]. These ulcers resembled those of aphthous stomatitis and were distinct from those seen in conventional mucositis. Further, unlike conventional mucositis, oral lesions secondary to targeted agents are often accompanied by a skin rash. These observations suggest that the pathogenic mechanisms of targeted therapy-induced toxicity are not necessarily the same as for other cancer treatments, and there remains a vast gap in our knowledge regarding the biological mechanisms responsible [81–83]. The term “stomatitis” has been used in several recent publications for oral lesions secondary to targeted agents to distinguish them from mucositis secondary to conventional chemotherapy and radiation therapy.
Targeted cancer therapy is often administered concurrently with chemotherapy or radiation, which appears to increase the frequency and severity of toxicities. For example, lapatinib, a reversible dual HER1/HER2 tyrosine kinase inhibitor, has been shown to cause diarrhoea in 42 % of patients when administered as a single agent [84]. In a phase III trial, where lapatinib was administered in combination with capecitabine, there was a significant increase in diarrhoea incidence, with 60 % of patients experiencing diarrhoea in the combination group [85]. The use of trastuzumab in combination treatments has also demonstrated an increase in incidence as well as severity of toxicities experienced. Al-Dasooqi and colleagues demonstrated single-agent trastuzumab induces gastrointestinal toxicities following 12 % of administrations. These include diarrhoea, abdominal pain and vomiting [86]. Moreover, phase II studies investigating the efficacy and tolerability of trastuzumab in combination with paclitaxel have shown diarrhoea to be the most frequent toxicity manifesting in 30 % of patients [87]. Toxicity profiling for newer combination regimens where trastuzumab is given with carboplatin or capecitabine has shown significant induction of mucositis, diarrhoea and vomiting at grade 3–4 intensity [88, 89].
The biological mechanisms underpinning these toxicities are largely unknown. Animal models are currently being utilized and developed. A recently developed, clinically relevant rat model of receptor tyrosine kinase inhibitor-induced diarrhoea has already identified differences in the mechanisms of damage following targeted drugs and conventional chemotherapy agents [90]. This model is currently being utilised to determine the exact pathogenesis of lapatinib-induced diarrhoea and to evaluate potential protective strategies.
Links to other toxicities
Until recently, the bulk of investigations into mucositis mechanisms have been in relation to the oral cavity and digestive tract, with little or no research on other mucosal surfaces which are generally less susceptible (the exception being bladder toxicity and haemorrhagic cystitis from cyclophosphamide). The respiratory and genitourinary tracts are mucosal surfaces which are affected by cytotoxics and may share a common injury pathobiology with the alimentary tract [91]. In the clinic, mucosal-related toxicities often occur concurrently following cytotoxic treatment, and this has prompted the need for investigating the common mechanisms of different regimen-related mucosal toxicities.
One of the first studies to recognise that toxicities arise in clusters rather than in isolation was carried out by Aprile and colleagues (2008). In a cohort of colorectal cancer patients, findings indicated the occurrence of localised (ulceration, abdominal pain, diarrhoea and malabsorption) as well as systemic (fatigue, nausea, infection and depression) toxicities in clusters. The recognition of concurrent occurrence of tissue-based and systemic toxicities has caused a shift in the potential applications of toxicity models to investigate regimen-related toxicity rather than tissue-specific toxicity [5]. Understanding toxicity clusters in response to different chemotherapy and/or radiotherapy regimens in different cancer types will aid in advancing mechanistic research and perhaps will also push forward the development of a systemic biomarker of toxicity.
Advances in mucosal injury risk prediction
While the frequency and severity of mucositis vary depending on the type and dose of cancer therapy, the clinical observation of variable mucositis rates among patients with similar malignancies and treatment regimens has resulted in a number of attempts to identify specific risk factors. The narrow range between therapeutic and toxic doses of antineoplastic agents makes identification of risk factors especially significant [92]. Risk factors for mucositis may be placed into two treatment categories: those associated with treatment and those that are patient-related [93]. Treatment-associated variables include drug and dosing schedule, route of administration, formulation, use of concomitant therapies and agents, radiation schedule, port and radiation source [92]. Reported patient-related risk factors include age, bodyweight, body mass, gender, renal and hepatic function, local oral factors and genetics [92]. Also, patients’ ability to metabolise and eliminate drugs may impact their risk for toxicity, and a pharmacogenetically based approach to risk assessment can be used to identify patients at risk for prolonged or severe toxicity. For example, deficiencies in dihydropyrimidine dehydrogenase, the enzyme responsible for catabolizing 5-FU in liver, are associated with increased toxicity [94]. Importantly, however, the percentage of patients affected by mutations impacting chemotherapy drug metabolism is small and far less than the population which goes on to develop toxicities.
