Abstract
Background
Among comorbidities, pulmonary hypoplasia (PH) is known as a significant risk factor for mortality in infants with end-stage kidney disease (ESKD). However, the final outcomes of infants with both ESKD and PH are still not well defined, as the diagnosis modality, and definition of PH severity remain ambiguous.
Methods
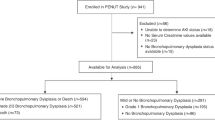
Children initiating peritoneal dialysis during infancy from 1990 to 2015 were followed until death, date of last contact, or the end of 2015. We examined the long-term outcome of children with congenital pulmonary disorders by studying infants with prolonged respiratory disorders of greater than 28 days duration after birth and evaluated risk factors for mortality.
Results
Forty-six children were followed (median follow-up, 9.23 years), and classified as children without (n = 38; Group A) or with (n = 8; Group B) a prolonged respiratory disorder. Overall actuarial 5 year survival rate in this cohort was 79.5 %. The survival curve in Group B showed a significant decline compared with Group A. Prolonged respiratory disorder was significantly associated with mortality by multivariate analysis (hazard ratio, 8.32).
Conclusions
Infants who initiate peritoneal dialysis complicated by prolonged respiratory disorders have increased adverse risk factors for mortality; therefore, withholding aggressive treatment should be considered.




Similar content being viewed by others
References
Bunchman TE (2000) Infant dialysis: the future is now. J Pediatr 136:1–2
Ledermann SE, Scanes ME, Fernando ON, Duffy PG, Madden SJ, Trompeter RS (2000) Long-term outcome of peritoneal dialysis in infants. J Pediatr 136:24–29
McDonald SP, Craig JC, Australian, New Zealand Paediatric Nephrology A (2004) Long-term survival of children with end-stage renal disease. N Engl J Med 350:2654–2662
Ronnholm KA, Holmberg C (2006) Peritoneal dialysis in infants. Pediatr Nephrol 21:751–756
van Stralen KJ, Borzych-Duzalka D, Hataya H, Kennedy SE, Jager KJ, Verrina E, Inward C, Ronnholm K, Vondrak K, Warady BA, Zurowska AM, Schaefer F, Cochat P, registry EE-E, registry I, registry A, Japanese RRTr (2014) Survival and clinical outcomes of children starting renal replacement therapy in the neonatal period. Kidney Int 86:168–174
Rees L (2009) Long-term outcome after renal transplantation in childhood. Pediatr Nephrol 24:475–484
Zurowska AM, Fischbach M, Watson AR, Edefonti A, Stefanidis CJ, European Paediatric Dialysis Working G (2013) Clinical practice recommendations for the care of infants with stage 5 chronic kidney disease (CKD5). Pediatr Nephrol 28:1739–1748
Mitsnefes MM, Laskin BL, Dahhou M, Zhang X, Foster BJ (2013) Mortality risk among children initially treated with dialysis for end-stage kidney disease, 1990–2010. JAMA 309:1921–1929
Alexander RT, Foster BJ, Tonelli MA, Soo A, Nettel-Aguirre A, Hemmelgarn BR, Samuel SM, of the Pediatric Renal Outcomes Group C (2012) Survival and transplantation outcomes of children less than 2 years of age with end-stage renal disease. Pediatr Nephrol 27:1975–1983
Carey WA, Talley LI, Sehring SA, Jaskula JM, Mathias RS (2007) Outcomes of dialysis initiated during the neonatal period for treatment of end-stage renal disease: a North American Pediatric Renal Trials and Collaborative Studies special analysis. Pediatrics 119:e468–473
Vidal E, Edefonti A, Murer L, Gianoglio B, Maringhini S, Pecoraro C, Sorino P, Leozappa G, Lavoratti G, Ratsch IM, Chimenz R, Verrina E, Italian Registry of Paediatric Chronic D (2012) Peritoneal dialysis in infants: the experience of the Italian Registry of Paediatric Chronic Dialysis. Nephrol Dial Transplant 27:388–395
Rheault MN, Rajpal J, Chavers B, Nevins TE (2009) Outcomes of infants <28 days old treated with peritoneal dialysis for end-stage renal disease. Pediatr Nephrol 24:2035–2039
Lantos JD, Warady BA (2013) The evolving ethics of infant dialysis. Pediatr Nephrol 28:1943–1947
Teh JC, Frieling ML, Sienna JL, Geary DF (2011) Attitudes of caregivers to management of end-stage renal disease in infants. Perit Dial Int 31:459–465
Geary DF (1998) Attitudes of pediatric nephrologists to management of end-stage renal disease in infants. J Pediatr 133:154–156
Rees L (2014) The dilemmas surrounding the decision to start chronic dialysis in the neonate. Kidney Int 86:18–20
Shroff R, Ledermann S (2009) Long-term outcome of chronic dialysis in children. Pediatr Nephrol 24:463–474
Shroff R, Rees L, Trompeter R, Hutchinson C, Ledermann S (2006) Long-term outcome of chronic dialysis in children. Pediatr Nephrol 21:257–264
Spiro JE, Konrad M, Rieger-Fackeldey E, Masjosthusmann K, Amler S, Klockenbusch W, Schmitz R (2015) Renal oligo- and anhydramnios: cause, course and outcome-a single-center study. Arch Gynecol Obstet 292:327–336
Cuckow PM, Nyirady P, Winyard PJ (2001) Normal and abnormal development of the urogenital tract. Prenat Diagn 21:908–916
