Summary
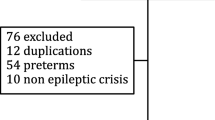
OBJECTIVES: To investigate the frequency of malformations, fetal growth retardation, cerebral hemorrhage and neonatal withdrawal symptoms in newborns exposed to antiepileptic drugs (AEDs) in utero. DESIGN: Population of the northeastern part of Slovenia (pregnant women and newborns between 1998 and 2002). METHODS: Data on newborns born between 1998 and 2002 of 37 epileptic mothers taking AEDs in pregnancy, of 32 epileptic mothers not taking AEDs in pregnancy and of 211 mothers healthy in pregnancy were ascertained from hospital obstetric and neonatal records and included in the study. The health status of 270 newborns was assessed. Main outcome measures: frequency of congenital malformations, growth retardation (SFD), intracranial hemorrhage, feeding problems and withdrawal symptoms. RESULTS: In the group not exposed to antiepileptic drugs (32 neonates), two (2.9%) had germinal matrix hemorrhage grade I, one (1.4%) was small for date (SFD) and one (1.4%) had feeding problems. In the group exposed to antiepileptic drugs (37 neonates), nine (13%) had germinal matrix hemorrhage grade I, six (8.6%) were SFD, five (7.24%) had feeding problems, four (5.8%) had withdrawal symptoms and three (4.3%) "macro" congenital anomalies. Among neonatal problems in the control non-exposed group of newborns of 211 healthy women we identified 23 (10.9%) newborns who were SFD, 5 (2.4%) cases with germinal matrix hemorrhage grade I, 5 (2.4%) cases with major congenital malformations and 7 (3.3%) cases with feeding problems. CONCLUSIONS: Prenatal antiepileptic drug exposure in the setting of maternal epilepsy is associated with increased risk of neonatal morbidity. In our study a particularly significant connection was established between carbamazepine therapy during pregnancy and cerebral hemorrhage in the neonates.
Similar content being viewed by others
References
Olafsson E, Hallgrimson JT, Hauser WA, Ludwigsson P, Gudmundsson G (1998) Pregnancies of women with epilepsy: a population based study in Iceland. Epilepsia 39: 887–892
Kallen B (1986) A register study of maternal epilepsy and delivery outcome with special reference to drug use. Acta Neurol Scand 73: 253–259
Sonneveld SW, Correy JF (1990) Outcome of pregnancies complicated by epilepsy in Tasmania 1981–1988. Aust NZ J Obstet Gynecol 30: 286–289
Russell AJC, Macpherson H, Cairnie V, Brodie MJ (1996) The care of pregnant woman with epilepsy. Seizure 5: 271–275
Zahn C (1998) Neurologic care of pregnant women with epilepsy. Epilepsia 39 [Suppl 8]: S26–S31
Sabers A, A Rogvi-Hansen B, Dam M, et al (1998) Pregnancy and epilepsy. A retrospective study of 151 pregnancies. Acta Neurol Scand 97: 164–170
Ried S, Beck-Mannagetta G (1996) Epilepsy, pregnancy and child. Blackwell Science. Berlin Vienna
Jick SS, Terris BZ (1997) Anticonvulsants and congenital malformations. Pharmacotherapy 17: 561–564
Bertollini R, Mastroiacovo P, Segni G (1985) Maternal epilepsy and birth defects. A case control study in the Italian Multicentric Registry of birth defects. Eur J Epidemiol 1: 67–72
Kaneko S, Battino D, Andermann E, et al (1999) Congenital malformations due to antiepileptic drugs. Epilepsy Res 33: 145–158
Omtzigt JG, Los FJ, Hagenaars AM, Stewart PA, Sahs ES, Lindhout D (1992) Prenatal diagnosis of spina bifida aperta after first trimester valproate exposure. Prenat Diagn 12: 893–897
Lindhout D, Omtzigt JG (1994) Teratogenic effects of antiepileptic drugs. Implications for the management of epilepsy in women of childbearing age. Epilepsia 35 [Suppl 4]: S19–S28
Battino D, Granata T, Binelli S, et al (1992) Intrauterine growth in the offspring of epileptic mothers. Acta Neurol Scand 86: 555–557
Steegers-Theunissen RP, Renier WO, Borm GF, et al (1994) Factors influencing the risk of abnormal pregnancy outcome in epileptic women: a multi centre prospective study. Epilepsia Res 18: 261–269