An alternative approach is based on the observation that the presence of certain single nucleotide polymorphisms (SNPs) is associated with toxicity risk. SNP-based toxicity risk has been studied using both candidate gene and genome-wide association approaches [95, 96]. To date, the use of SNPs as mucositis risk predictors has been evaluated in a relatively small number of studies [95, 97–101]. Most of these studies are not confirmed and are predominantly associated with metabolic pathways of a small number of drugs. Recently, an entirely different analytical method has been proposed in which Bayesian networks learned from SNP array outputs were predictive of oral mucositis risk in patients undergoing hematopoietic stem cell transplantation [91]. This technique was used by Alterovitz et al. (2011) to identify gene clusters which differentiated responders from non-responders in a mucositis clinical trial [102]. Ongoing research is required in this area and should be based on our current knowledge in the pathobiology of mucositis. The ultimate goal of this research is to be able to personalise cancer treatment and avoid severe and potentially life-threatening drug toxicity for patients.
Biomarkers of mucosal injury
The conceptual application of biomarkers to assess the severity and course of cancer therapy-related injury is not new. A range of biomarkers have been investigated including citrulline, calprotectin and the pro-inflammatory cytokines [51, 103, 104]. For a biomarker to have clinical utility, it should have some actionable clinical value. Alternatively, as a research tool, robust biomarkers would serve as real-time surrogates of mucosal injury. In this respect, there has been some success.
An emerging class of biomarkers for mucositis is the pro-inflammatory cytokines and matrix metalloproteinases (MMPs). These have augmented expression profiles in the alimentary tract in animal models of mucositis [19, 50]. Preliminary findings from a pilot human study suggest that TNF, IL1β, MMP-3 and MMP-9 are potential biomarkers of gastrointestinal toxicity induced by 5-fluorouracil, capecitabine or irinotecan. Apoptotic and inflammatory markers detectable in cytologic smears have also been suggested as potential biomarkers of OM [105]. Prospective studies are now required to assess the feasibility of biomarkers for mucositis in particular and regimen-related toxicity in general.
Conclusions
The ultimate goal of mucositis researchers is to be able to predict toxicity risk and personalise toxicity interventions to genetically suitable patients. Continuing research efforts are needed to further our understanding of mucositis pathobiology and the pharmacogenomics of toxicity. This can be achieved by performing high-quality pre-clinical research in validated and clinically relevant animal models and investigating the potential of these findings for toxicity prediction and attenuation in the clinic.
References
Elting L et al (2003) The burdens of cancer therapy: clinical and economic outcomes of chemotherapy-induced mucositis. Cancer 98:1531–1539
Sonis S et al (2004) Perspectives on cancer therapy-induced mucosal injury: pathogenesis, measurement, epidemiology, and consequences for patients. Cancer 100:1995–2025
Capp A et al (2009) Is there more than one proctitis syndrome? A revisitation using data from the TROG 96.01 trial. Radiother Oncol 90:400–407
Keefe D et al (2007) Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer 109:820–831
Aprile G et al (2008) Application of distance matrices to define associations between acute toxicities in colorectal cancer patients receiving chemotherapy. Cancer 112:284–292
Murphy B (2007) Clinical and economic consequences of mucositis induced by chemotherapy and/or radiation therapy. J Support Oncol 5:13–21
Sonis S (2004) The pathobiology of mucositis. Nat Rev Cancer 4:277–284
Sonis S et al (2002) The gene expression sequence of radiated mucosa in an animal mucositis model. Cell Prolif 35:s92–s102
Sonis S et al (1990) An animal model for mucositis induced by cancer chemotherapy. Oral Surg, Oral Med, Oral Pathol 69:437–443
