Abstract
Background and aims
With the global epidemic of SARS-CoV-2, there has been a growing concern regarding the risk of aerosol exposure to healthcare workers and patients during medical/surgical interventions. The Schlieren device is capable of visualizing fine gas-flows by using refractive index differences in the medium. We aimed to reveal the existence of gas leakage from gastro-intestinal endoscopy system by utilizing Schlieren device and to clarify the factors which relates to the amount of gas leakage.
Methods
The experiments were performed on the excised swine stomach while maintaining a constant pressure environment in the stomach. The System Schlieren (SS100,KatoKoken) was used to visualize possible gas leakages from forceps plugs of endoscopy. We attempted to semi-quantify the leakage by referring to the image of the gas from the forceps plug and by measuring the initial velocity and diffusion area of the leakage.
Results
Regardless of the type of forceps plugs, a certain amount of leakage was detected during both insertion and removal of forceps. The initial velocity and the diffusion area of the leakage increased with the increase in intragastric pressure. Semi-quantitative comparison showed that there was a difference in the amount of gas leakage among various forceps plugs. Furthermore, the amount of gas leakage was significantly greater in the forceps plugs that were used repeatedly.
Conclusion
It was possible to visualize gas leakages from the gastrointestinal endoscope system using the Schlieren optical device. Avoiding too high intragastric pressure and not using deteriorated plugs may reduce the risk of aerosol exposure.
Similar content being viewed by others
With the global spread of SARS-CoV-2 in 2020, there has been increasing interest in the assessment of the risk of viral infection via leaking gas from medical device, as SARS-CoV-2 is believed to be mediated by aerosols, which are finer particle forms than regular droplets [1, 2]. Therefore, visualizing the behavior of aerosols is useful in assessing the risk of viral exposure. As well as patients, health care workers are at high risk for viral infections, and their risk assessment is particularly important. [3] Gastrointestinal (GI) endoscopy has been recognized as a procedure with a very high risk of aerosol exposure because of the inevitable contact with the patient’s oral and airway secretions [4, 5]. To reduce the risk of infection, wearing personal protective equipment (PPE) is recommended during GI endoscopy, but it is difficult to say that PPE is thoroughly applied in clinical practice, and there are reports that even with sufficient PPE, the risk of infection cannot be reduced to zero [3]. In addition to personal protection with PPE, it is extremely important to take this opportunity to reduce exposure to aerosols, i.e., to prevent gas leakage from patients themselves and from medical devices (including endoscopes). Although screening tests for COVID-19 have been conducted on patients and the risk of exposure to the virus via aerosols has been reduced, it is important to evaluate gas leaks from medical devices and develop countermeasures in an attempt to prevent a possible future pandemic of an unknown infectious disease.
Schlieren optical systems are used mainly in engineering fields to visualize minute changes in gas-flow that are invisible to the naked eye, by using differences in the density and refractive index of the medium [6]. This visualization method has the potential to semi-quantitatively analyze the gas leakage from various parts of the endoscopic system, but no systematic studies have been conducted.
Even if there is gas leakage from the endoscopy system, it is not certain whether the gas contains the virus RNA that is the source of infection; as far as SARS-CoV-2 is concerned, it has been reported that the gastric juice contains viral RNA [7]. As long as it has not been proven that there is no risk of infection, countermeasures are necessary, and gas leaks are not desirable in any case, even in the case of unknown infectious diseases other than SARS-CoV-2.
In this study, we aimed to obtain answers to the following questions; Question 1: Can gas leakage from forceps plugs be visualized using the Schlieren device? Question 2: Is gas leakage from the plug associated with internal pressure in the stomach? Question 3: Is gas leakage from the plug related to the type and condition of the plug itself?
Materials and methods
Study settings
Procedures were performed on bench-top simulators containing an explanted swine stomach.
