Abstract
Background
Children presenting with proliferative lupus nephritis (LN) are treated with intensified immunosuppressive protocols. Data on renal outcome and treatment toxicity is scare.
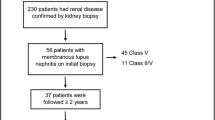
Methods
Twelve-month renal outcome and comorbidity were assessed in 79 predominantly Caucasian children with proliferative LN reported to the Lupus Nephritis Registry of the German Society of Paediatric Nephrology diagnosed between 1997 and 2015.
Results
At the time of diagnosis, median age was 13.7 (interquartile range 11.8–15.8) years; 86% showed WHO histology class IV, nephrotic range proteinuria was noted in 55%, and median estimated glomerular filtration rate amounted to 75 ml/min/1.73 m2. At 12 months, the percentage of patients with complete and partial remission was 38% and 41%, respectively. Six percent of patients were non-responders and 15% presented with renal flare. Nephrotic range proteinuria at the time of diagnosis was associated with inferior renal outcome (odds ratio 5.34, 95% confidence interval 1.26–22.62, p = 0.02), whereas all other variables including mode of immune-suppressive treatment (e.g., induction treatment with cyclophosphamide (IVCYC) versus mycophenolate mofetil (MMF)) were not significant correlates. Complications were reported in 80% of patients including glucocorticoid toxicity in 42% (Cushingoid appearance, striae distensae, cataract, or osteonecrosis), leukopenia in 37%, infection in 23%, and menstrual disorder in 20%. Growth impairment, more pronounced in boys than girls, was noted in 78% of patients.
Conclusions
In this cohort of juvenile proliferative LN, renal outcome at 12 months was good irrespectively if patients received induction treatment with MMF or IVCYC, but glucocorticoid toxicity was very high underscoring the need for corticoid sparing protocols.

Graphical abstract


Similar content being viewed by others
References
Brunner HI, Gladman DD, Ibanez D, Urowitz MD, Silverman ED (2008) Difference in disease features between childhood-onset and adult-onset systemic lupus erythematosus. Arthritis Rheum 58:556–562
Marks SD, Sebire NJ, Pilkington C, Tullus K (2007) Clinicopathological correlations of paediatric lupus nephritis. Pediatr Nephrol 22:77–83
Bogdanovic R, Nikolic V, Pasic S, Dimitrijevic J, Lipkovska-Markovic J, Eric-Marinkovic J, Ognjanovic M, Minic A, Stajic N (2004) Lupus nephritis in childhood: a review of 53 patients followed at a single center. Pediatr Nephrol 19:36–44
Emre S, Bilge I, Sirin A, Kilicaslan I, Nayir A, Oktem F, Uysal V (2001) Lupus nephritis in children: prognostic significance of clinicopathological findings. Nephron 87:118–126
Cameron JS (1994) Lupus nephritis in childhood and adolescence. Pediatr Nephrol 8:230–249
Moroni G, Quaglini S, Gallelli B, Banfi G, Messa P, Ponticelli C (2007) The long-term outcome of 93 patients with proliferative lupus nephritis. Nephrol Dial Transplant 22:2531–2539
Lee BS, Cho HY, Kim EJ, Kang HG, Ha IS, Cheong HI, Kim JG, Lee HS, Choi Y (2007) Clinical outcomes of childhood lupus nephritis: a single center's experience. Pediatr Nephrol 22:222–231
Lupus nephritis: prognostic factors and probability of maintaining life-supporting renal function 10 years after the diagnosis. gruppo italiano per lo studio della nefrite lupica (GISNEL) (1992) Am J Kidney Dis 19: 473–479
Ruggiero B, Vivarelli M, Gianviti A, Benetti E, Peruzzi L, Barbano G, Corona F, Ventura G, Pecoraro C, Murer L, Ghiggeri GM, Pennesi M, Edefonti A, Coppo R, Emma F (2013) Lupus nephritis in children and adolescents: results of the italian collaborative study. Nephrol Dial Transplant 28:1487–1496
Tanaka H, Tsugawa K, Oki E, Suzuki K, Ito E (2008) Mizoribine intermittent pulse protocol for induction therapy for systemic lupus erythematosus in children: an open-label pilot study with five newly diagnosed patients. Clin Rheumatol 27:85–89