Paris F et al (2001) Endothelial apoptosis as the primary lesion initiating intestinal radiation damage in mice. Science 293:293–297
Logan R et al (2009) Is the pathobiology of chemotherapy-induced alimentary tract mucositis influenced by the type of mucotoxic drug administered? Cancer Chemother Pharmacol 63:239–251
Sonis S et al (2000) Defining mechanisms of action of interleukin-11 on the progression of radiation-induced oral mucositis in hamsters. Oral Oncol 36:373–381
Yeoh A et al (2005) Nuclear factor κB (NFκB) and cyclooxygenase-2 (COX-2) expression in the irradiated colorectum is associated with subsequent histopathological changes. Int J Radiat Oncol Biol Phys 63:1295–1303
Manzano M et al (2007) Intestinal toxicity induced by 5-fluorouracil in pigs: a new preclinical model. Chemotherapy 53:344–355
Stringer A et al (2009) Irinotecan-induced mucositis manifesting as diarrhoea corresponds with an amended intestinal flora and mucin profile. Int J Exp Pathol 90:489–499
Stringer A et al (2009) Chemotherapy-induced changes to microflora: evidence and implications of change. Curr Drug Metab 10:79–83
Stringer A et al (2007) Chemotherapy-induced diarrhea is associated with changes in the luminal environment in the DA rat. Exp Biol Med 232:96–106
Al-Dasooqi N et al (2011) Irinotecan-induced alterations in intestinal cell kinetics and extracellular matrix component expression in the dark agouti rat. Int J Exp Pathol 92:357–365
Al-Dasooqi N et al (2010) Matrix metalloproteinases are possible mediators for the development of alimentary tract mucositis in the DA rat. Exp Biol Med 235:1244–1256
Anthony L et al (2007) New thoughts on the pathobiology of regimen-related mucosal injury. Support Care Cancer 14:516–518
Hannum Y (1997) Apoptosis and the dilemma of cancer chemotherapy. Blood 89:1845–1853
Kerr J, Winterford C, Harmon B (1994) Apoptosis: its significant in cancer and cancer therapy. Cancer 73:2013–2026
Gibson R et al (2005) Relationship between dose of methotrexate, apoptosis, p53/p21 expression and intestinal crypt proliferation in the rat. Clin Exp Med 4:188–195
Bowen J et al (2005) Cytotoxic chemotherapy up-regulates pro-apoptotic Bax and Bak in the small intestine of rats and humans. Pathology 37:56–62
Keefe D (2000) Chemotherapy for cancer causes apoptosis that precedes hypoplasia in crypts of the small intestine in humans. Gut 47:632–637
Sonis S et al (1992) Effect of epidermal gorwth factor on ulcerative mucositis in hamsters that receive chemotherapy. Oral Surg, Oral Med, Oral Pathol 74:749–755
Gibson R et al (2007) Establishment of a single-dose irinotecan model of gastrointestinal mucositis. Chemotherapy 53:360–369
Gibson R et al (2006) Apoptosis occurs early in the basal layer of the oral mucosa following cancer chemotherapy. Asia Pac J Clin Oncol 2:39–49
Li C et al (2011) The correlation between the severity of radiotherapy-induced glossitis and endothelial cell injury in local tissues in a rat model. Med Oral Pathol Oral Cir Bucal 16:e711–e715
Carneiro-Filho B et al (2004) Intestinal barrier function and secretion in methotrexate-induced rat intestinal mucositis. Dig Dis Sci 49:65–72
Chen P et al (2011) Role of AMP-18 in oral mucositis. Oral Oncol 47:831–839
Huang T et al (2009) Minocycline attenuates 5-fluorouracil-induced small intestinal mucositis in mouse model. Biochem Biophys Res Commun 389:634–639
Meredith J, Fazeli B, Schwartz M (1993) The extracellular matrix as a cell survival factor. Mol Biol Cell 4:953–961
Afshar S, Phelan K, O'Donnell C, Bragdon C, Castro D, Sonis S (2002) A new in vivo model for the study of mucosal disease. International Association for Dental Research Meeting Abstract 16220
Phelan S, Afshar S, O'Donnell C, Bragdon C, Castro D, Shklar G, Sonis S (2002) A mucosal graft model to evaluate radiation induced injury. International Association for Dental Research Meeting Abstract 0221
Beutheu Youmba S et al (2012) Methotrexate modulates tight junctions through NFkB, MEK, and JNK pathways. J Pediatric Gastroenterol Nutr 54:463–470
