Abstract
Objectives
We used intravenous midazolam and ketamine for children undergoing minor operative procedures with satisfactory results. We aimed to further evaluate its efficacy and adverse effects in pediatric ward setting.
Methods
This was a prospective study of all children undergoing minor operations with sedation in our pediatric general and oncology wards from July 1998 to June 1999. The procedures included lumber puncture±intrathecal chemotherapy, bone marrow aspiration±trephine biopsy, central venous catheter removal, skin biopsy, or their combination. All sedation procedures were started with midazolam 0.1 mg/kg and ketamine 1 mg/kg; they were increased gradually to 0.4 and 4 mg/kg, respectively, if necessary. Heart rate and SaO2 were continuously monitored.
Results
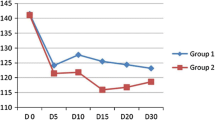
Altogether, 369 minor operations were performed in 112 patients (male:female=2:1, median age 6 years, range 5 months–17 years). All achieved adequate sedation, with 96% within 30 s and 75% required just the starting dose. Younger children required a higher dosage (p=0.003 for midazolam, p<0.001 for ketamine). The median recovery time was 87 min, with no association with age, sex, or dosage of sedation, but was longer in patients having hallucination (p=0.001). Adverse effects included tachycardia (27.9%), increased secretion (17.6%), agitation (13.6%), nausea and vomiting (9.2%), hallucination (8.7%), desaturation (8.4%), and cataleptic reaction (0.8%). All desaturation episodes were transient and responded to oxygen supplement alone. None developed bronchospasm or convulsion. Some adverse effects were dose-related. Half of the children who received 0.3 mg/kg midazolam developed desaturation.
Conclusions
Intravenous midazolam–ketamine can provide rapid, effective, and safe sedation for children undergoing minor operations in ward setting. Adverse effects are mild. Midazolam above 0.3 mg/kg should be used with caution.
Similar content being viewed by others
References
Acworth JP, Purdie D, Clark RC (2001) Intravenous ketamine plus midazolam is superior to intranasal midazolam for emergency paediatric procedural sedation. Emerg Med J 18:39–45
American Academy of Pediatrics Committee on Drugs (1992) Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures. Pediatrics 89:1110–1115
American College of Emergency Physicians (1998) Clinical policy for procedural sedation and analgesia in the emergency department. Ann Emerg Med 31:663–677
American Society of Anesthesiologists (1996) Practice guidelines for sedation and analgesia by non-anesthesiologists. A report by the American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Anesthesiology 84:459–471
Bailey PL, Pace NL, Ashburn MA, Moll JW, East KA, Stanley TH (1990) Frequent hypoxemia and apnea after sedation with midazolam and fentanyl. Anesthesiology 73:826–830
Berde C (1995) Pediatric oncology procedures: to sleep or perchance to dream? Pain 62:1–2
Bowdle TA, Radant AD, Cowley DS, Kharasch ED, Strassman RJ, Roy-Byrne PP (1998) Psychedelic effects of ketamine in healthy volunteers: relationship to steady-state plasma concentrations. Anesthesiology 88:82–88
Brown RT, Freeman WS, Perrin JM, Stein MT, Amler RW, Feldman HM, Pierce K, Wolraich ML (2001) Prevalence and assessment of attention-deficit/hyperactivity disorder in primary care settings. Pediatrics 107:E43
Cascorbi I (2003) Pharmacogenetics of cytochrome p4502D6: genetic background and clinical implication. Eur J Clin Invest 33(Suppl 2):17–22
Cote CJ, Karl HW, Notterman DA, Weinberg JA, McCloskey C (2000) Adverse sedation events in pediatrics: analysis of medications used for sedation. Pediatrics 106:633–644
