Abstract
Goal of work
The aim of the study was to investigate if the International Classification of Functioning, Disability and Health (ICF) model with clinical data from patients with breast-cancer-related lymphedema can predict their health-related quality of life (HRQL).
Materials and methods
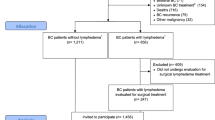
Sixty-one patients with breast-cancer-related lymphedema were recruited. Data were collected from records, including age, type(s) of surgery, number of dissected lymph nodes and history of radiotherapy and/or chemotherapy, duration of lymphedema, and duration between surgery and enrollment. Excessive arm volume, average arm symptom, function of upper extremity (U/E), and HRQL were assessed four times during and after patients’ treatment of lymphedema.
Results
The ICF model accounted for 20.5% to 55.6% variance in each domain of HRQL. Activity and participation reflected by U/E function were the most important factor, significantly predicting every domain of HRQL. Among measured impairments, average arm symptom was found to be most correlated with U/E function (r = 0.590, P < 0.05).
Conclusion
The ICF model consisting of clinical measures for patients with breast-cancer-related lymphedema can predict their HRQL. Activity and participation were the most important component. Arm symptoms rather than arm volume significantly correlated with U/E function. This might suggest that reducing arm symptoms is relatively more important while treating patients with breast-cancer-related lymphedema.
Similar content being viewed by others
Notes
SPSS version 11.0 (SPSS, Chicago, IL, USA).
References
Andersen L, Hojris I, Erlandsen M, Andersen J (2000) Treatment of breast-cancer-related lymphedema with or without manual lymphatic drainage—a randomized study. Acta Oncol 39:399–405
Bunce IH, Miroli BR, Hennessy JM, Ward LC, Jones LC (1994) Postmasectomy lymphoedema treatment and measurement. Med J Aust 161:125–128
Caban ME (2002) Trends in the evaluation of lymphedema. Lymphology 35:28–38
Carati CJ, Anderson SN, Gannon BJ, Piller NB (2003) Treatment of postmasecotmy lymphoedema with low level laser therapy. Cancer 98:1114–1122
Chen YW, Tsai HJ, Hung HC, Tsauo JY (2008) Reliability study of measurements for lymphedema in breast cancer patients. Am J Phys Med Rehabil 87:33–38
Clodius L, Deak L, Piller NB (1976) A new instrument for the evaluation of tissue tonicity in lymphoedema. Lymphology 9:1–5
Cohen SR, Payne DK, Tunkel RS (2001) Lymphedema. Cancer 92:980–987
Engel J, Kerr J, Schlesinger-Raab A, Sauer H, Holzel D (2003) Axilla surgery severely affects quality of life: results of a 5-year prospective study in breast cancer patients. [Erratum appears in Breast Cancer Res Treat 2003 Jul;80(2):233]. Breast Cancer Res Treat 79:47–57
Gosselink R, Rouffaer L, Vanhelden P, Piot W, Troosters T, Christiaens MR (2003) Recover of upper limb function after axillary dissection. J Surg Oncol 83:204–211
Hack TF, Cohen L, Katz J, Robson LS, Goss P (1999) Physical and psychological morbidity after axillary lymph node dissection for breast cancer. J Clin Oncol 17:143–149
Hladiuk M, Huchcroft S, Temple W, Schnurr BE (1992) Arm function after axillary dissection for breast cancer: a pilot study to provide parameter estimates. J Surg Oncol 50:47–52
Jette AM (2006) Toward a common language for function, disability, and health. Phys Ther 86:726–734
Kärki A, Simonen R, Mälkiä E, Selfe J (2005) Impairments, activity limitations and participation restrictions 6 and 12 months after breast cancer operation. J Rehabil Med 37:180–188
Ko DSC, Lerner R, Klose G, Cosimi AB (1998) Effective treatment of lymphoedema of the extremities. Arch Surg 133:452–458
Leduc O, Leduc A, Bourgeois P, Belgrado JP (1998) The physical treatment of upper limb edema. Cancer 83(12 Suppl American):2835–2839
Liao SF, Huang MS, Li SH, Chen IR, Wei TS, Kuo SJ, Chen ST, Hsu JC (2004) Complex decongestive physiotherapy for patients with chronic cancer-associated lymphedema. J Formos Med Assoc 103:344–348
Liang HW, Wang HK, Yao G, Horng YS, Hou SM (2004) Psychometric evaluation of the Taiwan version of the disability of the arm, shoulder, and hand (DASH) questionnaire. J Formos Med Assoc 103:773–779