Hamada K et al (2010) Zonula Occluden-1 alterations and enhances intestinal permeability in methotrexate-treated rats. Cancer Chemother Pharmacol 66:1031–1038
Al-Sadi R et al (2010) IL-1beta-induced increase in intestinal epithelial tight junction permeability is mediated by MEKK-1 activation of canonical NF-kappaB pathway. Am J Pathol 177:2310–2322
Al-Sadi R et al (2008) Mechanism of IL-1beta-induced increase in intestinal epithelial tight junction permeability. J Immunol 180:5653–5661
Ma T et al (2004) TNF-alpha-induced increase in intestinal epithelial tight junction permeability requires NF-kappa B activation. Am J Physiol Gastrointest Liver Physiol 286:G367–G376
Han X, Fink M, Delude R (2003) Proinflammatory cytokines cause NO*-dependent and -independent changes in expression and localization of tight junction proteins in intestinal epithelial cells. Shock 19:229–237
Melichar B et al (2005) Intestinal permeability in the assessment of intestinal toxicity of cytotoxic agents. Chemotherapy 51:336–338
Logan R et al (2008) Characterisation of mucosal changes in the alimentary tract following administration of irinotecan: implications for the pathobiology of mucositis. Cancer Chemother Pharmacol 62:33–41
Sonis S (2002) The biologic role for nuclear factor-kappaB in disease and its potential involvement in mucosal injury associated with anti-neoplastic therapy. Crit Rev Oral BiolMed 13:380–389
Sonis S (2004) A biological approach to mucositis. J Support Oncol 2:21–32
Sonis S et al (2004) The relationship between mucosal cyclooxygenase-2 (COX-2) expression and experimental radiation-induced mucositis. Oral Oncol 40:170–176
Logan R et al (2007) Nuclear factor-kB (NFkB) and cyclooxygenase-2 expression in the oral mucosa following cancer chemotherapy. Oral Oncol 43:395–401
Haagen J et al (2009) Effect of selective inhibitors of inflammation on oral mucositis: preclinical studies. Radiother Oncol 92:472–476
Ong Z et al (2010) Pro-inflammatory cytokines play a key role in the development of radiotherapy-induced gastrointestinal mucositis. Radiat Oncol 16:22
Logan R et al (2007) The role of pro-inflammatory cytokines in cancer treatment-induced alimentary tract mucositis: pathobiology, animal models and cytotoxic drugs. Cancer Treat Rev 33:448–460
Logan R et al (2008) Serum levels of NFkappaB and pro-inflammatory cytokines following administration of mucotoxic drugs. Cancer Biol Ther 7:1139–1145
Lima V et al (2005) Effects of tumour necrosis factor-alpha inhibitors pentoxifylline and thalidomide in short-term experimental oral mucositis in hamsters. Eur J Oral Sci 113:210–217
Melo M et al (2008) Role of cytokines (TNF-alpha, IL-1beta and KC) in the pathogenesis of CPT-11-induced intestinal mucositis in mice: effect of pentoxifylline and thalidomide. Cancer Chemother Pharmacol 61:775–784
Fiochhi C (1998) Inflammatory bowel disease: etiology and pathogenesis. Gastroenterology 115:182–205
de Koning B et al (2006) Contributions of mucosal immune cells to methotrexate-induced mucositis. Int Immunol 18:941–949
Bultzingslowen I et al (2006) Growth factors and cytokines in the prevention and treatment of oral and gastrointestinal mucositis. Support Care Cancer 14:519–527
Gibson R et al (2002) Effect of interleukin-11 on ameliorating intestinal damage after methotrexate treatment of breast cancer in rats. Dig Dis Sci 47:2751–2757
Antin J et al (2002) A phase I/II double-blind, placebo-controlled study of recombinant human interleukin-11 for mucositis and acute GVHD prevention in allogeneic stem cell transplantation. Bone Marrow Transplant 29:373–377
Zhao J et al (2004) Oral RDP58 allows CPT-11 dose intensification for enhanced tumor response by decreasing gastrointestinal toxicity. Clin Cancer Res 10:2851–2859
Frei E et al (1965) The nature and control of infections in patients with acute leukemia. Cancer Res 25:1511–1515
Dreizen S, Bodey G, Brown L (1974) Opportunistic gram-negative bacillary infections in leukemia. Oral manifestations during myelosuppression. Post Med 55:133–139
Stringer A et al (2008) Faecal microflora and β-glucuronidase expression are altered in an irinotecan-induced diarrhoea model in rats. Cancer Biol Ther 7:1919–1925
