Abstract
Background
The purpose of this study was to evaluate the effect of an enhanced recovery after surgery (ERAS) protocol on opioid and anti-emetic use, length of stay and safety after laparoscopic sleeve gastrectomy (LSG).
Methods
Patients who underwent LSG between March 2018 and January 2019 at our accredited, high-volume bariatric surgery center were randomized to either standard of care (SOC) or ERAS. ERAS included a pre- and post-surgical medication regimen designed to reduce postoperative nausea, vomiting and pain. Outcomes included post-operative symptom scores, opioid use, anti-emetic use, time to achieve readiness for discharge (RFD) and inpatient and 30-day adverse events, readmissions and emergency department visits.
Results
The final analysis included 130 patients, (SOC 65; ERAS 65). Groups did not differ on demographics or comorbidities. Relative to SOC, fewer ERAS patients utilized opioids in the hospital ward (72.3% vs. 95.4%; p < .001), peak pain scores were significantly lower, and median time to achieve RFD was shorter (28.0 h vs. 44.4 h; p = 0.001). More ERAS patients were discharged on post-operative day 1 (38.5% vs. 15.4%; p < .05). The overall use of rescue anti-emetic medications was not different between groups. Rates of postoperative 30-day events, readmissions, and emergency department visits did not differ between groups.
Conclusion
Relative to SOC, ERAS was associated with earlier discharge, lower pain scores, less frequent use of opioids and use in lower amounts after LSG with no differences in 30 day safety outcomes.
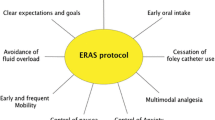
Graphical abstract



Similar content being viewed by others
References
Kehlet H (1997) Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 78(5):606–617
Thorell A, MacCormick AD, Awad S, Reynolds N, Roulin D, Demartines N, Vignaud M, Alvarez A, Singh PM, Lobo DN (2016) Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg 40(9):2065–2083
Benevides ML, Oliveira SS, de Aguilar-Nascimento JE (2013) The combination of haloperidol, dexamethasone, and ondansetron for prevention of postoperative nausea and vomiting in laparoscopic sleeve gastrectomy: a randomized double-blind trial. Obes Surg 23(9):1389–1396
Lemanu DP, Singh PP, Berridge K, Burr M, Birch C, Babor R, MacCormick AD, Arroll B, Hill AG (2013) Randomized clinical trial of enhanced recovery versus standard care after laparoscopic sleeve gastrectomy. Br J Surg 100(4):482–489
Seip RL, Lee S, McLaughlin T, Staff I, Nsereko A, Thompson S, Santana C, Tishler DS, Papasavas P (2022) Utility of a novel scale to assess readiness for discharge after bariatric surgery. World J Surg 46(1):172–179
Urbaniak, G. C., & Plous, S. (2013). Research Randomizer. Version 4.0 [Software]. [Cited June 22, 2013]. Available from http://www.randomizer.org.
Myles PS, Wengritzky R (2012) Simplified postoperative nausea and vomiting impact scale for audit and post-discharge review. Br J Anaesth 108(3):423–429
Centers for Medicare and Medicaid Services. Opioid Oral Morphine Milligram Equivalent (MME) Conversion Factors [internet]. [Cited July 7, 2020]. Available from https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-Aug-2017.pdf.
Wright JG (2007) A practical guide to assessing levels of evidence. J Bone Joint Surg Am 89(5):1128–1130
Bigal LM, Bibeau K, Dumbar SJ (2019) Patterns in opioid prescription in the United States by region and prescribers over a 4-year period. Opioid Manag 15(6):499–506
Centers for Disease Control and Prevention U.S. Opioid Prescribing Rate Maps [internet]. [Cited July 7, 2020]. Available at https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html.
