Summary
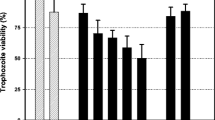
Trichomonosis, the disease caused by the protozoan parasite Trichomonas vaginalis, is the most common curable sexually transmitted disease with 174 million cases per year worldwide. The emerging resistance against the current standard therapy with metronidazole is pushing the search for alternative drugs. The purpose of this study was to determine the efficacy of curcumin, a derivate of Curcuma longa, on T. vaginalis. The effective concentrations (ECs) were evaluated using three strains of T. vaginaliswith different metronidazole susceptibilities (ATCC 30001, ATCC 30236 and ATCC 50138) and dilution series of curcumin in 24-well microtitre assays. Curcumin was shown to be highly effective against T. vaginalis, and the susceptibility of the different strains was not affected by an existing resistance to metronidazole. After 24 h of incubation, the EC50 ranged from 73.0 to 105.8 µg/ml and the EC90 from 216.3 to 164.9 µg/ml. In all strains tested, a 100 % eradication of all trichomonal cells within 24 h was reached at a concentration of 400 µg/ml curcumin, the 50-fold concentration still being very well tolerated by human mucosa. Altogether, curcumin seems to be a promising candidate for topical treatment of trichomonosis.
Zusammenfassung
Trichomonas vaginalis ist der Erreger der Trichomonose, der mit weltweit etwa 174 Mio. Neuinfektionen pro Jahr häufigsten heilbaren sexuell übertragbaren Erkrankung. Das zunehmende Auftreten von Stämmen, die gegen das derzeitige Standardtherapeutikum Metronidazol resistent sind, erregt Besorgnis. Ziel dieser Studie war es, die Wirksamkeit von Curcumin, einer aus der Wurzel der Pflanze Curcuma longa gewonnenen Substanz, auf T. vaginalis zu untersuchen. Hierfür wurden 3 T. vaginalisStämme unterschiedlicher Metronidazol-Resistenz (ATCC 30001, ATCC 30236 und ATCC 50138) auf ihre Empfänglichkeit gegenüber Curcumin in einem 24-well Mikrotiterplatten-System untersucht. Curcumin erwies sich als ausgesprochen wirksam gegen T. vaginalis, unabhängig von einer vorliegenden Metronidazol-Resistenz. Nach 24 h Inkubation lagen die EC50-Werte bei 73,0 bis 105,8 µg/ml und die EC90-Werte bei 216,3 bis 164,9 µg/ml. Alle 3 untersuchten Trichomonaden-Stämme konnten mit 400 µg/ml Curcumin innerhalb von 24 h vollständig abgetötet werden, die 50fache Konzentration wird von menschlicher Mukosa gut vertragen. Insgesamt erscheint Curcumin ein vielversprechender Kandidat für die topische Behandlung der Trichomonose.


Similar content being viewed by others
References
WHO. Global prevalence and incidence of selected curable sexually transmitted diseases. 2001. http://www.who.int/docstore/hiv/GRSTI/index.htm. Accessed 20 Dec 2013.
Sutton M, Sternberg M, Koumans EH, et al. The prevalence of Trichomonas vaginalis infection among reproductive-age women in the United States, 2001–2004. Clin Infect Dis. 2007;45(10):1319–26.
Geelen TH, Hoebe CJ, Dirks A, et al. Low positivity rate after systematic screening for Trichomonas vaginalis in three patient cohorts from general practitioners, STI clinic and a national population-based chlamydia screening study. Sex Transm Infect. 2013;89(6):532–4.
Allsworth JE, Ratner JA, Peipert JF. Trichomoniasis and other sexually transmitted infections: results from the 2001–2004 National Health and Nutrition Examination Surveys. Sex Transm Dis. 2009;36(12):738–44.
Shew ML, Fortenberry JD, Tu W, et al. Association of condom use, sexual behaviors, and sexually transmitted infections with the duration of genital human papillomavirus infection among adolescent women. Arch Pediatr Adolesc Med. 2006;160(2):151–6.
Gottlieb SL, Douglas JM Jr, Foster M, et al. Incidence of herpes simplex virus type 2 infection in 5 sexually transmitted disease (STD) clinics and the effect of HIV/STD risk-reduction counseling. J Infect Dis. 2004;190(6):1059–67.
McClelland RS, Sangare L, Hassan WM, et al. Infection with Trichomonas vaginalis increases the risk of HIV-1 acquisition. J Infect Dis. 2007;195(5):698–702.
Van Der Pol B, Kwok C, Pierre-Louis B, et al. Trichomonas vaginalis infection and human immunodeficiency virus acquisition in African women. J Infect Dis. 2008;197(4):548–54.
