Abstract
Background
Pediatric patients on maintenance hemodialysis (HD) are at risk of both malnutrition and fluid overload. This pilot study aimed to assess correlates of normalized protein catabolic rate (nPCR) in adolescents on chronic HD, in particular fluid status markers.
Methods
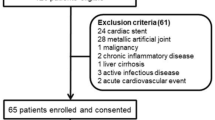
All patients aged 10–18 years on chronic HD in our center between 2017 and 2019 were enrolled. For each patient, mean nPCR was calculated and correlations with the following parameters investigated: dry body weight change in subsequent 3 months in kg (∆BW) and percentage of BW (∆BW%), change in body mass index (∆BMI), preHD systolic and diastolic blood pressure (SBP, DBP), residual urine output, biochemistry, and blood volume monitoring–derived first hour refill index (RI), calculated as ratio between ultrafiltration rate and reduction in relative blood volume in first hour of dialysis.
Results
Seventy-nine nPCR determinations were collected in 23 patients, median age 14.8 years. nPCR significantly correlated with ∆BW, ∆BW%, ∆BMI, spKT/V, and preHD serum creatinine, and negatively correlated with age, DBP SDS (r=−0.466, p=0.025) and RI (r=−0.435, p=0.043). RI was significantly higher in patients with nPCR <1 than those with nPCR above this threshold: 3.2 (1.9–4.7) vs. 1.4 (0.7–1.8) ml/kg/h/% (p=0.021). At multivariable analysis, nPCR remained positively correlated with creatinine and spKt/V, and inversely correlated with RI.
Conclusions
nPCR is a significant predictor of weight change in adolescents on maintenance HD, and seems associated with creatinine and dialysis adequacy. Inverse correlation with RI suggests possible associations between malnutrition and fluid overload, but larger prospective studies are needed to confirm this.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information.


Similar content being viewed by others
References
Fouque D, Kalantar-Zadeh K, Kopple J, Cano N, Chauveau P, Cuppari L, Franch H, Guarnieri G, Ikizler TA, Kaysen G, Lindholm B, Massy Z, Mitch W, Pineda E, Stenvinkel P, Trevinho-Becerra A, Wanner C (2008) A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int 73:391–398
Fischbach M, Dheu C, Seuge L, Orfanos N (2009) Hemodialysis and nutritional status in children: malnutrition and cachexia. J Ren Nutr 19:91–94
Edefonti A, Paglialonga F, Picca M (2006) A prospective multicentre study of nutritional status in children on chronic peritoneal dialysis. Nephrol Dial Transplant 21:1946–1951
Mak RH, Cheung WW, Zhan JY, Shen Q, Foster BJ (2012) Cachexia and protein-energy wasting in children with chronic kidney disease. Pediatr Nephrol 27:173–181
Edefonti A, Picca M, Damiani B, Garavaglia R, Loi S, Ardissino G, Marra G, Ghio L (2001) Prevalence of malnutrition assessed by bioimpedance analysis and anthropometry in children on peritoneal dialysis. Perit Dial Int 21:172–179
Brem AS, Lambert C, Hill C, Kitsen J, Shemin DG (2002) Prevalence of protein malnutrition in children maintained on peritoneal dialysis. Pediatr Nephrol 17:527–530
Foster BJ, Leonard MB (2005) Nutrition in children with chronic kidney disease: pitfalls of popular assessment methods. Perit Dial Int 25(Suppl 3):S143–S146
Paglialonga F, Edefonti A (2009) Nutrition assessment and management in children on peritoneal dialysis. Pediatr Nephrol 24:721–730
Grupe WE, Harmon WE, Spinozzi NS (1983) Protein and energy requirements in children receiving chronic hemodialysis. Kidney Int Suppl 15:S6–S10
Harmon WE, Spinozzi NS, Sargent JR, Grupe WE (1979) Determination of protein catabolic rate (PCR) in children on hemodialysis by urea kinetic modelling. Pediatr Res 13:513–517
