Abstract
Objectives
To delineate urine biomarkers that reflect kidney structural damage and predict renal functional decline in pediatric lupus nephritis (LN).
Methods
In this prospective study, we evaluated kidney biopsies and urine samples of 89 patients with pediatric LN. Urinary levels of 10 biomarkers [adiponectin, ceruloplasmin, kidney injury molecule-1, monocyte chemotactic protein-1, neutrophil gelatinase-associated lipocalin, osteopontin, transforming growth factor-ß (TGFß), vitamin-D binding protein, liver fatty acid binding protein (LFABP), and transferrin] were measured. Regression analysis was used to identify individual and combinations of biomarkers that determine LN damage status [NIH-chronicity index (NIH-CI) score ≤ 1 vs. ≥ 2] both individually and in combination, and biomarker levels were compared for patients with vs. without renal functional decline, i.e., a 20% reduction of the glomerular filtration rate (GFR) within 12 months of a kidney biopsy.
Results
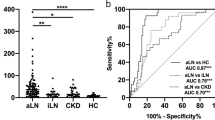
Adiponectin, LFABP, and osteopontin levels differed significantly with select histological damage features considered in the NIH-CI. The GFR was associated with NIH-CI scores [Pearson correlation coefficient (r) = − 0.49; p < 0.0001] but not proteinuria (r = 0.20; p > 0.05). Similar to the GFR [area under the ROC curve (AUC) = 0.72; p < 0.01], combinations of osteopontin and adiponectin levels showed moderate accuracy [AUC = 0.75; p = 0.003] in discriminating patients by LN damage status. Renal functional decline occurred more commonly with continuously higher levels of the biomarkers, especially of TGFß, transferrin, and LFABP.
Conclusion
In combination, urinary levels of adiponectin and osteopontin predict chronic LN damage with similar accuracy as the GFR. Ongoing LN activity as reflected by high levels of LN activity biomarkers heralds renal functional decline.
Key messages
• Levels of osteopontin and adiponectin measured at the time of kidney biopsy are good predictors of histological damage with lupus nephritis.
• Only about 20% of children with substantial kidney damage from lupus nephritis will have an abnormally low urine creatinine clearance.
• Continuously high levels of biomarkers reflecting lupus nephritis activity are risk factors of declining renal function.


Similar content being viewed by others
References
Maroz N, Segal MS (2013) Lupus nephritis and end-stage kidney disease. Am J Med Sci 346:319–323
Sexton DJ, Reule S, Solid C, Chen SC, Collins AJ, Foley RN (2015) ESRD from lupus nephritis in the United States, 1995-2010. Clin J Am Soc Nephrol 10:251–259
Livingston B, Bonner A, Pope J (2012) Differences in autoantibody profiles and disease activity and damage scores between childhood- and adult-onset systemic lupus erythematosus: a meta-analysis. Semin Arthritis Rheum 42:271–280
Mina R, Brunner HI (2013) Update on differences between childhood-onset and adult-onset systemic lupus erythematosus. Arthritis Res Ther 15:218
Hanaoka H, Yamada H, Kiyokawa T, Iida H, Suzuki T, Yamasaki Y, Ooka S, Nagafuchi H, Okazaki T, Ichikawa D, Shirai S, Shibagaki Y, Koike J, Ozaki S (2017) Lack of partial renal response by 12 weeks after induction therapy predicts poor renal response and systemic damage accrual in lupus nephritis class III or IV. Arthritis Res Ther 19:4
Esdaile JM, Levinton C, Federgreen W, Hayslett JP, Kashgarian M (1989) The clinical and renal biopsy predictors of long-term outcome in lupus nephritis: a study of 87 patients and review of the literature. Q J Med 72:779–833
Dall’Era M, Cisternas MG, Smilek DE, Straub L, Houssiau FA, Cervera R, Rovin BH, Mackay M (2015) Predictors of long-term renal outcome in lupus nephritis trials: lessons learned from the euro-lupus nephritis cohort. Arthritis Rheumatol 67:1305–1313
Bennett M, Brunner HI (2013) Biomarkers and updates on pediatrics lupus nephritis. Rheum Dis Clin N Am 39:833–853