Stringer A et al (2009) Gastrointestinal microflora and mucins play a role in the development of 5-fluorouracil-induced gastrointestinal mucositis in rats. Exp Biol Med 234:430–441
Shao Z et al (2011) Effects of intensity-modulated radiotherapy on human oral microflora. J Radiat Res 52:834–839
Napenas J et al (2010) Molecular methodology to assess the impact of cancer chemotherapy on the oral bacterial flora: a pilot study. Oral Surg, Oral Med, Oral Pathol, Oral Radiol Endodentics 109:554–560
van Vliet M et al. (2010) The role of intestinal microbiota in the development and severity of chemotherapy-induced mucositis. PLoS Pathog 6(5): e1000879
Martin M, van Saene H (1992) The role of oral microorganisms in cancer therapy. Curr Opin Dent 2:81–84
Bochud P et al (1994) Bacteremia due to viridans streptococcus in neutropenic patients with cancer: clinical spectrum and risk factors. Clin Infect Dis 18:25–31
Ruescher T et al (1998) The impact of mucositis on alpha-hemolytic streptococcal infection in patients undergoing autologous bone marrow transplantation for hematologic malignancies. Cancer 82:2275–2281
Soga Y et al (2011) Bacterial substitution of coagulase-negative staphylococci for streptococci on the oral mucosa after hematopoietic cell transplantation. Support Care Cancer 19:995–1000
van der Velden W, Donnelly J, Blijlevens N (2012) Lymphocyte subsets, granulocyte-colony-stimulating factor responsiveness and post-stem cell transplantation infections: mucositis is the underestimated confounder? Cytotherapy 14:381–383
Sonis S (2009) Mucositis: the impact, biology and therapeutic opportunities of oral mucositis. Oral Oncol 45:1015–1020
Barasch A et al (2006) Antimicrobials, mucosal coating agents, anesthetics, analgesics, and nutritional supplements for alimentary tract mucositis. Support Care Cancer 14:528–532
Blijlevens N, Donnelly J, DePauw B (2000) Mucosal barrier injury: biology, pathology, clinical counterparts and consequences of intensive treatment for haematological malignancy: an overview. Bone Marrow Transplant 25:1269–1278
Prisciandaro L et al (2011) Probiotic factors partially improve parameters of 5-fluorouracil-induced intestinal mucositis in rats. Cancer Biol Ther 11:671–677
Gibson R et al. (2013) Systematic review of agents for the management of gastrointestinal mucositis in cancer patients. Supportive Care Cancer 21(1):313-26
Blijlevens N, Donnelly J (2011) Mucosal barrier injury and infections. In: Safdar A (ed) Principles and practice of cancer infectious diseases, current clinical oncology. Springer Science, New York
Wisplinghoff H et al (2003) Current trends in the epidemiology of nosocomial bloodstream infections in patients with hematological malignancies and solid neoplasms in hospitals in the United States. Clin Infect Dis 36:1103–1110
Keefe D, Bateman E (2011) Tumor control versus adverse events with targeted anticancer therapies. Nat Rev Clin Oncol 9:98–109
Sonis S et al (2010) Preliminary characterization of oral lesions associated with inhibitors of mammalian target of rapamycin in cancer patients. Cancer 116:210–215
Toi M et al (2009) Lapatinib monotherapy in patients with relapsed, advanced, or metastatic breast cancer: efficacy, safety, and biomarker results from Japanese patients phase II studies. Br J Cancer 101(10):1676–1682
Sawaki M et al (2004) Efficacy and safety of trastuzumab as a single agent in heavily pretreated patients with HER-2/neu-overexpressing metastatic breast cancer. Tumori 90(1):40–43
Keefe D, Gibson R (2007) Mucosal injury from targeted anticancer therapy. Support Care Cancer 15:483–490
Burris H (2004) Dual kinase inhibition in the treatment of breast cancer: initial experience with the EGFR/ErbB-2 inhibitor lapatinib. Oncologist 9:10–15
Geyer CE et al (2006) Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med 355(26):2733–2743
Al-Dasooqi N et al (2008) Trastuzumab induces gastrointestinal side effects in HER2-overexpressing breast cancer patients. Investig New Drugs 27:173–178
