Abstract
Background
Robotic distal pancreatectomy has increasingly been accepted as it has overcome some of the limitations of open distal pancreatectomy, whilst the outcomes following robotic radical antegrade modular pancreatosplenectomy (RAMPS) in patients with pancreatic ductal adenocarcinoma (PDAC) are still uncertain. This study aimed to evaluate the short and long-term outcomes of robotic RAMPS and open RAMPS for PDAC.
Methods
The patients who underwent robotic RAMPS and open RAMPS for PDAC at our clinical centre between January 2017 and December 2021 were reviewed. After a propensity score matching (PSM) at a 1:1 ratio, the perioperative and pathological outcomes in the both groups were reviewed. Univariable and multivariable Cox regression analyses were used to identify independent prognosis factors for overall survival (OS) and recurrence-free survival (RFS) of these patients.
Results
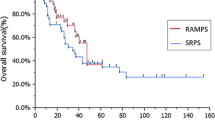
318 cases were recorded in robotic and open groups. The robotic group showed advantages in operative time [205.00 (166.00, 240.00) min vs 235 (184.75, 270.00) min, P = 0.002], estimated blood loss [100 (50, 100) ml vs 300 (100, 400) ml, P < 0.001], delayed gastric emptying [0 vs 5.03%, P = 0.007] and postoperative hospital stay [7.00 (5.00, 10.00) days vs 11.00 (8.00, 14.00) days, P < 0.001]. There were no significant differences in rate of severe postoperative complications between the robotic group and the open group. Multivariable analysis showed that carbohydrate antigen 19-9, estimated blood loss, N stage, tumour differentiation, chemotherapy and vascular invasion were independent risk factors for OS and RFS of these patients.
Conclusions
Robotic RAMPS was safe and had some advantages over open RAMPS for PDAC. There were no significantly differences in oncological outcomes and long-term survival rates between the robotic and open groups. Robotic RAMPS expanded the indications for minimally invasive surgeries for PDAC to a certain extent.



Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RAMPS:
-
Radical antegrade modular pancreatosplenectomy
- PDAC:
-
Pancreatic ductal adenocarcinoma
- PSM:
-
Propensity score matching
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- AJCC:
-
American Joint Committee on Cancer
- S.D:
-
Standard deviation
- IQR:
-
Interquartile range
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- CR-POPF:
-
Clinically relevant postoperative fistulas
References
Rooij TD, Hilst JV, Santvoort HV et al (2019) Minimally invasive versus open distal pancreatectomy: a multicenter patient-blinded randomized controlled trial. Ann Surg 269 (1):2–9
Gagner M, Pomp A, Herrera MF (1996) Early experience with laparoscopic resections of islet cell tumors. Surgery 120:1051–1054
Li MY, Liu Q, Zhang T et al (2022) Evaluating the learning curve of robotic radical antegrade modular pancreatosplenectomy: a retrospective cohort study. Int J Sur 101:106612
Weng Y, Jin J, Huo Z et al (2021) Robotic-assisted versus open distal pancreatectomy for benign and low-grade malignant pancreatic tumors: a propensity score-matched study. Surg Endosc 35 (5):2255–2264
Von Elm E, Altman DG, Egger M et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
https://www.researchregistry.com/register-now#home/registrationdetails/63a09f3e6a116f002747dd60/
Ginimol M, Riaz A, Joerg A et al (2021) STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery—ScienceDirect. Int J Surg 96:106165
Liu Q, Zhao GD, Zhao ZM et al (2021) The standardized technique in robotic radical antegrade modular pancreatosplenectomy using the flip-up approach. Langenbeck’s Arch Surg 406 (5):1697–1703
Strasberg SM, Linehan DC, Hawkins WG (2007) Radical antegrade modular pancreatosplenectomy procedure for adenocarcinoma of the body and tail of the pancreas: ability to obtain negative tangential margins. J Am Coll Surg 204:244–249
Knuf KM, Maani CV, Cummings AK (2018) Clinical agreement in the American Society of Anesthesiologists physical status classification. Perioper Med (Lond) 7:14
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240 (2):205–213
Chun YS, Pawlik TM, Vauthey JN (2018) 8th edition of the AJCC Cancer Staging Manual: pancreas and hepatobiliary cancers. Ann Surg Oncol 25 (4):845–847
Brecher ME, Monk T, Goodnough LT (1997) A standardized method for calculating blood loss. Transfusion 37:1070–1074
Bassi C, Marchegiani G, Dervenis C et al (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161:584–591
Wente MN, Veit JA, Bassi C et al (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142 (1):20–25
Wente MN, Bassi C, Dervenis C et al (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142:761–768
Wang M, Li DW, Chen RF et al (2021) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours: a multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol 6 (6):438–447
Berger M, Bellin MD, Kirchner V et al (2020) Laparoscopic-assisted versus open total pancreatectomy and islet autotransplantation: a case-matched study of pediatric patients. J Pediatr Surg 55 (3):558–563