Kissinger P, Amedee A, Clark RA, et al. Trichomonas vaginalis treatment reduces vaginal HIV-1 shedding. Sex Transm Dis. 2009;36(1):11–6.
Schmid G, Narcisi E, Mosure D, et al. Prevalence of metronidazole-resistant Trichomonas vaginalis in a gynecology clinic. J Reprod Med. 2001;46(6):545–9.
Petrin D, Delgaty K, Bhatt R, et al. Clinical and microbiological aspects of Trichomonas vaginalis. Clin Microbiol Rev. 1998;11(2):300–17.
Hager WD. Treatment of metronidazole-resistant Trichomonas vaginalis with tinidazole: case reports of three patients. Sex Transm Dis. 2004;31(6):343–5.
Kulda J. Trichomonads, hydrogenosomes and drug resistance. Int J Parasitol. 1999;29(2):199–212.
Sobel JD, Nagappan V, Nyirjesy P. Metronidazole-resistant vaginal trichomoniasis—an emerging problem. N Eng J Med. 1999;341(4):292–3.
Narcisi EM, Secor WE. In vitro effect of tinidazole and furazolidone on metronidazole-resistant Trichomonas vaginalis. Antimicrob Agents Chemother. 1996;40(5):1121–5.
Kuriyama A, Jackson JL, Doi A, et al. Metronidazole-induced central nervous system toxicity: a systematic review. Clin Neuropharmacol. 2011;34(6):241–7.
Chacko J, Pramod K, Sinha S, et al. Clinical, neuroimaging and pathological features of 5-nitroimidazole-induced encephalo-neuropathy in two patients: insights into possible pathogenesis. Neurol India. 2011;59(5):743–7.
Connor TH, Stoeckel M, Evrard J, et al. The contribution of metronidazole and two metabolites to the mutagenic activity detected in urine of treated humans and mice. Cancer Res. 1977;37(2):629–33.
Lindmark DG, Muller M. Antitrichomonad action, mutagenicity, and reduction of metronidazole and other nitroimidazoles. Antimicrob Agents Chemother. 1976;10(3):476–82.
Koss CA, Baras DC, Lane SD, et al. Investigation of metronidazole use during pregnancy and adverse birth outcomes. Antimicrob Agents Chemother. 2012;56(9):4800–5.
Kazy Z, Puho E, Czeizel AE. Teratogenic potential of vaginal metronidazole treatment during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2005;123(2):174–8.
Centers for Disease Control and Prevention, Workowski KA, et al. Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep. 2006;55(RR-11):1–94.
Blaha C, Duchene M, Aspock H, et al. In vitro activity of hexadecylphosphocholine (miltefosine) against metronidazole-resistant and -susceptible strains of Trichomonas vaginalis. J Antimicrob Chemother. 2006;57(2):273–8.
Kranzler M. Pentamycin—a new option for the treatment of infections with Trichomonas vaginalis? Diploma thesis, University of Vienna; 2011. eBook 978-3-656-14565-32011.
Sharma RA, Gescher AJ, Steward WP. Curcumin: the story so far. Eur J Cancer. 2005;41(13):1955–68.
Buescher R, Yang L. Turmeric. In: Lauro GJ, Francis FJ, editors. Natural food colorants. New York: Marcel Dekker; 2000.
Perez-Arriaga L, Mendoza-Magana ML, Cortes-Zarate R, et al. Cytotoxic effect of curcumin on Giardia lamblia trophozoites. Acta Trop. 2006;98(2):152–61.
Khalafalla RE, Muller U, Shahiduzzaman M, et al. Effects of curcumin (diferuloylmethane) on Eimeria tenella sporozoites in vitro. Parasitol Res. 2011;108(4):879–86.
Mimche PN, Taramelli D, Vivas L. The plant-based immunomodulator curcumin as a potential candidate for the development of an adjunctive therapy for cerebral malaria. Malar J. 2011;10(Suppl. 1):S10.
Shahiduzzaman M, Dyachenko V, Khalafalla RE, et al. Effects of curcumin on Cryptosporidium parvum in vitro. Parasitol Res. 2009;105(4):1155–61.
Koide T, Nose M, Ogihara Y, et al. Leishmanicidal effect of curcumin in vitro. Biol Pharm Bull. 2002;25(1):131–3.
Changtam C, de Koning HP, Ibrahim H, et al. Curcuminoid analogs with potent activity against Trypanosoma and Leishmania species. Eur J Med Chem. 2010;45(3):941–56.
Allam G. Immunomodulatory effects of curcumin treatment on murine Schistosomiasis mansoni. Immunobiology. 2009;214(8):712–27.