Weening JJ, D’Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, Balow JE, Bruijn JA, Cook T, Ferrario F, Fogo AB, Ginzler EM, Hebert L, Hill G, Hill P, Jennette JC, Kong NC, Lesavre P, Lockshin M, Looi LM, Makino H, Moura LA, Nagata M (2004) The classification of glomerulonephritis in systemic lupus erythematosus revisited. J Am Soc Nephrol 15:241–250
Weening JJ, D’Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, Balow JE, Bruijn JA, Cook T, Ferrario F, Fogo AB, Ginzler EM, Hebert L, Hill G, Hill P, Jennette JC, Kong NC, Lesavre P, Lockshin M, Looi LM, Makino H, Moura LA, Nagata M, International Society of Nephrology Working Group on the Classification of Lupus N, Renal Pathology Society Working Group on the Classification of Lupus N (2004) The classification of glomerulonephritis in systemic lupus erythematosus revisited. Kidney Int 65:521–530
Austin HA 3rd, Muenz LR, Joyce KM, Antonovych TT, Balow JE (1984) Diffuse proliferative lupus nephritis: identification of specific pathologic features affecting renal outcome. Kidney Int 25:689–695
Brunner HI, Bennett MR, Mina R, Suzuki M, Petri M, Kiani AN, Pendl J, Witte D, Ying J, Rovin BH, Devarajan P (2012) Association of noninvasively measured renal protein biomarkers with histologic features of lupus nephritis. Arthritis Rheum 64:2687–2697
Brunner HI, Bennett MR, Abulaban K, Klein-Gitelman MS, O’Neil KM, Tucker L, Ardoin SP, Rouster-Stevens KA, Onel KB, Singer NG, Anne Eberhard B, Jung LK, Imundo L, Wright TB, Witte D, Rovin BH, Ying J, Devarajan P (2016) Development of a novel renal activity index of lupus nephritis in children and young adults. Arthritis Care Res 68:1003–1011
Brunner HI, Bennett MR, Gulati G, Abulaban K, Klein-Gitelman MS, Ardoin SP, Tucker LB, Rouster-Stevens KA, Witte D, Ying J, Devarajan P (2017) Urine biomarkers to predict response to lupus nephritis therapy in children and young adults. J Rheumatol 44:1239–1248
Gulati G, Bennett MR, Abulaban K, Song H, Zhang X, Ma Q, Brodsky SV, Nadasdy T, Haffner C, Wiley K, Ardoin SP, Devarajan P, Ying J, Rovin BH, Brunner HI (2017) Prospective validation of a novel renal activity index of lupus nephritis. Lupus 26:927–936
Rovin BH, Song H, Hebert LA, Nadasdy T, Nadasdy G, Birmingham DJ, Yung Yu C, Nagaraja HN (2005) Plasma, urine, and renal expression of adiponectin in human systemic lupus erythematosus. Kidney Int 68:1825–1833
Saraheimo M, Forsblom C, Thorn L, Waden J, Rosengard-Barlund M, Heikkila O, Hietala K, Gordin D, Frystyk J, Flyvbjerg A, Groop PH, FinnDiane Study G (2008) Serum adiponectin and progression of diabetic nephropathy in patients with type 1 diabetes. Diabetes Care 31:1165–1169
Jerebtsova M, Saraf SL, Lin X, Lee G, Adjei EA, Kumari N, Afangbedji N, Raslan R, McLean C, Gordeuk VR (2018) Identification of ceruloplasmin as a biomarker of chronic kidney disease in urine of sickle cell disease patients by proteomic analysis. Am J Hematol 93:E45–E47
Nielsen S, Schjoedt K, Astrup A, Tarnow L, Lajer M, Hansen P, Parving HH, Rossing P (2010) Neutrophil gelatinase-associated lipocalin (NGAL) and kidney injury molecule 1 (KIM1) in patients with diabetic nephropathy: a cross-sectional study and the effects of lisinopril. Diabet Med 27:1144–1150
Abulaban KM, Song H, Zhang X, Kimmel PL, Kusek JW, Nelson RG, Feldman HI, Vasan RS, Ying J, Mauer M, Nelsestuen GL, Bennett M, Brunner HI, Rovin BH (2016) Predicting decline of kidney function in lupus nephritis using urine biomarkers. Lupus 25:1012–1018
Chan RWY, Lai FMM, Li EKM, Tam LS, Wong TYH, Szeto CYK, Li PKT, Szeto CC (2004) Expression of chemokine and fibrosing factor messenger RNA in the urinary sediment of patients with lupus nephritis. Arthritis Rheum 50:2882–2890
Yang CC, Hsieh SC, Li KJ, Wu CH, Lu MC, Tsai CY, Yu CL (2012) Urinary neutrophil gelatinase-associated lipocalin is a potential biomarker for renal damage in patients with systemic lupus erythematosus. J Biomed Biotechnol 2012:759313
Morii T, Fujita H, Narita T, Shimotomai T, Fujishima H, Yoshioka N, Imai H, Kakei M, Ito S (2003) Association of monocyte chemoattractant protein-1 with renal tubular damage in diabetic nephropathy. J Diabetes Complicat 17:11–15