Ielpo B, Caruso R, Duran H et al (2019) Robotic versus standard open pancreatectomy: a propensity score-matched analysis comparison. Updates Surg. 71 (1):137–144
Zhou JJ, Lv Z, Zou H et al (2020) Up-to-date comparison of robotic-assisted versus open distal pancreatectomy: a PRISMA-compliant meta-analysis. Medicine (Baltimore) 99 (23):e20435
Marino MV, Shabat G, Gulotta G et al (2018) From illusion to reality: a brief history of robotic surgery. Surg Innov 25:291–296
Liu R, Liu Q, Zhao ZM et al (2017) Robotic versus laparoscopic distal pancreatectomy: a propensity score-matched study. J Surg Oncol 116 (4):461–469
Kamarajah SK, Sutandi N, Sen G et al (2022) Comparative analysis of open, laparoscopic and robotic distal pancreatic resection: the United Kingdom’s first single-centre experience. J Minim Access Surg 18 (1):77–83
Lytras D, Paraskevas KI, Avgerinos C et al (2007) Therapeutic strategies for the management of delayed gastric emptying after pancreatic resection. Langenbeck’s Arch Surg 392:1–12
Kawaida H, Kono H, Hosomura N et al (2019) Surgical techniques and postoperative management to prevent postoperative pancreatic fistula after pancreatic surgery. World J Gastroenterol 25 (28):3722–3737
Partelli S, Ricci C, Cinelli L et al (2021) Evaluation of cost-effectiveness among open, laparoscopic and robotic distal pancreatectomy: a systematic review and meta-analysis. Am J Surg 222 (3):513–520
Magistri P, Boggi U, Esposito A et al (2021) Robotic vs open distal pancreatectomy: a multi-institutional matched comparison analysis. J Hepatobiliary Pancreat Sci 28 (12):1098–1106
Bergquist JR et al (2016) Carbohydrate antigen 19-9 elevation in anatomically resectable, early stage pancreatic cancer is independently associated with decreased overall survival and an indication for neoadjuvant therapy: a national cancer database study. J Am Coll Surg 223 (1):52–65
Tamagawa H, Aoyama T, Yamamoto N et al (2020) The impact of intraoperative blood loss on the survival of patients with stage II/III pancreatic cancer. In Vivo. https://doi.org/10.21873/invivo.11931
Min SK, You YH, Choi DW et al (2022) Prognosis of pancreatic head cancer with different patterns of lymph node metastasis. J Hepatobiliary Pancreat Sci 29 (9):1004–1013
Durán H, Olivares S, Ielpo B et al (2020) Prognostic value of lymph node status for actual long-term survival in resected pancreatic cancer. Surg Technol Int 28 (37):79–84
Mirkin KA, Hollenbeak CS, Wong J (2017) Greater lymph node retrieval and lymph node ratio impacts survival in resected pancreatic cancer. J Surg Res 220:12–24
Huang L, Jansen L, Balavarca Y et al (2021) Significance of examined lymph node number in accurate staging and long-term survival in resected stage I-II pancreatic cancer—more is better? A large international population-based cohort study. Ann Surg 274 (6):e554–e563
Yonemura K, Kajiwara Y, Ao T, Mochizuki S, Shinto E, Okamoto K, Hase K, Ueno H (2019) Prognostic value of poorly differentiated clusters in liver metastatic lesions of colorectal carcinoma. Am J Surg Pathol 43:1341–1348
Altman AM, Wirth K, Marmor S et al (2019) Completion of adjuvant chemotherapy after upfront surgical resection for pancreatic cancer is uncommon yet associated with improved survival. Ann Surg Oncol 26 (12):4108–4116
Kasahara N, Noda H, Kakizawa N et al (2019) A lack of postoperative complications after pancreatectomy contributes to the long-term survival of patients with pancreatic cancer. Pancreatology 19 (5):686–694. https://doi.org/10.1016/j.pan.2019.06.012
Fukami Y, Kaneoka Y et al (2016) Prognostic impact of splenic artery invasion for pancreatic cancer of the body and tail. Int J Surg 35:64–68. https://doi.org/10.1016/j.ijsu.2016.09.076
Vicente E, Núñez-Alfonsel J, Ielpo B et al (2020) A cost-effectiveness analysis of robotic versus laparoscopic distal pancreatectomy. Int J Med Robot 16 (2):e2080
Acknowledgements
This study was not supported by any funding.
Author information
Authors and Affiliations
Contributions
Conception and design: RL, YS, WZ, YG; Provision of study materials or patients: ZZ, ZY, CX; Collection and assembly of data: YS, WZ, YG, QL; Data analysis and interpretation: YS, WZ, QL; Manuscript writing: YS, WZ, YG; Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Disclosures
Yuyao Song, Wenbo Zou, Yuanxing Gao, Zhiming Zhao, Zhuzeng Yin, Chaohui Xiao, Qu Liu and Rong Liu have no conflicts of interest or financial ties to disclose.
Consent to participate
Written informed consent was obtained from all patients.
Ethical approval
This study was approved by the Institutional Review Board at the First Medical Center, Chinese People’s Liberation Army General Hospital (S2020-252-14).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Song, Y., Zou, W., Gao, Y. et al. Short- and long-term outcomes of robotic versus open radical antegrade modular pancreatosplenectomy: a retrospective propensity score-matched cohort study. Surg Endosc 38, 1316–1328 (2024). https://doi.org/10.1007/s00464-023-10635-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10635-4