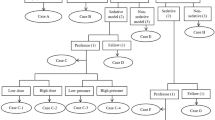
The steady pressure automatically controlled endoscopy (SPACE) system
Steady pressure automatically controlled endoscopy (SPACE) system was constructed according to our previous reports but with several modifications [8,9,10,11]. In order to ensure the reproducibility of the experiments, the intragastric pressure had to be kept constant at an arbitrary pressure, and each experiment was performed under the control of the SPACE system. Briefly, a detachable leak-proof device with an anti-reflux valve and a Luer lock connection (Leak Cutter; Top, Tokyo, Japan) was connected to a standard endoscopic overtube (#16,630; Top). A standard flexible GI endoscope (GIF-Q260J; Olympus Medical Systems; Tokyo, Japan) was advanced into the stomach through the overtube. For CO2 insufflation, a dedicated CO2 insufflator (GW-200; Fujifilm) was connected to the side channel of the Leak Cutter. The intragastric pressure was controlled at 0–15 mmHg via GW-200. The entire observation system is shown in Fig. 1. The performance of the SPACE system has already been verified in a previous report [8].
The experimental setting for visualizing gas leakages by System Schlieren using the SPACE system. A SPACE system: CO2 insufflation system (GW-200, Fujifilm, Tokyo, Japan) was connected to Leak Cutter (Top, Tokyo, Japan) inserted into the esophagus of a swine to create a SPACE environment. B The body of Schlieren optical system (System Schlieren, SS100, Kato Koken, Tokyo, Japan). C The part of the forceps plug to be observed was placed in the area between the achromat lens and the reflector of the Schlieren device
Schlieren optical system
We used a large, sensitive Schlieren optical system (System Schlieren, SS100, Kato Koken, Tokyo, Japan: Fig. 2A) based on a 10 cm diameter parabolic telescope mirror to image the gas-flows from the biopsy plugs of endoscopy. The schlieren system is located in a 10 × 10 × 3.6 m laboratory. Room air-conditioning is turned off while imaging to provide a quiescent ambient atmosphere. The average air temperature during testing is set at 22 °C, the same as in a typical clinical setting in our hospital. High-definition 1024 × 1024-pixel, 200 frame/second video records of gas leakages were captured by a digital SLR camera (Nikon D90, Tokyo, Japan) with 1/40000 shutter speed. Details on the Schlieren system are given in Supplemental Figs. 1 and 2.
System Schlieren -the device to visualize gas leakages—A Appearance of System Schlielen B Visualization of jet stream using System Schlieren Schlieren photography is a technique used to capture gas movement based on differences in fluid density. For example, gas with higher temperature has lower density than the surrounding gas with lower temperature, leading to different values of refractive index. C Optical principle of the System Schlieren (a) Reflection mirror, (b) Acromat lems, (c) Half mirror, (d) Light source, (e) Reflection mirror, (f) Knife edge, (e) Camera Depending on the refractive index, some light is cut off at the knife edge.
The procedure of inserting and removing forceps
In order to minimize variability due to the procedure, the method of insertion and removal of the endoscopic instrument was standardized as follows. The forceps were inserted perpendicularly to the biopsy plug and advanced vertically by 1 cm per second; after 3 cm insertion (i.e., after 3 s), the forceps were held in place for 1 s and then withdrawn vertically by 1 cm per second till complete removal. We marked 3 cm from the tip of the forceps and inserted it for 3 s while having a timekeeper measure the time to get there, making the speed as uniform as possible. The same procedure was repeated five times for all plugs. The method of insertion and removal of the forceps is summarized in Fig. 3.
Visualization of gas leakage from biopsy plug. A Device insertion and removal procedure. (1) Insert the device upright to the entrance hole. (2) Advance the device 1 cm/s keeping upright to the plug. (3) Advance 3mc and pause 1 s. (4) Extract the device 1 cm/s keeping upright to the plug. (5) Remove the device. B. C Sequential photographs of the insertion and removal of instruments taken using a schlieren optical system every 50 ms; B Insertion, C Removal
Image analysis
The methods to analyze the images of gas leakages are shown in Fig. 4. In this study, the following two parameters were used to semi-quantify the gas leakages.