National Kidney Foundation Kidney Disease Quality Outcome Initiative (K/DOQI) (2009) Clinical Practice Guideline for Nutrition in Children with CKD: 2008 Update. Am J Kidney Dis 53(Suppl 2):S1–S123
Borah MF, Schoenfeld PY, Gotch FA, Sargent JA, Wolfsen M, Humphreys MH (1978) Nitrogen balance during intermittent dialysis therapy of uremia. Kidney Int 14:491–500
Goldstein SL, Baronette S, Vital Gambrell T, Currier H, Brewer ED (2002) nPCR assessment and IDPN treatment of malnutrition in pediatric hemodialysis patients. Pediatr Nephrol 17:531–534
Juarez-Congelosi M, Orellana P, Goldstein SL (2007) Normalized protein catabolic rate versus serum albumin as a nutrition status marker in pediatric patients receiving hemodialysis. J Ren Nutr 17:269–274
Orellana P, Juarez-Congelosi M, Goldstein SL (2005) Intradialytic parenteral nutrition treatment and biochemical marker assessment for malnutrition in adolescent maintenance hemodialysis patients. J Ren Nutr 15:312–317
Haskin O, Sutherland SM, Wong CJ (2017) The effect of intradialytic intralipid therapy in pediatric hemodialysis patients. J Ren Nutr 27:132–137
Rees LO, Shaw V (2009) Nutrition in children with CRF and on dialysis. Pediatr Nephrol 24:475–484
Dekker MJE, Konings C, Canaud B, van der Sande FM, Stuard S, Raimann JG, Öztürk E, Usvyat L, Kotanko P, Kooman JP (2018) Interactions between malnutrition, inflammation, and fluid overload and their associations with survival in prevalent hemodialysis Patients. J Ren Nutr 28:435–444
Demirci MS, Demirci C, Ozdogan O, Kircelli F, Akcicek F, Basci A, Ok E, Ozkahya M (2011) Relations between malnutrition-inflammation-atherosclerosis and volume status. The usefulness of bioimpedance analysis in peritoneal dialysis patients. Nephrol Dial Transplant 26:1708–1716
Kang SH, Do JY (2020) Effects of volume status on body composition in incident peritoneal dialysis patients. Eur J Clin Nutr 74:633–641
Cheng LT, Tang W, Wang T (2005) Strong association between volume status and nutritional status in peritoneal dialysis patients. Am J Kidney Dis 45:891–902
Guo Q, Yi C, Li J, Wu X, Yang X, Yu X (2013) Prevalence and risk factors of fluid overload in Southern Chinese continuous ambulatory peritoneal dialysis patients. PLoS One 8:e53294
Paglialonga F, Consolo S, Galli MA, Testa S, Edefonti A (2015) Interdialytic weight gain in oligoanuric children and adolescents on chronic hemodialysis. Pediatr Nephrol 30:999–1005
Fischbach M, Zaloszyc A, Shroff R (2015) The interdialytic weight gain: a simple marker of left ventricular hypertrophy in children on chronic haemodialysis. Pediatr Nephrol 30:859–863
Flythe JE, Chang TI, Gallagher MP, Lindley E, Madero M, Sarafidis PA, Unruh ML, Wang AY, Weiner DE, Cheung M, Jadoul M, Winkelmayer WC, Polkinghorne KR, Conference Participants (2020) Blood pressure and volume management in dialysis: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int 97:861–876
Hayes W, Paglialonga F (2019) Assessment and management of fluid overload in children on dialysis. Pediatr Nephrol 34:233–242
Milani GP, Groothoff JW, Vianello FA, Fossali EF, Paglialonga F, Edefonti A, Agostoni C, Consonni D, van Harskamp D, van Goudoever JB, Schierbeek H, Oosterveld MJ (2017) Bioimpedance and fluid status in children and adolescents treated with dialysis. Am J Kidney Dis 69:428–435
Paglialonga F, Consolo S, Edefonti A, Montini G (2018) The first hour refill index: a promising marker of volume overload in children and young adults on chronic hemodialysis. Pediatr Nephrol 33:1209–1214
Depner TA, Daugirdas JT (1996) Equations for normalized protein catabolic rate based on two-point modeling of hemodialysis urea kinetics. J Am Soc Nephrol 7:780–785
Paglialonga F, Ardissino G, Galli MA, Scarfia RV, Testa S, Edefonti A (2012) Bioimpedance analysis and cardiovascular status in pediatric patients on chronic hemodialysis. Hemodial Int 16(Suppl 1):S20–S25