Liu NF, Olszewski W (1992) Use of tonometry to assess lower extremity lymphedema. Lymphology 25:155–158
Maunsell E, Brisson J, Deschènes L (1992) Arm problems and psychological distress after surgery for breast cancer. Can J Surg 36:315–320
McKenzie DC, Kalda AL (2003) Effect of upper extremity exercise on secondary lymphedema in breast cancer patients: a pilot study. J Clin Oncol 21:463–466
Megens AM, Harris SR, Kim-Sing C, McKenzie DC (2001) Measurement of upper extremity volume in women after axillary dissection for breast cancer. Arch Phys Med Rehabil 82:1639–1644
Mondry TE, Riffenburgh RH, Johnstone PA (2004) Prospective trial of complete decongestive therapy for upper extremity lymphedema after breast cancer therapy. Cancer J 10:42–48
Motimer PS, Bates DO, Brassington HD, Stanton AWB, Strachan DP, Levick JR (1996) The prevalence of arm oedema following treatment for breast cancer. Q J Med 89:377–380
Nagi SZ (1964) A study in the evaluation of disability and rehabilitation potential: concepts, methods, and procedures. Am J Public Health Nations Health 54:1568–1579
Pain SJ, Purushotham AD (2000) Lymphoedema following surgery for breast cancer. Br J Surg 87:1128–1141
Passik SD, McDonald MV (1998) Psychosocial aspects of upper extremity lymphedema in women treated for breast carcinoma. Cancer 83(12 Suppl American):2817–2820
Pierce CA, Hanks RA (2006) Life satisfaction after traumatic brain injury and the World Health Organization model of disability. Am J Phys Med Rehabil 85:889–898
Rietman JS, Dijkstra PU, Debreczeni R, Geertzen JHB, Robinson DPH, De Vries J (2004) Impairments, disabilities and health related quality of life after treatment for breast cancer: a follow-up study 2.7 years after surgery. Disabil Rehabil 26:78–84
Sander AP, Hajer NM, Hemenway K, Miller AC (2002) Upper-extremity volume measurements in women with lymphedema: a comparison of measurements obtained via water displacement with geometrically determined volume. Phys Ther 82:1201–1212
Segerström K, Bjerle P, Nystrom A (1991) Importance of time in assessing arm and hand function after treatment of breast cancer. Scand J Plast Reconstr Surg Hand Surg 25:241–244
Szuba A, Achalu R, Rockson SG (2002) Decongestive lymphatic therapy for patients with breast carcinoma-associated lymphedema. A randomized, prospective study of a role for adjunctive intermittent pneumatic compression. Cancer 95:2260–2267
Szuba A, Cooke JP, Yousuf S, Rockson SG (2000) Decongestive lymphatic therapy for patients with cancer-related or primary lymphedema. Am J Med 109:296–300
Tobin MB, Lacey HJ, Meyer L, Mortimer PS (1993) The psychological morbidity of breast cancer-related arm swelling. Psychological morbidity of lymphoedema. Cancer 72:3248–3252
Taylor R, Jayasinghe UW, Koelmeyer L, Ung O, Boyages J (2006) Reliability and validity of arm volume measurements for assessment of lymphedema. Phys Ther 86:205–214
Tsai HJ, Liu YX, Tsauo JY (2005) Reliability study of lymphedema measurement. Formos J Phys Ther 30:124–131
Williams AF, Vadgama A, Franks PJ, Mortimer PS (2002) A randomized controlled crossover study of manual lymphatic drainage therapy in women with breast cancer-related lymphoedema. Eur J Cancer Care 11:254–261
World Health Organization (1980) International classification of impairments, disabilities, and handicaps: a manual of classification relating to the consequences of disease. World Health Organization, Geneva
World Health Organization (2001) ICF-International classification of functioning, disability and health. WHO Library, Geneva
Acknowledgments
The authors thank the participants and the National Science Council of the Republic of China for financial support under grant nos. NSC93-2314-B-002-118 and NSC94-2314-B-002-074, which made this study possible.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsauo, JY., Hung, HC., Tsai, HJ. et al. Can ICF model for patients with breast-cancer-related lymphedema predict quality of life?. Support Care Cancer 19, 599–604 (2011). https://doi.org/10.1007/s00520-010-0857-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-010-0857-2