Sawhney H, Vasishta K, Suri V, Khunnu B, Goel P, Sawhney IM (1996) Pregnancy with epilepsy – a retrospective analysis. Int J Gynecol Obstet 54: 17–22
Ornoy A, Cohen E (1996) Outcome of children born to epileptic mothers treated with carbamazepine during pregnancy. Arch Dis Child 75: 517–520
Dessens AB, Cohen-Kettenis PT, Mellenbergh GJ, Koppe JG, et al (2000) Association of prenatal phenobarbital and phenitoin exposure with small head size at birth and with learning problems. Acta Pediatr 89: 533–541
Volpe JJ (2000) Neurology of the newborn, 4th edn. WB Saunders, Philadelphia
Speidel BD, Meadow SR (1972) Maternal epilepsy and abnormalities of the fetus and newborn. Lancet 2: 839
Morrell MJ (1998) Guidelines for the care of women with epilepsy. Neurology 51: S21–S27
Morrell MJ (1998) Guidelines for the care of women with epilepsy. Neurology 51: S21–S27
Kaneko S, Battino D, Andermann E, et al (1999) Congenital malformations due to antiepileptic drugs. Epilepsy Res 33: 145–158
Wide K, Winbladh B, Tomson T, et al (2000) Psychomotor development and minor anomalies in children exposed to antiepileptic drugs in utero: a prospective population based study. Dev Med Child Neurol 42: 87–92
Fonager K, Larsen H, Pedersen L, Sorensen HT (2000) Birth outcomes in women exposed to anticovulsant drugs. Acta Neurol Scand 101: 289–294
Devinsky O (1996) Quality of life with epilepsy. In: Willie E (ed) The treatment of epilepsy, 2nd edn. Williams and Williams, Baltimore, pp 1145–1150
Lindhout D, Meinardi H, Meier JW, Nau H (1992) Antiepileptic drugs and teratogenesis in two consecutive cohorts. Changes in prescription policy paralleled by changes in pattern of malformations. Neurology 42: 94–110
Paulson GW, Paulson RB (1981) Teratogenic effects of anticonvulsants. Arch Neurol 38: 140
Oguni M, Dansky L, Andermann E, et al (1992) Improved pregnancy outcome in epileptic women in the last decade. The relationship to maternal anticonvulsant therapy. Brain Dev 14: 371–380
Hanson JW, Smith DW (1975) The fetal hydantoin syndrome. J Pediatr 87: 285
Seip M (1976) Growth retardation, dysmorphic facies and minor malformations following massive exposure to phenobarbitone in utero. Acta Pediatr Scand 65: 617
Hoyme HE, Clericuzio CL (1985) Fetal primidone effects. Pediatr Res 19: 326A
Vestermark V, Vestermark S (1991) Teratogenic effect of carbamazepine. Arch Dis Child 66: 641–642
Buehler BA, Delimont D, Van Waes M, Finell RH (1990) Prenatal prediction of fetal hydantoin syndrome. N Engl J Med 322: 1567–1572
Finell RH, Buehler BA, Kerr BM, et al (1992) Clinical and experimental studies linking oxidative metabolism to phenitoin induced teratogenesis. Neurology 42: 25–31
Dansky LV, Rosenblatt DS, Andermann E (1992) Mechanisms of teratogenesis: folic acid and antiepileptic therapy. Neurology 42: 32–42
Thisted E, Ebbesen F (1993) Malformations after exposure to valproate in utero. Arch Dis Child 69: 288–291
Kozma C (2001) Valproic acid embriopathy. Am J Med Genet 98: 168–175
Malm H, Kajantie E, Kivirikko S, Kaariainen H, Peippo M, Somer M (2002) Valproate embryopathy in three sets of siblings: further proof of hereditary susceptibility. Neurology 59: 630–632
Renzulli P, Tuchschmid P, Eich G, et al (1998) Early Vit K deficiency bleeding after maternal Phenobarbital intake. Eur J Pediatr 157: 663–665
Cornelissen M, Steegerstheunissen R, Kollee L, et al (1993) Increased incidence of neonatal vitamin K deficiency resulting from maternal anticonvulsant therapy. Am J Obstet Gynecol 16: 923–928
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burja, S., Rakovec-Felser, Z., Treiber, M. et al. The frequency of neonatal morbidity after exposure to antiepileptic drugs in utero. Wien Klin Wochenschr 118 (Suppl 2), 12–16 (2006). https://doi.org/10.1007/s00508-006-0539-8
Issue Date:
DOI: https://doi.org/10.1007/s00508-006-0539-8