Abstract
Background
The surface morphology of colorectal polyps is well correlated with submucosal invasion in Eastern Countries but not in North America. We aimed to investigate associations between the Paris classification, surface morphology, and Kudo pit pattern to submucosal invasion in advanced endoscopic resection techniques.
Methods
We retrospectively analyzed prospectively collected data of consecutive advanced endoscopic procedures conducted by a single surgeon between August 2017 and October 2018. The data included patients’ demographics, the endoscopic finding of polyps (Paris, Kudo, and surface morphology), and pathology results.
Results
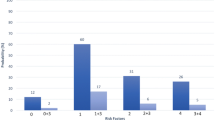
The study consisted of 138 lesions, and the mean age was 67 ± 10 years. The most common polyp locations were cecum (n = 41, 30%) followed by ascending colon (n = 28, 20%), and sigmoid colon (n = 18, 13%).The median polyp size was 30 mm (25–40). The en-bloc resection rate was 96%, and 11 (8%) polyps had adenocarcinoma with submucosal invasion. Nine patients (6.5%) had late bleeding, and 3 (2.2%) perforation occurred. Polyps with pit pattern of Kudo IV (n = 4, 36.4%) and Kudo V (n = 6, 54.5%) were associated with submucosal invasion.
Conclusions
Surface morphology and pit pattern can predict submucosal invasion in the North American patient population. Polyp morphology may aid polyp selection for advanced endoscopic interventions.





Similar content being viewed by others
References
Edwards BK, Noone AM, Mariotto AB, Simard EP, Boscoe FP, Henley SJ, Jemal A, Cho H, Anderson RN, Kohler BA, Eheman CR, Ward EM (2013) (2014) Annual Report to the Nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer 120(9):1290–1314. https://doi.org/10.1002/cncr.28509.Dec16
Lin JS, Piper MA, Perdue LA, Rutter CM, Webber EM, O’Connor E, Smith N, Whitlock EP (2016) (2016) Screening for colorectal cancer: updated evidence report and systematic review for the US preventive services task force. JAMA 315(23):2576–2594. https://doi.org/10.1001/jama.2016.3332
Markowitz AJ, Winawer SJ (1997) Management of colorectal polyps. CA Cancer J Clin 47(2):93–112. https://doi.org/10.3322/canjclin.47.2.93
Kitajima K, Fujimori T, Fujii S, Takeda J, Ohkura Y, Kawamata H, Kumamoto T, Ishiguro S, Kato Y, Shimoda T, Iwashita A, Ajioka Y, Watanabe H, Watanabe T, Muto T, Nagasako K (2004) Correlations between lymph node metastasis and depth of submucosal invasion in submucosal invasive colorectal carcinoma: a Japanese collaborative study. J Gastroenterol 39(6):534–543. https://doi.org/10.1007/s00535-004-1339-4
Terasaki M, Tanaka S, Oka S, Nakadoi K, Takata S, Kanao H, Yoshida S, Chayama K (2012) Clinical outcomes of endoscopic submucosal dissection and endoscopic mucosal resection for laterally spreading tumors larger than 20 mm. J Gastroenterol Hepatol 27(4):734–740. https://doi.org/10.1111/j.1440-1746.2011.06977.x
Holmes I, Friedland S (2016) Endoscopic mucosal resection versus endoscopic submucosal dissection for large polyps: a Western Colonoscopist’s view. Clin Endosc 49(5):454–456. https://doi.org/10.5946/ce.2016.077.Aug26,2016
Kudo S, Tamura S, Nakajima T, Yamano H, Kusaka H, Watanabe H (1996) Diagnosis of colorectal tumorous lesions by magnifying endoscopy. Gastrointest Endosc 44(1):8–14. https://doi.org/10.1016/s0016-5107(96)70222-5
Ikehara H, Saito Y, Matsuda T, Uraoka T, Murakami Y (2010) Diagnosis of depth of invasion for early colorectal cancer using magnifying colonoscopy. J Gastroenterol Hepatol 25(5):905–912. https://doi.org/10.1111/j.1440-1746.2010.06275.x
Mason SE, Poynter L, Takats Z, Darzi A, Kinross JM (2019) Optical technologies for endoscopic real-time histologic assessment of colorectal Polyps: a meta-analysis. Am J Gastroenterol 114(8):1219–1230. https://doi.org/10.14309/ajg.0000000000000156
Tanaka S, Kashida H, Saito Y, Yahagi N, Yamano H, Saito S, Hisabe T, Yao T, Watanabe M, Yoshida M, Saitoh Y, Tsuruta O, Sugihara KI, Igarashi M, Toyonaga T, Ajioka Y, Kusunoki M, Koike K, Fujimoto K, Tajiri H (2020) Japan gastroenterological endoscopy society guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc 32(2):219–239. https://doi.org/10.1111/den.13545
Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, Amato A, Berr F, Bhandari P, Bialek A, Conio M, Haringsma J, Langner C, Meisner S, Messmann H, Morino M, Neuhaus H, Piessevaux H, Rugge M, Saunders BP, Robaszkiewicz M, Seewald S, Kashin S, Dumonceau JM, Hassan C, Deprez PH (2015) Endoscopic submucosal dissection: European society of gastrointestinal endoscopy (ESGE) guideline. Endoscopy 47(9):829–854. https://doi.org/10.1055/s-0034-1392882
Draganov PV, Wang AY, Othman MO, Fukami N (2019) AGA institute clinical practice update: endoscopic submucosal dissection in the United States. Clin Gastroenterol Hepatol 17(1):16-25.e1. https://doi.org/10.1016/j.cgh.2018.07.04
Acknowledgements
None
Funding
This study did not receive any funding/support or financial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Ilker Ozgur: None declared. Ipek Sapci: None declared. Berke Sengun: None declared. Michael A. Valente: None declared. Scott R. Steele: None declared. David Liska: Consultant for Olympus,Conor P. Delaney: None declared. Emre Gorgun: Consultant for Boston Scientific, DiLumen and Olympus.
Ethical approval
The institutional review board approved the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was presented as Quick Shot presentation at Virtual 62nd Annual Meeting of SOCIETY FOR SURGERY OF THE ALIMENTARY TRACT, May 21-23, 2021 in partnership with Digestive Disease Week® 2021.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ozgur, I., Sapci, I., Sengun, B. et al. Do surface morphology and pit pattern have a role in predicting cancer for colon polyps in North America?. Surg Endosc 37, 2354–2358 (2023). https://doi.org/10.1007/s00464-023-09866-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09866-2