Abstract
Background
In recent years, the number of minimally invasive pancreatoduodenectomy (MIPD) has been increasing; however, the procedure has not been widely accepted due to its complexity and difficulty. We have developed a technique to mobilize the pancreas head using a left-sided approach with a focus on the complete dissection of the Treitz ligament.
Methods
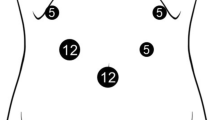
This technique focuses on the secure mobilization of the pancreas head using a left-sided approach. First, the transverse mesocolon is flipped upward and the anterior side of the mesojejunum is excised to expose the first jejunal artery (1st JA) from the distal side to its origin. During the procedure, the left sides of the SMA and Treitz ligament are exposed. The Treitz ligament is retracted to the left side and dissected anteriorly. Thereafter, the jejunum is flipped to the right side and the retroperitoneum around the origin of the jejunum and duodenum is dissected to identify the inferior vena cava (IVC). The rest of the Treitz ligament is dissected posteriorly and complete resection of the Treitz ligament releases the limitation of duodenal immobility. Thereafter, dissection proceeds along the anterior wall of the IVC, and mobilization of the pancreas head is completed from the left side.
Results
A total of 75 consecutive patients underwent MIPD from April 2016 to July 2022. The median operation times of laparoscopic and robotic procedures were 528 min (356–757 min) and 739 min (492–998 min), respectively. The volume of blood loss during laparoscopic and robotic procedures was 415 g (60–4360 g) and 211 g (17–1950 g), respectively. There was no mortality in any of the cases.
Conclusion
Mobilization of the pancreas head and left-sided approach using a caudal view will be a safe and useful technique for MIPD.




Similar content being viewed by others
References
Palanivelu C, Senthilnathan P, Sabnis SC, Babu NS, Srivatsan Gurumurthy S, Anand Vijai N, Nalankilli VP, Praveen Raj P, Parthasarathy R, Rajapandian S (2017) Randomized clinical trial of laparoscopic versus open pancreatoduodenectomy for periampullary tumours. Br J Surg 104(11):1443–1450
Poves I, Burdio F, Morato O, Iglesias M, Radosevic A, Ilzarbe L, Visa L, Grande L (2018) Comparison of perioperative outcomes between laparoscopic and open approach for pancreatoduodenectomy: the PADULAP Randomized Controlled Trial. Ann Surg 268(5):731–739
Wang M, Li D, Chen R, Huang X, Li J, Liu Y, Liu J, Cheng W, Chen X, Zhao W, Li J, Tan Z, Huang H, Li D, Zhu F, Qin T, Ma J, Yu G, Zhou B, Zheng S, Tang Y, Han W, Meng L, Ke J, Feng F, Chen B, Yin X, Chen W, Ma H, Xu J, Liu Y, Lin R, Dong Y, Yu Y, Liu J, Zhang H, Qin R (2021) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours: a multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol 6(6):438–447
Nickel F, Haney CM, Kowalewski KF, Probst P, Limen EF, Kalkum E, Diener MK, Strobel O, Muller-Stich BP, Hackert T (2020) Laparoscopic versus open pancreaticoduodenectomy: a systematic review and meta-analysis of randomized controlled trials. Ann Surg 271(1):54–66
Liu Q, Zhao Z, Zhang X, Wang W, Han B, Chen X, Tan X, Xu S, Zhao G, Gao Y, Gan Q, Yuan J, Ma Y, Dong Y, Liu Z, Wang H, Fan F, Liu J, Lau WY, Liu R (2021) Perioperative and oncological outcomes of robotic versus open pancreaticoduodenectomy in low-risk surgical candidates: a multicenter propensity score-matched study. Ann Surg. https://doi.org/10.1097/SLA.0000000000005160
Shiroshita H, Inomata M, Akira S, Kanayama H, Yamaguchi S, Eguchi S, Wada N, Kurokawa Y, Uchida H, Seki Y, Ieiri S, Iwazaki M, Sato Y, Kitamura K, Tabata M, Mimata H, Takahashi H, Uemura T, Akagi T, Taniguchi F, Miyajima A, Hashizume M, Matsumoto S, Kitano S, Watanabe M, Sakai Y (2022) Current status of endoscopic surgery in Japan: the 15th National Survey of Endoscopic Surgery by the Japan Society for Endoscopic Surgery. Asian J Endosc Surg. https://doi.org/10.1111/ases.13012
Honda G, Kurata M, Okuda Y, Kobayashi S, Sakamoto K, Takahashi K (2013) Laparoscopic pancreaticoduodenectomy: taking advantage of the unique view from the caudal side. J Am Coll Surg 217(6):e45–e49
Cho A, Yamamoto H, Kainuma O (2014) Tips of laparoscopic pancreaticoduodenectomy: superior mesenteric artery first approach (with video). J Hepatobiliary Pancreat Sci 21(3):E19–E21
Nagakawa Y, Watanabe Y, Kozono S, Boggi U, Palanivelu C, Liu R, Wang S, He J, Nishino H, Ohtsuka T, Ban D, Nakata K, Endo I, Tsuchida A, Nakamura M (2022) Surgical approaches to the superior mesenteric artery during minimally invasive pancreaticoduodenectomy: a systematic review. J Hepatobiliary Pancreat Sci 29(1):114–123
Nassar S, Menias CO, Palmquist S, Nada A, Pickhardt PJ, Shaaban AM, Gaballah AH, Elsayes KM (2021) Ligament of treitz: anatomy, relevance of radiologic findings, and radiologic-pathologic correlation. Am J Roentgenol 216(4):927–934
Nagakawa Y, Nakata K, Nishino H, Ohtsuka T, Ban D, Asbun HJ, Boggi U, He J, Kendrick ML, Palanivelu C, Liu R, Wang S, Tang C-N, Takaori K, Hilal MA, Goh BKP, Honda G, Jang J-Y, Kang CM, Kooby DA, Nakamura Y, Shrikhande SV, Wolfgang CL, Yiengpruksawan A, Yoon Y-S, Watanabe Y, Kozono S, Ciria R, Berardi G, Garbarino GM, Higuchi R, Ikenaga N, Ishikawa Y, Maekawa A, Murase Y, Zimmitti G, Kunzler F, Wang Z-Z, Sakuma L, Takishita C, Osakabe H, Endo I, Tanaka M, Yamaue H, Tanabe M, Wakabayashi G, Tsuchida A, Nakamura M (2022) International expert consensus on precision anatomy for minimally invasive pancreatoduodenectomy: PAM-HBP surgery project. J Hepatobiliary Pancreat Sci 29(1):124–135
Inoue Y, Sato T, Kato T, Oba A, Ono Y, Ito H, Makuuchi R, Takahashi Y (2022) How can we optimize surgical view during robotic-assisted pancreaticoduodenectomy? Feasibility of multiple scope transition method. J Am Coll Surg 235(4):e1–e7
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Kohei Nakata, Toshiya Abe, Noboru Ideno, So Nakamura, Naoki Ikenaga, Kinuko Nagayoshi, Yusuke Mizuuchi, Taiki Moriyama, Kenoki Ohuchida, and Masafumi Nakamura have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 117702 KB)
Supplementary file2 (MP4 255001 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nakata, K., Abe, T., Ideno, N. et al. A left-sided approach for wide mobilization of the pancreas with complete dissection of the Treitz ligament (with video). Surg Endosc 37, 4982–4989 (2023). https://doi.org/10.1007/s00464-023-10065-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10065-2