Fountzilas G et al (2001) Weekly paclitaxel as first-line chemotherapy and trastuzumab in patients with advanced breast cancer. A Hellenic Cooperative Oncology Group phase II study. Ann Oncol 12:1545–1551
Bartsch R et al (2007) Capecitabine and trastuzumab in heavily pretreated metastatic breast cancer. J Clin Oncol 25:3853–3858
Ruiz M et al (2008) Phase-II study of weekly schedule of trastuzumab, paclitaxel, and carboplatin followed by a week off every 28 days for HER2+ metastatic breast cancer. Cancer Chemother Pharmacol 62:1085–1090
Bowen J et al (2012) Development of a rat model of oral small molecule receptor tyrosine kinase inhibitor-induced diarrhoea. Cancer Biol Ther 13(13):1269-75
Peterson D, Keefe D, Sonis S (2012) New frontiers in mucositis. ASCO Educational Book. American Society of Clinical Oncology, Alexandria, pp. 545–61
Keefe D (1998) The effect of cytotoxic chemotherapy on the mucosa of the small intestine. Department of Medicine University of Adelaide, Adelaide
Pico J, Avila-Garavito A, Naccache P (1998) Mucositis: its occurence, consequences and treatment in the oncology setting. The Oncologist volume 3:p446–451
Sloan J et al (2002) Women experience greater toxicity with fluorouracil-based chemotherapy for colorectal cancer. J Clin Oncol 20:1491–1498
Pratesi N et al (2011) Association between single nucleotide polymorphisms in XRCC1 and RAD51 genes and clinical radiosensitivity in head and neck cancer. Radiother Oncol 99:356–362
West C, Dunning A, Rosenstein (2012) Genome-wide association studies and prediction of normal tissue toxicity. Sem Radiat Oncol 22:91–99
Thomas F et al (2011) Methylenetetrahydrofolate reductase genetic polymorphisms and toxicity to 5-FU-based chemoradiation in rectal cancer. Br J Cancer 105:1654–1662
Werbrouck J et al (2009) Acute normal tissue reactions in head-and-neck cancer patients treated with IMRT: influence of dose and association with genetic polymorphisms in DNA DSB repair genes. Int J Radiat Oncol Biol Phys 73:1187–1195
Schwab M et al (2008) Role of genetic and nongenetic factors for fluorouracil treatment-related severe toxicity: a prospective clinical trial by the German 5-FU Toxicity Study Group. J Clin Oncol 26:2131–2138
Cho H et al (2010) Glutathione-S-transferase genotypes influence the risk of chemotherapy-related toxicities and prognosis in Korean patients with diffuse large B-cell lymphoma. Cancer CGenet Cytogenet 198:40–46
Hahn T et al (2010) A deletion polymorphism in glutathione-S-transferase mu (GSTM1) and/or theta (GSTT1) is associated with an increased risk of toxicity after autologous blood and marrow transplantation. Biol Blood Marrow Transplant 16:801–808
Alterovitz G et al (2011) Personalized medicine for mucositis: bayesian networks identify unique gene clusters which predict the response to gamma-D-glutamyl-L-tryptophan (SCV-07) for the attenuation of chemoradiation-induced oral mucositis. Oral Oncol 47:951–955
Roseth A (2003) Determination of faecal calprotectin, a novel marker of organic gastrointestinal disorders. Dig Liver Dis 35:607–609
Lutgens L et al. (2005) Monitoring myeloablative therapy-induced small bowel toxicity by serum citrulline concentration: a comparison with sugar permeability tests. Cancer 103(1):191–9
Xanthinaki A et al (2008) Apoptosis and inflammation markers in oral mucositis in head and neck cancer patients receiving radiotherapy: preliminary report. Support Care Cancer 16:1025–1033
Conflict of interest
This project was carried out as part of the MASCC/ISOO Mucositis Guidelines Update, which was supported by BioAlliance Pharma and Helsinn Healthcare, NA. No industry representatives participated in the development of this manuscript in any way.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
An earlier version of this article was published in Volume 21, Issue 7, under DOI 10.1007/s00520-013-1810-y.
Rights and permissions
About this article
Cite this article
Al-Dasooqi, N., Sonis, S.T., Bowen, J.M. et al. Emerging evidence on the pathobiology of mucositis. Support Care Cancer 21, 3233–3241 (2013). https://doi.org/10.1007/s00520-013-1900-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1900-x