Bolignano D, Basile G, Parisi P, Coppolino G, Nicocia G, Buemi M (2009) Increased plasma neutrophil gelatinase-associated lipocalin levels predict mortality in elderly patients with chronic heart failure. Rejuvenation Res 12:7–14
Bolignano D, Donato V, Coppolino G, Campo S, Buemi A, Lacquaniti A, Buemi M (2008) Neutrophil gelatinase–associated lipocalin (NGAL) as a marker of kidney damage. Am J Kidney Dis 52:595–605
D’Amico G (1998) Tubulo-interstitial damage in glomerular diseases: its role in the progression of the renal damage. Nephrol Dial Transplant 13:80–85
Honkanen E, Teppo AM, Tornroth T, Groop PH, Gronhagen-Riska C (1997) Urinary transforming growth factor-beta 1 in membranous glomerulonephritis. Nephrol Dial Transplant 12:2562–2568
Nath KA (1992) Tubulointerstitial changes as a major determinant in the progression of renal damage. Am J Kidney Dis 20:1–17
Mirković K, Doorenbos CR, Dam WA, Heerspink HJL, Slagman MC, Nauta FL, Kramer AB, Gansevoort RT, van den Born J, Navis G (2013) Urinary vitamin D binding protein: a potential novel marker of renal interstitial inflammation and fibrosis. PLoS One 8:e55887
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Silva CA, Avcin T, Brunner HI (2012) Taxonomy for systemic lupus erythematosus with onset before adulthood. Arthrit Care Res 64:1787–1793
Mina R, Abulaban K, Klein-Gitelman MS, Eberhard BA, Ardoin SP, Singer N, Onel K, Tucker L, O’Neil K, Wright T, Brooks E, Rouster-Stevens K, Jung L, Imundo L, Rovin B, Witte D, Ying J, Brunner HI (2016) Validation of the lupus nephritis clinical indices in childhood-onset systemic lupus erythematosus. Arthritis Care Res 68:195–202
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Chaturvedi S, Farmer T, Kapke GF (2009) Assay validation for KIM-1: human urinary renal dysfunction biomarker. Int J Biol Sci 5:128–134
Bennett MR, Ma Q, Ying J, Devarajan P, Brunner H (2017) Effects of age and gender on reference levels of biomarkers comprising the pediatric renal activity index for lupus nephritis (p-RAIL). Pediatr Rheumatol Online J 15:74. https://doi.org/10.1186/s12969-017-0202-0
Fischer JE, Bachmann LM, Jaeschke R (2003) A readers’ guide to the interpretation of diagnostic test properties: clinical example of sepsis. Intensive Care Med 29:1043–1051
Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PM (2003) The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol 56:1129–1135
McGee S (2002) Simplifying likelihood ratios. J Gen Intern Med 17:646–649
Kurata M, Okura T, Irita J, Enomoto D, Nagao T, Jotoku M, Miyoshi K, Higaki J (2010) The relationship between osteopontin and adiponectin in patients with essential hypertension. Clin Exp Hypertens 32:358–363
Sharma K, Ramachandrarao S, Qiu G, Usui HK, Zhu Y, Dunn SR, Ouedraogo R, Hough K, McCue P, Chan L, Falkner B, Goldstein BJ (2008) Adiponectin regulates albuminuria and podocyte function in mice. J Clin Invest 118:1645–1656
Sasaki Y, Yamamoto Y, Miyazaki T, Ito MR, Nose M, Watanabe M (2006) Augmentation of osteopontin expression in renal tubuli is independent of a histopathological type of glomerular lesions in mouse lupus nephritis. Pathol Int 56:135–143
Feldreich T, Carlsson AC, Helmersson-Karlqvist J, Risérus U, Larsson A, Lind L, Ärnlöv J (2017) Urinary osteopontin predicts incident chronic kidney disease, while plasma osteopontin predicts cardiovascular death in elderly men. Cardiorenal Med 7:245–254
Quaglia M, Chiocchetti A, Cena T, Musetti C, Monti S, Clemente N, Dianzani U, Magnani C, Stratta P (2014) Osteopontin circulating levels correlate with renal involvement in systemic lupus erythematosus and are lower in ACE inhibitor-treated patients. Clin Rheumatol 33:1263–1271
Brunner HI, Silverman ED, To T, Bombardier C, Feldman BM (2002) Risk factors for damage in childhood-onset systemic lupus erythematosus: cumulative disease activity and medication use predict disease damage. Arthritis Rheum 46:436–444