Analyzing methods to quantify gas leakages. A: Initial velocity: The images 50 ms (10frames) after the initial gas leakage emerged was utilized. The distance between the advanced edge of the gas and the entrance of the plug (X) was measured by Image J and the velocity of gas was calculated. The initial velocity was calculated using the following formula; Initial velocity (cm/s) = X (cm)/0.05 (s). B, C Maximum leakage area. B Insertion: Analyze the image when the initial gas reached the edge of the vision (Y). C Removal: Analyze the image when the whole body of the device is removed from the plug (Z). The area of the gas diffused was traced manually and measure the area by Image J
Initial velocity
The images 50 ms (10frames) after the initial gas leakage emerged was utilized to decide the initial velocity (Fig. 4A). The distance between the advanced edge of the leakage gas-flow and the entrance of the plug was measured by Image J (National Institute of Health, Maryland, US), which is an open source, public domain image processing software. The initial velocity of gas leakage was calculated by dividing the distance by the time required (50 ms). The mean and standard deviation of the five measurements were calculated.
Maximum leakage area
The images when the leakage gas-flow reached the edge of the circular vision was utilized to decide the maximum leakage area of insertion (Fig. 4B). On the other hand, the images when the whole body of the device is removed from the plug was utilized to decide the maximum leakage area of removal (Fig. 4C). The area of the leakage gas-flow diffused was traced manually and measure by Image J. The mean and standard deviation of the five measurements were calculated.
Experiment 1
We investigated whether gas leakages can be visualized using a Schlieren device when biopsy forceps are inserted into a reusable plug. Intragastric pressure was maintained at 8 mmHg, close to the normal intragastric pressure during upper GI endoscopy as daily practice reported by Ushimaru et.al [12].
Experiment 2
The changes in gas leakages were studied when the intragastric pressure was varied at 4–15 mmHg using GW-200. Experiments were repeated five times for each intragastric pressure, and the data are presented as mean ± SD.
Experiment 3
The differences in gas leakages among three types of plugs were investigated: (1) reusable, (2) disposable, and (3) universal types. Repeatedly used (deteriorated) reusable plugs were also investigated in the same way. The details of each plug are as follows: reusable type is MB-358 (Olympus, Tokyo, Japan); disposable type is MAJ-1555 (Olympus); universal type is 711124 (US Endoscopy, Ohio, US). Repeatedly used (deteriorated) is a reusable plug after the biopsy forceps has been inserted and removed more than ten times. Through the experiment, standard biopsy forceps were used. Experiments were performed five times for each plug, and the data are presented as mean ± SD.
Statistical analysis
Data were analyzed with JMP14 software (SAS Institute Inc., Cary, NC, USA). Continuous data are reported as the mean ± standard deviation. ANOVA (analysis of variance) was used for group comparisons of continuous data at a single time point. P values < 0.05 were considered significant.
Results
Experiment 1
Gas leakages were observed on the very moment of insertion and removal in every procedure, but no leakages were observed during forceps advancement, at rest, and during extracting (Fig. 3B and C).
Experiment 2
The initial velocity and maximal leak area (mean ± SD) of gas leakage during forceps insertion at 8 mmHg were 67.5 ± 15.3 cm/s and 16.5 ± 3.9 cm2, respectively (Table 1, and Fig. 5). Both initial velocity and maximal leakage area tended to increase with higher intragastric pressure conditions. There was a significant difference between the mean values of initial velocity under each intragastric pressure condition (P = 0.001). As for the gas leakage at the time of forceps removal, both initial velocity and maximal leakage area tended to increase with higher intragastric pressure conditions. There was a significant difference in the mean values (P < 0.0001).
Experiment 3
During both insertion and removal of forceps, both initial velocity and maximal leakage area tended to be large for disposable type and deteriorated reusable type forceps plugs (Table 2 and Fig. 6). On the contrary, both the initial velocity and the maximal leakage area of Universal type forceps plugs were smaller than those of other forceps plugs.
Discussion
Although the SARS-CoV-2 pandemic has prompted a major reevaluation of the risk of infection in healthcare settings, [13] the risk of viral transmission during GI endoscopy has been mainly focused on the secretions from the patient's mouth [14]. It is not clear whether aerosols or body fluids from the oral cavity pose a greater threat of infection, as these were not evaluated in this study. In any case, wearing PPE is central to infection prevention, but past reports indicate that even with perfect PPE it is difficult to reduce the risk of infection to zero [3]. While perfect PPE is of course very important, we believe it is also important to try to limit aerosol leakage from the plug as well as limit the risk of exposure from coughing and other secretions from the patient’s oral cavity (e.g., wearing a patient mask) in order to further minimize the risk.