Paglialonga F, Lopopolo A, Scarfia RV, Galli MA, Consolo S, Brivio A, Grassi MR, Salera S, Edefonti A (2013) Correlates of exercise capacity in pediatric patients on chronic hemodialysis. J Ren Nutr 23:380–386
Marsenic O, Peco-Antić A, Jovanović O (2001) Effect of dialysis dose on nutritional status of children on chronic hemodialysis. Nephron 88:273–275
Cano FJ, Azocar MA, Delucchi MA, Rodriguez EE, Marin VS, Diaz ED, Mazuel N (2004) Nitrogen balance studies and Kt/V urea in children undergoing chronic peritoneal dialysis. Adv Perit Dial 20:245–250
van Hoeck KJ, Rusthoven E, Vermeylen L, Vandesompel A, Marescau B, Lilien M, Schroder CH (2003) Nutritional effects of increasing dialysis dose by adding an icodextrin daytime dwell to Nocturnal Intermittent Peritoneal Dialysis (NIPD) in children. Nephrol Dial Transplant 18:1383–1387
Buur T, Smye SW, Bradbury M, Will EJ (1995) The correlation between protein catabolic rate and Kt/V in hemodialysis is not a mathematical artifact. Int J Artif Organs 18:351–354
Agarwal R, Kelley K, Light RP (2008) Diagnostic utility of blood volume monitoring in hemodialysis patients. Am J Kidney Dis 51:242–254
Maduell F, Arias M, Massó E, Fontseré N, Carrera M, Vera M, Cases A, Campistol JM (2013) Sensitivity of blood volume monitoring for fluid status assessment in hemodialysis patients. Blood Purif 35:202–208
Koomans HA, Geers AB, Mees EJ (1984) Plasma volume recovery after ultrafiltration in patients with chronic renal failure. Kidney Int 26:848–854
Wizemann V, Leibinger A, Mueller K, Nilson A (1995) Influence of hydration state on plasma volume changes during ultrafiltration. Artif Organs 19:416–419
Guzzo I, Mancini E, Kengne Wafo S, Ravà L, Picca S (2009) Residual renal function and nutrition in young patients on chronic hemodialysis. Pediatr Nephrol 24:1391–1397
Fischbach M, Terzic J, Menouer S, Dheu C, Seuge L, Zalosczic A (2010) On line haemodiafiltration promotes catch-up growth in children on chronic dialysis. Nephrol Dial Transplant 25:867–873
Shroff R, Smith C, Ranchin B, Bayazit AK, Stefanidis CJ, Askiti V, Azukaitis K, Canpolat N, Ağbaş A, Aitkenhead H, Anarat A, Aoun B, Aofolaju D, Bakkaloglu SA, Bhowruth D, Borzych-Dużałka D, Bulut IK, Büscher R, Deanfield J, Dempster C, Duzova A, Habbig S, Hayes W, Hegde S, Krid S, Licht C, Litwin M, Mayes M, Mir S, Nemec R, Obrycki L, Paglialonga F, Picca S, Samaille C, Shenoy M, Sinha MD, Spasojevic B, Stronach L, Vidal E, Vondrák K, Yilmaz A, Zaloszyc A, Fischbach M, Schmitt CP, Schaefer F (2019) Effects of hemodiafiltration versus conventional hemodialysis in children with ESKD: the HDF, Heart and Height Study. J Am Soc Nephrol 30:678–691
Author information
Authors and Affiliations
Contributions
FP and SC contributed to the study conception and design. Data collection was performed by FP, SC, MA, and OC. Data analysis was performed by FP. The first draft of the manuscript was written by FP and revised by SC, MB, OC, MRG, and GM. Each author contributed important intellectual content during manuscript drafting or revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The study was approved by the local Institutional Review Board and conformed to the Declaration of Helsinki.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
Graphical abstract: Nutritional status and volume control in adolescents on chronic hemodialysis (PPTX 55 kb)
Rights and permissions
About this article
Cite this article
Paglialonga, F., Consolo, S., Brambilla, M. et al. Nutritional status and volume control in adolescents on chronic hemodialysis. Pediatr Nephrol 36, 3733–3740 (2021). https://doi.org/10.1007/s00467-021-05089-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05089-6