Bertsias GK, Tektonidou M, Amoura Z, Aringer M, Bajema I, Berden JH, Boletis J, Cervera R, Dorner T, Doria A, Ferrario F, Floege J, Houssiau FA, Ioannidis JP, Isenberg DA, Kallenberg CG, Lightstone L, Marks SD, Martini A, Moroni G, Neumann I, Praga M, Schneider M, Starra A, Tesar V, Vasconcelos C, van Vollenhoven RF, Zakharova H, Haubitz M, Gordon C, Jayne D, Boumpas DT, European League Against Rheumatism and European Renal Association-European Dialysis and Transplant Association (2012) Joint european league against rheumatism and european renal association-european dialysis and transplant association (EULAR/ERA-EDTA) recommendations for the management of adult and paediatric lupus nephritis. Ann Rheum Dis 71:1771–1782
Hahn BH, MA MM, Wilkinson A, Wallace WD, Daikh DI, Fitzgerald JD, Karpouzas GA, Merrill JT, Wallace DJ, Yazdany J, Ramsey-Goldman R, Singh K, Khalighi M, Choi SI, Gogia M, Kafaja S, Kamgar M, Lau C, Martin WJ, Parikh S, Peng J, Rastogi A, Chen W, Grossman JM, American College of Rheumatology (2012) American college of rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res 64:797–808
Yu F, Haas M, Glassock R, Zhao MH (2017) Redefining lupus nephritis: clinical implications of pathophysiologic subtypes. Nat Rev Nephrol 13:483–495
Mina R, von Scheven E, Ardoin SP, Eberhard BA, Punaro M, Ilowite N, Hsu J, Klein-Gitelman M, Moorthy LN, Muscal E, Radhakrishna SM, Wagner-Weiner L, Adams M, Blier P, Buckley L, Chalom E, Chedeville G, Eichenfield A, Fish N, Henrickson M, Hersh AO, Hollister R, Jones O, Jung L, Levy D, Lopez-Benitez J, McCurdy D, Miettunen PM, Quintero-del Rio AI, Rothman D, Rullo O, Ruth N, Schanberg LE, Silverman E, Singer NG, Soep J, Syed R, Vogler LB, Yalcindag A, Yildirim-Toruner C, Wallace CA, Brunner HI, Carra SLE Subcommittee (2012) Consensus treatment plans for induction therapy of newly diagnosed proliferative lupus nephritis in juvenile systemic lupus erythematosus. Arthritis Care Res 64:375–383
Tanaka H, Joh K, Imaizumi T (2017) Treatment of pediatric-onset lupus nephritis: a proposal of optimal therapy. Clin Exp Nephrol 21:755–763
Groot N, de Graeff N, Marks SD, Brogan P, Avcin T, Bader-Meunier B, Dolezalova P, Feldman BM, Kone-Paut I, Lahdenne P, McCann L, Ozen S, Pilkington CA, Ravelli A, Royen-Kerkhof AV, Uziel Y, Vastert BJ, Wulffraat NM, Beresford MW, Kamphuis S (2017) European evidence-based recommendations for the diagnosis and treatment of childhood-onset lupus nephritis: the SHARE initiative. Ann Rheum Dis 76:1965–1973
Fanouriakis A, Kostopoulou M, Alunno A, Aringer M, Bajema I, Boletis JN, Cervera R, Doria A, Gordon C, Govoni M, Houssiau F, Jayne D, Kouloumas M, Kuhn A, Larsen JL, Lerstrom K, Moroni G, Mosca M, Schneider M, Smolen JS, Svenungsson E, Tesar V, Tincani A, Troldborg A, van Vollenhoven R, Wenzel J, Bertsias G, Boumpas DT (2019) 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis 78:736–745
Arbeitsgemeinschaft für Pädiatrische Nephrologie (APN) (2007) Treatment recommendations in children and adolescents with lupus nephritis. Monatsschrift Kinderheilkunde 155:1175–1188
Mina R, Brunner HI (2010) Pediatric lupus--are there differences in presentation, genetics, response to therapy, and damage accrual compared with adult lupus? Rheum Dis Clin N Am 36(53–80):vii
Ardoin SP, Schanberg LE (2012) Paediatric rheumatic disease: lessons from SLE: children are not little adults. Nat Rev Rheumatol 8:444–445
Ardoin SP, Daly RP, Merzoug L, Tse K, Ardalan K, Arkin L, Knight A, Rubinstein T, Ruth N, Wenderfer SE, Hersh AO, Childhood Arthritis and Rheumatology Research Alliance and Lupus Foundation of America (2019) Research priorities in childhood-onset lupus: results of a multidisciplinary prioritization exercise. Pediatr Rheumatol Online J 17:32–019
Weening JJ, D’Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, Balow JE, Bruijn JA, Cook T, Ferrario F, Fogo AB, Ginzler EM, Hebert L, Hill G, Hill P, Jennette JC, Kong NC, Lesavre P, Lockshin M, Looi LM, Makino H, Moura LA, Nagata M, International Society of Nephrology Working Group on the Classification of Lupus Nephritis, & Renal Pathology Society Working Group on the Classification of Lupus Nephritis (2004) The classification of glomerulonephritis in systemic lupus erythematosus revisited. Kidney Int 65:521–530
Hochberg MC (1997) Updating the american college of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Levey AS, Coresh J, Bolton K, Culleton B, Harvey KS, Ikizler TA, Johnson CA, Kausz A, Kimmel PL, Kusek J (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