D’Agostino J, Terndrup TE (1996) Comparative review of the adverse effects of sedatives used in children undergoing outpatient procedures. Drug Safety 14:146–157
Domino EF, Chodoff P, Corssen G (1965) Pharmacologic effects of Ci-581, a new dissociative anesthetic, in man. Clin Pharmacol Ther 40:279–291
Gilger MA, Spearman RS, Dietrich CL, Spearman G, Wilsey MJ Jr, Zayat MN (2004) Safety and effectiveness of ketamine as a sedative agent for pediatric GI endoscopy. Gastrointest Endosc 59:659–663
Godambe SA, Elliot V, Matheny D, Pershad J (2003) Comparison of propofol/fentanyl versus ketamine/midazolam for brief orthopedic procedural sedation in a pediatric emergency department. Pediatrics 112:116–123
Grant IS, Nimmo WS, McNicol LR, Clements JA (1983) Ketamine disposition in children and adults. Br J Anaesth 55:1107–1111
Green SM, Johnson NE (1990) Ketamine sedation for pediatric procedures: part 2, review and implications. Ann Emerg Med 19:1033–1046
Green SM, Klooster M, Harris T, Lynch EL, Rothrock SG (2001) Ketamine sedation for pediatric gastroenterology procedures. J Pediatr Gastroenterol Nutr 32:26–33
Green SM, Krauss B (2004) Clinical practice guideline for emergency department ketamine dissociative sedation in children. Ann Emerg Med 44:460–471
Green SM, Kuppermann N, Rothrock SG, Hummel CB, Ho M (2000) Predictors of adverse events with intramuscular ketamine sedation in children. Ann Emerg Med 35:35–42
Hostetler MA, Davis CO (2002) Prospective age-based comparison of behavioral reactions occurring after ketamine sedation in the ED. Am J Emerg Med 20:463–468
Ivani G, Vercellino C, Tonetti F (2003) Ketamine: a new look to an old drug. Minerva Anestesiol 69:468–471
Kennedy RM, McAllister JD (2000) Midazolam with ketamine: who benefits? Ann Emerg Med 35:297–299
Kennedy RM, Porter FL, Miller JP, Jaffe DM (1998) Comparison of fentanyl/midazolam with ketamine/midazolam for pediatric orthopedic emergencies. Pediatrics 102:956–963
Krauss B, Green SM (2000) Sedation and analgesia for procedures in children. N Engl J Med 342:938–945
Malviya S, Voepel-Lewis T, Tait AR, Merkel S (2000) Sedation/analgesia for diagnostic and therapeutic procedures in children. J Perianesth Nurs 15:415–422
Mankikian B, Cantineau JP, Sartene R, Clergue F, Viars P (1986) Ventilatory pattern and chest wall mechanics during ketamine anesthesia in humans. Anesthesiology 65:492–499
Marx CM, Stein J, Tyler MK, Nieder ML, Shurin SB, Blumer JL (1997) Ketamine–midazolam versus meperidine–midazolam for painful procedures in pediatric oncology patients. J Clin Oncol 15:94–102
Maughan B, Rowe R, Messer J, Goodman R, Meltzer H (2004) Conduct disorder and oppositional defiant disorder in a national sample: developmental epidemiology. J Child Psychol Psychiatry 45:609–621
Meyer S, Aliani S, Graf N, Gottschling S (2004) Inter- and intraindividual variability in ketamine dosage in repetitive invasive procedures in children with malignancies. Pediatr Hematol Oncol 21:161–166
Meyer S, Aliani S, Graf N, Reinhard H, Gottschling S (2003) Sedation with midazolam and ketamine for invasive procedures in children with malignancies and hematological disorders: a prospective study with reference to the sympathomimetic properties of ketamine. Pediatr Hematol Oncol 20:291–301
Miser AW, Ayesh D, Broda E et al (1988) Use of patient-controlled device for nitrous oxide administration to control procedure-related pain in children and young adults with cancer. Clin J Pain 4:5–10
Newman DH, Azer MM, Pitetti RD, Singh S (2003) When is a patient safe for discharge after procedural sedation? The timing of adverse effect events in 1367 pediatric procedural sedations. Ann Emerg Med 42:627–635