In the Experiment 1, we firstly succeeded in visualizing gas leakages from the forceps plug of a GI endoscope using Schlieren optical system. Because of the assumption that the GI endoscopy system itself is essentially a “closed” circuit, aerosol exposure control in GI endoscopy has focused only on aerosols from the patient’s mouth. This study showed that there is a risk of aerosol exposure not only from the patient’s oral cavity, but also from forceps plugs. In the previous study, Urakawa et al. proved that there is a gas leakage from the forceps plug by submerging the endoscope in a water tank and recognizing it as an air bubble [15]. In this study, we examined the leakage in more detail. Visualizing gas leakage as a “jet” and semi-quantifying it in an environment similar to actual clinical practice and identifying factors associated with the amount of gas leakage is an achievement not seen in previous reports. The detailed mechanism of gas leakage was not examined in this study. We plan to analyze the mechanism of gas leakage through non-destructive analysis of plugs in the future, and to develop products that can minimize gas leakage.
The results of Experiment 2 showed a correlation between the intragastric pressure and the initial velocity of gas leakages. Physically, the higher the internal pressure, the higher the external force that pushes the gasflow out of the leakage, and thus the higher the flow velocity, which is a reasonable result. This result suggests that one effective way to reduce gas leakages from the forceps opening is to use lower gastric pressure, i.e., avoid unnecessary gas insufflation. On the other hand, the results of Experiment 1 showed that gas leakage from the plug occurred only when the forceps was inserted or withdrawn, and no leakage was observed when the forceps tip was in the stomach and the operation was being performed. Based on the above, we do not necessarily recommend low pressure at all times, but believe that it is acceptable to avoid “unnecessary” insufflation only during forceps insertion and removal, and to insufflate adequately during forceps manipulation.
In Experiment 3, there was a difference in the gas leakage velocity and diffusion area depending on the type of plugs. The initial velocity and leakage area of gas leakages from the reusable and disposable plugs were larger than those of the universal type. The difference in the internal structure of the forceps plug might be largely responsible for the difference in airtightness. In particular, plugs that had been used repeatedly had approximately 1.5 times the amount of leakage compared to plugs before use. In the case of the “exhausted” plug that had been used repeatedly and deteriorated, the distortion of the plug was assumed to be much larger than that of other plugs, and as a result, the gas leakages become more significant. In addition, the valve of the deteriorated reusable plug remained distorted even when the forceps was not inserted, and as a result, persistent gas leakages were observed even when the forceps was not inserted (Supplemental Fig. 3). In terms of infection prevention, excessive reuse of reusable plugs should be avoided.
Does the gas leakage from the GI endoscopy system that we visualized contain any infectious viruses? Miyake et al. reported that asymptomatic patients, even those with no detectable virus in their saliva, had SARS-CoV-2 in their GI tract [7]. On the other hand, Flemming et al. reported that SARS-CoV-2 is detectable in the respiratory system but not in the GI samples [16]. In other words, there is still no consensus on whether gas leakages from GI endoscopy systems carry a latent risk of SARS-CoV-2 infection. However, since there is no proof that the virus does not exist, it is important to assume that it does exist and to take all possible measures to prevent infection. We do not want to emphasize the danger of a gas leak from the plug itself, but rather the danger of performing a procedure without being aware of the presence of a gas leak. It is not clear how much gas leakage from the plug actually poses a risk of infection, but theoretically there is a certain risk for aerosol infection because gas leakage is from the gastrointestinal lumen adjacent to the airway at its most oral side. Furthermore, future unknown pathogen which can be more transmittable from the gastrointestinal fluid and/or mucosa will be in the gas leakage. We believe that one of the most significant aspects of this study is that it visualized gas leaks that carry a risk of infection and raised the need for countermeasures.
Routine testing for SARS-CoV-2 is being performed worldwide for daily screening tests, and the potential infection risk for healthcare workers with respect to SARS-CoV-2 has decreased. However, even with such a recent infection control situation, there are several reasons why gas leaks from plugs should be addressed as a source of infection. First of all, the sensitivity of the screening test itself is not 100% [17]. We should not assume that subjects who pass the screening test are not a source of infection. In addition, there are often situations in clinical practice where there is not enough time to perform the screening test. Life-threatening situations, such as hemostatic emergencies, can be handled quickly without a screening test. In such situations, healthcare workers tend to focus on saving the patient’s life, and the gas leakage may become a secondary concern. In addition, there is no screening test for emerging infectious diseases other than SARS-CoV-2, so it is important to prevent gas leakage from plugs as a “sustainable” infection control measure.