Neuhauser H, Schienkiewitz A, Rosario AS, Dortschy R, & Kurth B (2013) Referenzperzentile für anthropometrische maßzahlen und blutdruck aus der studie zur gesundheit von kindern und jugendlichen in deutschland (KiGGS)
Kromeyer-Hauschild K, Wabitsch M, Kunze D, Geller F, Geiß H, Hesse V, von Hippel A, Jaeger U, Johnsen D, Korte W, Menner K, Mueller G, Mueller J, Niemann-Pilatus A, Remer T, Schaefer F, Wittchen H, Zabransky S, Zellner K, Ziegler A, & Hebebrand J Perzentile für den body-mass-index für das kindes- und jugendalter unter heranziehung verschiedener deutscher stichproben
Prader A, Largo RH, Molinari L, Issler C (1989) Physical growth of swiss children from birth to 20 years of age. First Zurich longitudinal study of growth and development. Helv Paediatr Acta Suppl 52:1–125
Grote FK, Oostdijk W, De Muinck Keizer-Schrama SM, van Dommelen P, van Buuren S, Dekker FW, Ketel AG, Moll HA, Wit JM (2008) The diagnostic work up of growth failure in secondary health care; an evaluation of consensus guidelines. BMC Pediatr 8:21–2431
Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH, Austin A, Bell A, Bloch DA, Corey PN, Decker JL (1992) Derivation of the SLEDAI. Of J Am Col Rheumatol 35:630–640
Ginzler EM, Bollet AJ, Friedman EA (1980) The natural history and response to therapy of lupus nephritis. Annu Rev Med 31:463–487
Costenbader KH, Desai A, Alarcon GS, Hiraki LT, Shaykevich T, Brookhart MA, Massarotti E, Lu B, Solomon DH, Winkelmayer WC (2011) Trends in the incidence, demographics, and outcomes of end-stage renal disease due to lupus nephritis in the US from 1995 to 2006. Arthritis Rheum 63:1681–1688
Appel GB, Contreras G, Dooley MA, Ginzler EM, Isenberg D, Jayne D, Li LS, Mysler E, Sanchez-Guerrero J, Solomons N, Wofsy D, Aspreva Lupus Management Study Group (2009) Mycophenolate mofetil versus cyclophosphamide for induction treatment of lupus nephritis. J Am Soc Nephrol 20:1103–1112
Houssiau FA, Vasconcelos C, D'Cruz D, Sebastiani GD, Garrido ER, Danieli MG, Abramovicz D, Blockmans D, Mathieu A, Direskeneli H (2002) Immunosuppressive therapy in lupus nephritis: the Euro-Lupus Nephritis Trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum 46:2121–2131
Rovin BH, Furie R, Latinis K, Looney RJ, Fervenza FC, Sanchez-Guerrero J, Maciuca R, Zhang D, Garg JP, Brunetta P, Appel G, LUNAR Investigator Group (2012) Efficacy and safety of rituximab in patients with active proliferative lupus nephritis: the lupus nephritis assessment with rituximab study. Arthritis Rheum 64:1215–1226
Wu JY, Yeh KW, Huang JL (2014) Early predictors of outcomes in pediatric lupus nephritis: focus on proliferative lesions. Semin Arthritis Rheum 43:513–520
Rianthavorn P, Buddhasri A (2015) Long-term renal outcomes of childhood-onset global and segmental diffuse proliferative lupus nephritis. Pediatr Nephrol 30:1969–1976
Lau KK, Ault BH, Jones DP, Butani L (2008) Induction therapy for pediatric focal proliferative lupus nephritis: cyclophosphamide versus mycophenolate mofetil. J Pediatr Health Care 22:282–288
Smith E, Al-Abadi E, Armon K, Bailey K, Ciurtin C, Davidson J, Gardner-Medwin J, Haslam K, Hawley D, Leahy A, Leone V, McErlane F, Mewar D, Modgil G, Moots R, Pilkington C, Ramanan A, Rangaraj S, Riley P, Sridhar A, Wilkinson N, Beresford MW, Hedrich CM (2019) Outcomes following mycophenolate mofetil versus cyclophosphamide induction treatment for proliferative juvenile-onset lupus nephritis. Lupus 28:613–620
Aragon E, Chan YH, Ng KH, Lau YW, Tan PH, Yap HK (2010) Good outcomes with mycophenolate-cyclosporine-based induction protocol in children with severe proliferative lupus nephritis. Lupus 19:965–973
Hogan J, Godron A, Baudouin V, Kwon T, Harambat J, Deschenes G, Niel O (2018) Combination therapy of rituximab and mycophenolate mofetil in childhood lupus nephritis. Pediatr Nephrol 33:111–116
Chan TM, Li FK, Tang CS, Wong RW, Fang GX, Ji YL, Lau CS, Wong AK, Tong MK, Chan KW, Lai KN (2000) Efficacy of mycophenolate mofetil in patients with diffuse proliferative lupus nephritis. Hong Kong-Guangzhou nephrology study group. N Engl J Med 343:1156–1162