Ozdemir D, Kayserili E, Arslanoglu S, Gulez P, Vergin C (2004) Ketamine and midazolam for invasive procedures in children with malignancy: a comparison of routes of intravenous, oral, and rectal administration. J Trop Pediatr 50:224–228
Parker RI, Mahan RA, Giugliano D, Parker MM (1997) Efficacy and safety of intravenous midazolam and ketamine as sedation for therapeutic and diagnostic procedures in children. Pediatrics 99:427–431
Pellier I, Monrigal JP, Le Moine P, Rod B, Rialland X, Granry JC (1999) Use of intravenous ketamine–midazolam association for pain procedures in children with cancer. A prospective study. Paediatr Anaesth 9:61–68
Pena BM, Krauss B (1999) Adverse events of procedural sedation and analgesia in a pediatric emergency department. Ann Emerg Med 34:483–491
Pitetti RD, Singh S, Pierce MC (2003) Safe and efficacious use of procedural sedation and analgesia by nonanesthesiologists in a pediatric emergency department. Arch Pediatr Adolesc Med 157:1090–1096
Priestley SJ, Taylor J, McAdam CM, Francis P (2001) Ketamine sedation for children in the emergency department. Emerg Med (Fremantle) 13:82–90
Proudfoot J (1995) Analgesia, anesthesia, and conscious sedation. Emerg Med Clin North Am 13:357–379
Reich DL, Silvay G (1989) Ketamine: an update on the first twenty-five years of clinical experience. Can J Anaesth 36:186–197
Riavis M, Laux-End R, Carvajal-Busslinger MI, Tschappeler H, Bianchetti MG (1998) Sedation with intravenous benzodiazepine and ketamine for renal biopsies. Pediatr Nephrol 12:147–148
Rosen DA, Rosen KR (1998) Intravenous conscious sedation with midazolam in paediatric patients. Int J Clin Pract 52:46–50
Sectish TC (1997) Use of sedation and local anesthesia to prepare children for procedures. Am Fam Phys 55:909–916
Seigler RS, Avant MG, Gwyn DR, Lynch AL, Golding EM, Blackhurst DW, Wilfong DK (2001) A comparison of propofol and ketamine/midazolam for intravenous sedation of children. Pediatr Crit Care Med 2:20–23
Sherwin TS, Green SM, Khan A, Chapman DS, Dannenberg B (2000) Does adjunctive midazolam reduce recovery agitation after ketamine sedation for pediatric procedures? A randomized, double-blind, placebo-controlled trial. Ann Emerg Med 35:229–238
Slonim AD, Ognibene FP (1998) Sedation for pediatric procedures, using ketamine and midazolam, in a primarily adult intensive care unit: a retrospective evaluation. Crit Care Med 26:1900–1904
Tobias JD (1999) End-tidal carbon dioxide monitoring during sedation with a combination of midazolam and ketamine for children undergoing painful, invasive procedures. Pediatr Emerg Care 15:173–175
Tobias JD, Phipps S, Smith B, Mulhern RK (1992) Oral ketamine premedication to alleviate the distress of invasive procedures in pediatric oncology patients. Pediatrics 90:537–541
Wathen JE, Roback MG, Mackenzie T, Bothner JP (2000) Does midazolam alter the clinical effects of intravenous ketamine sedation in children? A double-blind, randomized, controlled, emergency department trial. Ann Emerg Med 36:579–588
Waxman K, Shoemaker WC, Lippmann M (1980) Cardiovascular effects of anesthetic induction with ketamine. Anesth Analg 59:355–358
Yaster M, Nichols DG, Deshpande JK, Wetzel RC (1990) Midazolam–fentanyl intravenous sedation in children: case report of respiratory arrest. Pediatrics 86:463–467
Yldzdas D, Yapcoglu H, Ylmaz HL (2004) The value of capnography during sedation or sedation/analgesia in pediatric minor procedures. Pediatr Emerg Care 20:162–165
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cheuk, D.K.L., Wong, W.H.S., Ma, E. et al. Use of midazolam and ketamine as sedation for children undergoing minor operative procedures. Support Care Cancer 13, 1001–1009 (2005). https://doi.org/10.1007/s00520-005-0821-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-005-0821-8