There are several limitations in this study. First of all, all of the experiments in this study were performed under benchtop settings using ex vivo models, and there might be many differences from our daily clinical practice. Clinically, the forceps would contain a tissue sample and be contaminated with patient fluids which may alter the dynamics of gas leakage, the fluid content of the leaked gas. In fact, we have confirmed that gas leakage does occur in actual living organisms (i.e., living swine), but we omitted it from this study because stable and reproducible data cannot be obtained due to the influence of body fluids (data not shown). When we develop a new forceps plug with less gas leakage, we test its feasibility in living bodies or in the clinical setting.
Secondly, Schlieren converts three-dimensional information into two-dimensional information, i.e., depth information is dismissed. Therefore, the accuracy of leakage quantification using Schlieren is potentially limited. Even though the purpose of this study was not to quantify but to visualize, the method of quantifying gas leakages using Schlieren needs to be further investigated. The third limitation is that we have not been able to prove the existence of viruses in leaking gas. Additional virological approaches such as PCR testing of particulates in leaking gas would be desirable. However, under the current social conditions, it is difficult to establish an experimental system to prove the presence of viruses in gas leakages. It is necessary to assume that there is a certain risk of viral exposure and to be prepared to take countermeasures. Thirdly, all forceps insertions and removals in this study were performed manually, and thus contain compound human error. It may be possible to reduce the influence of human error by further increasing the number of trials. However, the measurement error was small for each of the five trials in this study, and the influence of human error is assumed to be relatively small.
In conclusion, gas leakage was found during insertion and removal of forceps into the plug of GI endoscopy. The type of plug and the internal pressure of the stomach were found to be related to the amount of leakage. It is desirable to develop a new forceps plug that minimizes gas leakage based on the above findings.
Data availability
The data that support the findings of this study are available on request from the corresponding author, Kiyokazu Nakajima.
References
Liu Y, Ning Z, Chen Y, Guo M, Liu Y, Gali NK, Sun L, Duan Y, Cai J, Westerdahl D, Liu X, Xu K, Ho KF, Kan H, Fu Q, Lan K (2020) Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature 582:557–560
Wang C, Horby PW, Hayden FG, Gao GF (2020) A novel coronavirus outbreak of global health concern. Lancet (London, England) 395:470–473
Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, Mehta RS, Warner ET, Sikavi DR, Lo CH, Kwon S, Song M, Mucci LA, Stampfer MJ, Willett WC, Eliassen AH, Hart JE, Chavarro JE, Rich-Edwards JW, Davies R, Capdevila J, Lee KA, Lochlainn MN, Varsavsky T, Sudre CH, Cardoso MJ, Wolf J, Spector TD, Ourselin S, Steves CJ, Chan AT (2020) Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health 5:e475–e483
Chiu PWY, Ng SC, Inoue H, Reddy DN, Ling HuE, Cho JY, Ho LK, Hewett DG, Chiu HM, Rerknimitr R, Wang HP, Ho SH, Seo DW, Goh KL, Tajiri H, Kitano S, Chan FKL (2020) Practice of endoscopy during COVID-19 pandemic: position statements of the Asian Pacific Society for Digestive Endoscopy (APSDE-COVID statements). Gut 69:991–996
Sinonquel P, Roelandt P, Demedts I, Van Gerven L, Vandenbriele C, Wilmer A, Van Wijngaerden E, Bisschops R (2020) COVID-19 and gastrointestinal endoscopy: what should be taken into account? Dig Endosc 32:723–731
Mazumdar.M (2013) Principles and Techniques of Schlieren Imaging Systems. Columbia University Computer Science Technical Reports