Rygg M, Pistorio A, Ravelli A, Maghnie M, Di Iorgi N, Bader-Meunier B, Da Silva C, Roldan-Molina R, Barash J, Dracou C, Laloum SG, Jarosova K, Deslandre CJ, Kone-Paut I, Garofalo F, Press J, Sengler C, Tauber T, Martini A, Ruperto N, Paediatric Rheumatology International Trials Organisation (PRINTO) (2012) A longitudinal PRINTO study on growth and puberty in juvenile systemic lupus erythematosus. Ann Rheum Dis 71:511–517
Hiraki LT, Hamilton J, Silverman ED (2007) Measuring permanent damage in pediatric systemic lupus erythematosus. Lupus 16:657–662
Gutierrez-Suarez R, Ruperto N, Gastaldi R, Pistorio A, Felici E, Burgos-Vargas R, Martini A, Ravelli A (2006) A proposal for a pediatric version of the systemic lupus international collaborating clinics/american college of rheumatology damage index based on the analysis of 1,015 patients with juvenile-onset systemic lupus erythematosus. Arthritis Rheum 54:2989–2996
Marshall WA, Tanner JM (1970) Variations in the pattern of pubertal changes in boys. Arch Dis Child 45:13–23
Olney RC (2009) Mechanisms of impaired growth: effect of steroids on bone and cartilage. Horm Res 72(Suppl 1):30–35
Jux C, Leiber K, Hugel U, Blum W, Ohlsson C, Klaus G, Mehls O (1998) Dexamethasone impairs growth hormone (GH)-stimulated growth by suppression of local insulin-like growth factor (IGF)-I production and expression of GH- and IGF-I-receptor in cultured rat chondrocytes. Endocrinology 139:3296–3305
Ribeiro D, Zawadynski S, Pittet LF, Chevalley T, Girardin E, Parvex P (2015) Effect of glucocorticoids on growth and bone mineral density in children with nephrotic syndrome. Eur J Pediatr 174:911–917
Ruggenenti P, Ruggiero B, Cravedi P, Vivarelli M, Massella L, Marasa M, Chianca A, Rubis N, Ene-Iordache B, Rudnicki M, Pollastro RM, Capasso G, Pisani A, Pennesi M, Emma F, Remuzzi G, Rituximab in Nephrotic Syndrome of Steroid-Dependent or Frequently Relapsing Minimal Change Disease Or Focal Segmental Glomerulosclerosis (NEMO) Study Group (2014) Rituximab in steroid-dependent or frequently relapsing idiopathic nephrotic syndrome. J Am Soc Nephrol 25:850–863
Hocker B, Weber LT, John U, Drube J, Fehrenbach H, Klaus G, Pohl M, Seeman T, Fichtner A, Wuhl E, Tonshoff B (2019) Steroid withdrawal improves blood pressure control and nocturnal dipping in pediatric renal transplant recipients: analysis of a prospective, randomized, controlled trial. Pediatr Nephrol 34:341–348
Acknowledgments
We thank the colleagues of the participating centers and the study nurses from Hannover Medical School for data collection and registry support.
Funding
This study was supported by a grant of €5,000 by the German Society of Paediatric Nephrology. This had no influence on analysis content.
Author information
Authors and Affiliations
Consortia
Contributions
D.H. and I.H. designed the study; A.S. structured the database and analyzed the data. A.S., I.H., and D.H. drafted and revised the paper; all other authors recruited patients to this registry and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Written informed consent was obtained from all parents/guardians to participate in the registry, with assent from patients when appropriate for their age. The study complies with the declaration of Helsinki and was approved by the ethics committee of the Medical University of Rostock, Germany.
Disclaimer
The results in this article have not been published previously in whole or in part, except in abstract form.
Conflict of interest
D.H. has received research grants from Sandoz, Kyowa Kirin, Horizon, and Amgen and has received speaker and/or consultant fees from Amgen, Sandoz, Kyowa Kirn, Pfizer, Merck Serono, Horizon, and Chiesi. All the other authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Nephrology
Rights and permissions
About this article
Cite this article
Suhlrie, A., Hennies, I., Gellermann, J. et al. Twelve-month outcome in juvenile proliferative lupus nephritis: results of the German registry study. Pediatr Nephrol 35, 1235–1246 (2020). https://doi.org/10.1007/s00467-020-04501-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04501-x