Abstract
Introduction
Despite being one of the most commonly performed operations in the US, there is a paucity of data on practice patterns and resultant long-term outcomes of groin hernia repair. In this context, we performed a contemporary assessment of operative approach with 5 year follow-up to inform care for the 800000 persons undergoing groin hernia repair annually.
Methods
This was a retrospective cohort study of adult patients undergoing elective groin hernia repair in a 20% representative Medicare sample from 2010–17. Surgical approach [minimally invasive (MIS) vs open] was defined using appropriate CPT codes. The primary outcome was operative recurrence at up to 5 years following surgery. We estimated the overall risk of operative recurrence using a multivariable Cox proportional hazards model.
Results
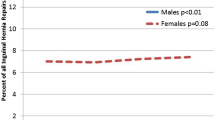
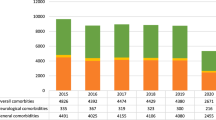
Among 118119 patients, the majority (76.4%) underwent an open repair. Compared to patients who underwent MIS repair, patients in the open surgery cohort were older (mean age 72.7 vs 71.0, p < 0.001), more often female (14.4 vs 10.9%, p < 0.001), less often white (86.9 vs 87.7%, p < 0.001), and had a higher prevalence of nearly all measured comorbidities Patients in the open cohort had a lower incidence of operative recurrence at 1-year (1.0 vs 1.5%, p < 0.001), 3-years, (2.5 vs 3.5%, p < 0.001), and 5-years (3.7 vs 4.7%, p < 0.001). In the Cox proportional hazards model, we found that patients who underwent an open groin hernia repair were significantly less likely to experience operative recurrence (HR 0.86, 95% CI 0.79–0.93).
Conclusions
In this study, we found that open groin hernia repair was associated with a lower risk of operative recurrence over time. While this may be related to patient comorbidity and age at the index operation, future work should focus on the impact of surgeon volume on outcomes in the modern era.
Graphical abstract

Similar content being viewed by others
References
El-Dhuwaib Y, Corless D, Emmett C, Deakin M, Slavin J (2013) Laparoscopic versus open repair of inguinal hernia: a longitudinal cohort study. Surg Endosc 27:936–945
Schmidt L, Oberg S, Andresen K, Rosenberg J (2018) Recurrence rates after repair of inguinal hernia in women: a systematic review. JAMA Surg 153:1135–1142
Aiolfi A et al (2021) Treatment of inguinal hernia: systematic review and updated network meta-analysis of randomized controlled trials. Ann Surg 274:954–961
Köckerling F et al (2019) Lichtenstein versus total extraperitoneal patch plasty versus transabdominal patch plasty technique for primary unilateral inguinal hernia repair: a registry-based, propensity score-matched comparison of 57906 patients. Ann Surg 269:351–357
Neumayer L et al (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Wellwood J et al (1998) Randomised controlled trial of laparoscopic versus open mesh repair for inguinal hernia: outcome and cost. BMJ 317:103–110
Ehlers AP et al (2022) Guideline-discordant care among females undergoing groin hernia repair: the importance of sex as a biologic variable. Hernia 26(3):823–829
Ehlers AP (2022) The female groin hernia: isn’t it time that we study this? Ann Surg 275:220–221
Rutkow IM (2003) Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am 83(1045–1051):v–vi
Ehlers AP, Vitous CA, Sales A, Telem DA (2020) Exploration of factors associated with surgeon deviation from practice guidelines for management of inguinal hernias. JAMA Netw Open 3:e2023684
Ehlers AP, Telem DA (2021) Decision support tools: best practice or failed experiment? Am J Surg 222:270–271
International guidelines for groin hernia management (2018) Hernia 22:1–165
Kald A et al (1998) Reoperation as surrogate endpoint in hernia surgery a three year follow-up of 1565 herniorrhaphies. Eur J Surg. 164(1):45–50
Richards MK et al (2015) A national review of the frequency of minimally invasive surgery among general surgery residents: assessment of ACGME case logs during 2 decades of general surgery resident training. JAMA Surg 150:169–172
Daes J, Felix E (2017) Critical view of the myopectineal orifice. Ann Surg 266:e1–e2
Vu JV et al (2019) Surgeon utilization of minimally invasive techniques for inguinal hernia repair: a population-based study. Surg Endosc 33:486–493
Funding
Society of American Gastrointestinal and Endoscopic Surgeons, Disparities in Healthcare Grant—Sex-Based Differences in Outcomes of Groin Hernia Repair, Anne Ehlers.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Ms. Lai, Dr. Hu, Dr. Davidson, and Dr. Waljee have no disclosures. Dr. Ehlers receives unrelated funding from the Association for Academic Surgeons and the Society for American Gastrointenstinal and Endoscopic Surgeons. Dr. Howard receives unrelated funding from the Blue Cross Blue Shield of Michigan Foundation and the National Institute of Diabetes and Digestive and Kidney Diseases (5T32DK108740-05). Dr. Dimick receives grant funding from the NIH, AHRQ, Blue Cross Blue Shield of Michigan Foundation, and is a cofounder of ArborMetrix, Inc. Dr. Telem receives funding from AHRQ K08HS025778-01A1 and receives consulting fees from Medtronic. The content of this study is solely the responsibility of the authors. No funder or sponsor had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. Dr. Ehlers had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ehlers, A.P., Lai, YL., Hu, H.M. et al. Five year trends in surgical technique and outcomes of groin hernia repair in the United States. Surg Endosc 37, 4818–4823 (2023). https://doi.org/10.1007/s00464-022-09586-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09586-z