Miyake S, Ashikari K, Kato S, Takatsu T, Kuwashima H, Kaneko H, Nagai K, Watari I, Sato T, Yamaoka Y, Yamamoto T, Ryo A, Maeda S, Nakajima A, Higurashi T (2021) Severe acute respiratory syndrome coronavirus 2 prevalence in saliva and gastric and intestinal fluid in patients undergoing gastrointestinal endoscopy in coronavirus disease 2019 endemic areas: prospective cross-sectional study in Japan. Dig Endosc. https://doi.org/10.1111/den.13945
Takahashi H, Hirota M, Takahashi T, Yamasaki M, Miyazaki Y, Makino T, Kurokawa Y, Takiguchi S, Mori M, Doki Y, Nakajima K (2016) Simultaneous automatic insufflation and smoke-evacuation system in flexible gastrointestinal endoscopy. Endoscopy 48:579–583
Yamada T, Hirota M, Tsutsui S, Kato M, Takahashi T, Yasuda K, Sumiyama K, Tsujii M, Takehara T, Mori M, Doki Y, Nakajima K (2015) Gastric endoscopic submucosal dissection under steady pressure automatically controlled endoscopy (SPACE); a multicenter randomized preclinical trial. Surg Endosc 29:2748–2755
Hirota M, Miyazaki Y, Takahashi T, Yamasaki M, Takiguchi S, Mori M, Doki Y, Nakajima K (2014) Dynamic article: steady pressure CO2 colonoscopy; its feasibility and underlying mechanism. Dis Colon Rectum 57:1120–1128
Kato M, Nakajima K, Yamada T, Hirota M, Miyazaki Y, Yamasaki M, Nishida T, Mori M, Doki Y, Tsujii M, Takehara T (2014) Esophageal submucosal dissection under steady pressure automatically controlled endoscopy (SPACE): a clinical feasibility study. Endoscopy 46:680–684
Ushimaru Y, Nakajima K, Hirota M, Miyazaki Y, Yamashita K, Saito T, Tanaka K, Makino T, Takahashi T, Kurokawa Y, Yamasaki M, Mori M, Doki Y (2020) The endoluminal pressures during flexible gastrointestinal endoscopy. Sci Rep 10:18169
Black JRM, Bailey C, Przewrocka J, Dijkstra KK, Swanton C (2020) COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet (London, England) 395:1418–1420
Verbeek JH, Rajamaki B, Ijaz S, Sauni R, Toomey E, Blackwood B, Tikka C, Ruotsalainen JH, Kilinc Balci FS (2021) Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Emergencias 33:59–61
Urakawa S, Hirashita T, Momose K, Nishimura M, Nakajima K, Milsom JW (2021) Intraluminal gas escape from biopsy valves and endoscopic devices during endoscopy: caution advised during the COVID-19 era. Endosc Int Open 9:E443-e449
Flemming S, Hankir M, Hering I, Meybohm P, Krone M, Weissbrich B, Germer CT, Wiegering A (2020) Abdominal fluid samples (negative for SARS-CoV-2) from a critically unwell patient with respiratory COVID-19. Br J Surg 107:e259–e260
Mina MJ, Parker R, Larremore DB (2020) Rethinking Covid-19 test sensitivity—a strategy for containment. N Engl J Med 383:e120
Acknowledgements
The authors acknowledge CASTEM Co. Ltd, Fukuyama, Japan and Fujifilm Corporation, Tokyo, Japan for their technical supports. The authors acknowledge KATOKOKEN Co. Ltd, Fukuyama, Japan and Fujifilm Corporation, Tokyo, Japan for their technical supports.
Funding
This research was supported by the AMED project for the development of technologies to combat infectious diseases.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
All the authors (Drs. Tomo Ishida, Yoshinori Hayashi, Takuro Saito, Kazuyoshi Yamamoto, Kotarou Yamashita, Koji Tanaka, Tomoki Makino, Tsuyoshi Takahashi, Yukirnori Kurokawa, Hidetoshi Eguchi, Yuichiro Doki, and Kiyokazu Nakajima) have no conflicts of interest or financial ties to disclose.
Ethical approval
This research is not medical research on human subjects and does not require IRB approval or written consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ishida, T., Hayashi, Y., Saito, T. et al. Gas leakages from gastrointestinal endoscopy system—its visualization and semi-quantification utilizing schlieren optical system in the swine models. Surg Endosc 37, 1718–1726 (2023). https://doi.org/10.1007/s00464-022-09668-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09668-y