Jackson JC (2012) Respiratory distress in the preterm infant. In: Devaskar CAGU (ed) Avery’s diseases of the newborn, 9th edn. W.B. Saunders, Philadelpia, pp 633–646
Sinkin RA, Cox C, Phelps DL (1990) Predicting risk for bronchopulmonary dysplasia: selection criteria for clinical trials. Pediatrics 86:728–736
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, Wrage LA, Poole K, National Institutes of Child H, Human Development Neonatal Research N (2005) Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics 116:1353–1360
Ishikura K, Uemura O, Ito S, Wada N, Hattori M, Ohashi Y, Hamasaki Y, Tanaka R, Nakanishi K, Kaneko T, Honda M, CKDSG Pediatric, Japan Committee of Measures for Pediatric CKDotJSoPN (2013) Pre-dialysis chronic kidney disease in children: results of a nationwide survey in Japan. Nephrol Dial Transplant 28:2345–2355
Geary C, Whitsett J (2002) Inhaled nitric oxide for oligohydramnios-induced pulmonary hypoplasia: a report of two cases and review of the literature. J Perinatol 22:82–85
Robyr R, Benachi A, Daikha-Dahmane F, Martinovich J, Dumez Y, Ville Y (2005) Correlation between ultrasound and anatomical findings in fetuses with lower urinary tract obstruction in the first half of pregnancy. Ultrasound Obstet Gynecol 25:478–482
Klaassen I, Neuhaus TJ, Mueller-Wiefel DE, Kemper MJ (2007) Antenatal oligohydramnios of renal origin: long-term outcome. Nephrol Dial Transplant 22:432–439
Kemper MJ, Mueller-Wiefel DE (2007) Prognosis of antenatally diagnosed oligohydramnios of renal origin. Eur J Pediatr 166:393–398
Preutthipan A (2015) Home mechanical ventilation in children. Indian J Pediatr 82:852–859
Mekahli D, Shaw V, Ledermann SE, Rees L (2010) Long-term outcome of infants with severe chronic kidney disease. Clin J Am Soc Nephrol 5:10–17
Samuel SM, Tonelli MA, Foster BJ, Alexander RT, Nettel-Aguirre A, Soo A, Hemmelgarn BR, Pediatric Renal Outcomes Canada G (2011) Survival in pediatric dialysis and transplant patients. Clin J Am Soc Nephrol 6:1094–1099
Rees L (2007) Long-term peritoneal dialysis in infants. Perit Dial Int 27[Suppl 2]:S180–184
Shooter M, Watson A (2000) The ethics of withholding and withdrawing dialysis therapy in infants. Pediatr Nephrol 14:347–351
Fauriel I, Moutel G, Moutard ML, Montuclard L, Duchange N, Callies I, Francois I, Cochat P, Herve C (2004) Decisions concerning potentially life-sustaining treatments in paediatric nephrology: a multicentre study in French-speaking countries. Nephrol Dial Transplant 19:1252–1257
Riano I, Malaga S, Callis L, Loris C, Martin-Govantes J, Navarro M, Vallo A (2000) Towards guidelines for dialysis in children with end-stage renal disease. Pediatr Nephrol 15:157–162
Wood EG, Hand M, Briscoe DM, Donaldson LA, Yiu V, Harley FL, Warady BA, Ellis EN, North American Pediatric Renal Transplant Cooperative S (2001) Risk factors for mortality in infants and young children on dialysis. Am J Kidney Dis 37:573–579
Chock VY, Van Meurs KP, Hintz SR, Ehrenkranz RA, Lemons JA, Kendrick DE, Stevenson DK, Network NNR (2009) Inhaled nitric oxide for preterm premature rupture of membranes, oligohydramnios, and pulmonary hypoplasia. Am J Perinatol 26:317–322
de Waal K, Kluckow M (2015) Prolonged rupture of membranes and pulmonary hypoplasia in very preterm infants: pathophysiology and guided treatment. J Pediatr 166:1113–1120
Kumar P, Committee on F, Newborn, American Academy of Pediatrics (2014) Use of inhaled nitric oxide in preterm infants. Pediatrics 133:164–170
Uga N, Ishii T, Kawase Y, Arai H, Tada H (2004) Nitric oxide inhalation therapy in very low-birth weight infants with hypoplastic lung due to oligohydramnios. Pediatr Int 46:10–14
Caesar RE, Packer MG, Kaplan GW, Dudell GG, Guerrant AL, Griswold WR, Lemire JM, Mendoza SA, Reznik VM (1995) Extracorporeal membrane oxygenation in the neonate with congenital renal disease and pulmonary hypoplasia. J Pediatr Surg 30:1560–1563
Acknowledgments
The authors would like to thank Mr. Tetsuji Kaneko (Department of Clinical Research, Tokyo Metropolitan Children’s Medical Center, Tokyo, Japan), Dr. Junya Hashimoto (Department of Nephrology, Tokyo Metropolitan Children’s Medical Center, Tokyo, Japan), Dr. Yoshinobu Nagaoka (Department of Pediatrics, National Hospital Organization, Hokkaido Medical Center), Dr. Hiroyuki Satoh (Department of Urology, Tokyo Metropolitan Children’s Medical Center, Tokyo, Japan) and Dr. Seiichiro Shishido (Department of Pediatric Nephrology, Toho University Faculty of Medicine, Tokyo, Japan) for their contributions to the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declared that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Ethical Committee of Tokyo Metropolitan Children’s Medical Center (approval number: H24-96). For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Sakai, T., Murakami, Y., Okuda, Y. et al. Prolonged respiratory disorder predicts adverse prognosis in infants with end-stage kidney disease. Pediatr Nephrol 31, 2127–2136 (2016). https://doi.org/10.1007/s00467-016-3430-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3430-5