Jordan WC, Drew CR. Curcumin—a natural herb with anti-HIV activity. J Natl Med Assoc. 1996;88(6):333.
Barthelemy S, Vergnes L, Moynier M, et al. Curcumin and curcumin derivatives inhibit Tat-mediated transactivation of type 1 human immunodeficiency virus long terminal repeat. Res Virol. 1998;149(1):43–52.
Yadav VS, Mishra KP, Singh DP, et al. Immunomodulatory effects of curcumin. Immunopharmacol Immunotoxicol. 2005;27(3):485–97.
Chainani-Wu N. Safety and anti-inflammatory activity of curcumin: a component of tumeric (Curcuma longa). J Altern Complement Med. 2003;9(1):161–8.
Wei QY, Chen WF, Zhou B, et al. Inhibition of lipid peroxidation and protein oxidation in rat liver mitochondria by curcumin and its analogues. Biochim Biophys Acta. 2006;1760(1):70–7.
Devasena T, Rajasekaran KN, Gunasekaran G, et al. Anticarcinogenic effect of bis-1,7-(2-hydroxyphenyl)-hepta-1,6-diene-3,5-dione a curcumin analog on DMH-induced colon cancer model. Pharmacol Res. 2003;47(2):133–40.
Srivivasan A, Menon VP, Periaswamy V, et al. Protection of pancreatic beta-cell by the potential antioxidant bis-o-hydroxycinnamoyl methane, analogue of natural curcuminoid in experimental diabetes. J Pharm Pharm Sci. 2003;6(3):327–33.
Clark CG, Diamond LS. Methods for cultivation of luminal parasitic protists of clinical importance. Clin Microbiol Rev. 2002;15(3):329–41.
Fang HY, Chen SB, Guo DJ, et al. Proteomic identification of differentially expressed proteins in curcumin-treated MCF-7 cells. Phytomedicine. 2011;18(8–9):697–703.
Wang L, Wang L, Song R, et al. Targeting sarcoplasmic/endoplasmic reticulum Ca2+-ATPase 2 by curcumin induces ER stress-associated apoptosis for treating human liposarcoma. Mol Cancer Ther. 2011;10(3):461–71.
He ZY, Shi CB, Wen H, et al. Upregulation of p53 expression in patients with colorectal cancer by administration of curcumin. Cancer Investig. 2011;29(3):208–13.
Elad S, Meidan I, Sellam G, et al. Topical curcumin for the prevention of oral mucositis in pediatric patients: case series. Altern Ther Health Med. 2013;19(3):21–4.
Manifar S, Obwaller A, Gharehgozloo A, et al. Curcumin gel in the treatment of minor aphthous ulcer: a randomized, placebo-controlled trial. J Med Plants. 2012;11(41):40–5.
Heng MC. Wound healing in adult skin: aiming for perfect regeneration. Int J Dermatol. 2011;50(9):1058–66.
Helson L. Curcumin (diferuloylmethane) delivery methods: a review. Biofactors. 2013;39(1):21–6.
Patel MB, Mandal S, Rajesh KS. Formulation and kinetic modeling of curcumin loaded intranasal mucoadhesive microemulsion. J Pharm Bioallied Sci. 2012;4(Suppl. 1):S81–3.
Berginc K, Skalko-Basnet N, Basnet P, et al. Development and evaluation of an in vitro vaginal model for assessment of drug’s biopharmaceutical properties: curcumin. AAPS PharmSciTech. 2012;13(4):1045–53.
Di Pierro F, Rapacioli G, Di Maio EA, et al. Comparative evaluation of the pain-relieving properties of a lecithinized formulation of curcumin (Meriva()), nimesulide, and acetaminophen. J Pain Res. 2013;6:201–5.
Kulac M, Aktas C, Tulubas F, et al. The effects of topical treatment with curcumin on burn wound healing in rats. J Mol Histol. 2013;44(1):83–90.
Acknowledgements
The authors would like to thank the members of the workgroup Molecular Parasitology of the Institute of Specific Prophylaxis and Tropical Medicine for their technical assistance.
Conflict of interest
Orphanidis Pharma Research is patent holder of a formulation comprising curcumin and PEG and license holder of a cosmetic product comprising curcumin. Benjamin Wachter, Michael Syrowatka and Julia Walochnik have no conflicts of interest to declare.
Ethical approval
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wachter, B., Syrowatka, M., Obwaller, A. et al. In vitro efficacy of curcumin on Trichomonas vaginalis . Wien Klin Wochenschr 126 (Suppl 1), 32–36 (2014). https://doi.org/10.1007/s00508-014-0522-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-014-0522-8