Birmingham DJ, Rovin BH, Shidham G, Bissell M, Nagaraja HN, Hebert LA (2008) Relationship between albuminuria and total proteinuria in systemic lupus erythematosus nephritis: diagnostic and therapeutic implications. Clin J Am Soc Nephrol 3:1028–1033
Fassett RG, Venuthurupalli SK, Gobe GC, Coombes JS, Cooper MA, Hoy WE (2011) Biomarkers in chronic kidney disease: a review. Kidney Int 80:806–821
Benito S, Sanchez-Ortega A, Unceta N, Jansen JJ, Postma G, Andrade F, Aldamiz-Echevarria L, Buydens LMC, Goicolea MA, Barrio RJ (2018) Plasma biomarker discovery for early chronic kidney disease diagnosis based on chemometric approaches using LC-QTOF targeted metabolomics data. J Pharm Biomed Anal 149:46–56
Lv W, Fan F, Wang Y, Gonzalez-Fernandez E, Wang C, Yang L, Booz GW, Roman RJ (2018) Therapeutic potential of microRNAs for the treatment of renal fibrosis and CKD. Physiol Genomics 50:20–34
Donnola SB, Piccone CM, Lu L, Batesole J, Little J, Dell KM, Flask CA (2018) Diffusion tensor imaging MRI of sickle cell kidney disease: initial results and comparison with iron deposition. NMR Biomed. https://doi.org/10.1002/nbm.3883
Birmingham DJ, Rovin BH, Shidham G, Nagaraja HN, Zou X, Bissell M, Yu C-Y, Hebert LA (2007) Spot urine protein/creatinine ratios are unreliable estimates of 24 h proteinuria in most systemic lupus erythematosus nephritis flares. Kidney Int 72:865–870
Aragon E, Resontoc L, Chan Y, Lau Y, Tan P, Loh H, Ng K, Yap H (2016) Long-term outcomes with multi-targeted immunosuppressive protocol in children with severe proliferative lupus nephritis. Lupus 25:399–406
Sato V, Marques I, Goldenstein P, Carmo L, Jorge L, Titan S, Barros R, Woronik V (2012) Lupus nephritis is more severe in children and adolescents than in older adults. Lupus 21:978–983
Malvar A, Pirruccio P, Alberton V, Lococo B, Recalde C, Fazini B, Nagaraja H, Indrakanti D, Rovin BH (2017) Histologic versus clinical remission in proliferative lupus nephritis. Nephrol Dial Transplant 32:1338–1344
Wenderfer SE, Lane JC, Shatat IF, von Scheven E, Ruth NM (2015) Practice patterns and approach to kidney biopsy in lupus: a collaboration of the Midwest pediatric nephrology consortium and the childhood arthritis and rheumatology research alliance. Pediatr Rheumatol Online J 13:26
Acknowledgements
We are indebted to Ms. Kasha Wiley for data management and Lukasz Itert for development of the electronic data entry platform. We acknowledge sample management support by Dr. Fahad Abu-Azzah, Mr. Allen Watts, Ms. Jamie Meyers-Eaton, Ms. Monica Tsoras, and Ms. Mackenzie Gauck at the Cincinnati Children’s Hospital Medical Center. A special thanks to Prof. Susan Thompson for the support of the Rheumatology Research Core Center (1 P30 AR070549). We thank Christopher Haffner and Qing Ma for the measurement of various urine biomarkers.
Funding
This study is supported by grants from the NIH (U01 AR059509 to HB, P50 DK096418 to PD and HB, P30 AR070549-01 to Susan Thompson) and the Innovation Fund from CCHMC; the CCTST at the University of Cincinnati is funded by the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program, grant 5UL1TR001425-03. The CTSA program is led by the NIH’s National Center for Advancing Translational Sciences (NCATS). The content of this website is solely the responsibility of the CCTST and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study complied with the Declaration of Helsinki and was approved by the institutional review boards of all of the participating institutions.
Conflict of interest
The authors declare no conflict of interest.
Statement of informed consent
Written informed consent was obtained from the parents of the children at each institution.
Electronic supplementary material
ESM 1
(DOCX 79 kb)
Rights and permissions
About this article
Cite this article
Brunner, H.I., Gulati, G., Klein-Gitelman, M.S. et al. Urine biomarkers of chronic kidney damage and renal functional decline in childhood-onset systemic lupus erythematosus. Pediatr Nephrol 34, 117–128 (2019). https://doi.org/10.1007/s00467-018-4049-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-4049-5