Han B, Compton WM, Blanco C, Crane E, Lee J, Jones C (2017) Prescription opioid use, misuse, and use disorders in US adults: 2015 national survey on drug use and health. Ann Intern Med 167(5):293–301
Seth P, Rudd RA, Noonan RK, Haegerich T (2018) Quantifying the epidemic of prescription opioid overdose deaths. Am J Public Health 108(4):500–502
Hsu DJ, McCarthy EP, Stevens JP, Makumal K (2017) Hospitalizations, costs and outcomes associated with heroin and prescription opioid overdoses in the United States 2001–12. Addiction 112(9):1558–1564
Geubbels N, Evren I, Acherman Y, Bruin SC, van de Laar A, Hoen M, Maurits de Brauw L (2019) Randomized clinical trial of an enhanced recovery after surgery programme versus conventional care in laparoscopic Roux-en-Y gastric bypass surgery. BJS Open 3:274–281
Surve A, Cottam D, Zaveri H, Cottam A, Belnap L, Richards C, Medlin W, Duncan T, Tuggle K, Zorak A, Umbach T, Apel M, Billing P, Billing J, Landerholm R, Stewart K, Kaufman J, Harris E, Williams M, Hart C, Johnson W, Lee C, Lee C, DeBarros J, Orris M, Schniederjan B, Neichoy B, Dhorepatil A, Cottam S, Horsley B (2018) Does the future of laparoscopic sleeve gastrectomy lie in the outpatient surgery center? a retrospective study of the safety of 3162 outpatient sleeve gastrectomies. Surg Obes Relat Dis 14(10):1442–1447
Lalezari S, Musielak MC, Broun LA, Curry T (2018) Laparoscopic sleeve gastrectomy as a viable option for an ambulatory surgical procedure: our 52-month experience. Surg Obes Relat Dis 14(6):748–750
Billing P, Billing J, Harris E, Kaufman J, Landerholm R, Stewart K (2019) Safety and efficacy of outpatient sleeve gastrectomy: 2534 cases performed in a single free-standing ambulatory surgical center. Surg Obes Relat Dis 15(6):832–836
Lee Y, Yu J, Doumouras AG, Ashoorian V, Gmora S, Anvari M, Hong D (2019) Intravenous acetaminophen versus placebo in post-bariatric surgery multimodal pain management: a meta-analysis of randomized controlled trials. Obes Surg 29(4):1420–1428
Moon RC, Lastrapes L, Wier J, Nakajima M, Gaskins W, Teixeira A, Jawad M (2019) Preoperative transversus abdominis plane (TAP) block with liposomal bupivacaine for bariatric patients to reduce the use of opioid analgesics. Obes Surg 29(4):1099–1104
Pimenta GP, Capellan DA, de Aguilar-Nascimento JE (2015) Sleeve gastrectomy with or without a multimodal perioperative care: a randomized pilot study. Obes Surg 25(9):1639–1646
Cohen J (1969) Statistical Power Analysis for the Behavioral Sciences. Academic Press, New York
Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences (2nd Edition). Lawrence Erlbaum Associates, Mahwah
Hedges L, Olkin I (1985) Statistical Methods for Meta-Analysis. Academic Press, New York
Funding
The authors wish to acknowledge funding from the Hartford Hospital Medical Staff and support from the Hartford Hospital Research Committee.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Dr. Darren Tishler served as a consultant for Medtronic. Drs. Pavlos Papasavas, Richard Seip, Tara McLaughlin, Ilene Staff, Richard Gannon, Witold Waberski, Mr. Stephen Thompson, Ms. Ifeoma Mogor, Ms. Jane Sweeney have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Pain numeric rating scale
The Pain Numeric Rating Scale (which asks patients to rate their pain on a 0–10 scale) equates to categories of mild, moderate and severe pain used for medication dosing orders. The nurse describes the scale to the patient. For patients who have trouble assigning a numeric value (or understanding what the numbers between 0 and 10 indicate), descriptions of each number in relation to functional ability are as follows:
0 = no pan.
2 = mild pain, does not limit activities.
4 = moderate pain, can do most activities with rest.
6 = unable to do some activities because of pain.
8 = severe pain, unable to do most activities because of pain.
10 = excruciating, unable to do any activities because of pain.
Post-operative nausea and vomiting (ponv) impact scale
-
Q1.
Have you vomited or had dry-retching*?
-
0. No.
-
1. Once.
-
2. Twice.
-
3. Three or more times.
-
-
Q2.
Have you experienced a feeling of nausea (“an unsettled feeling in the stomach and slight urge to vomit”)? If yes, has your feeling of nausea interfered with activities of daily living, such as being able to get out of bed, being able to move about freely in bed, being able to walk normally, or eating and drinking?
-
0. Not at all.
-
1. Sometimes.
-
2. Often or most of the time.
-
3. All of the time.
-
Post-operative nausea and vomiting (ponv) impact scale
To calculate the PONV Impact Scale score, add the numerical responses to questions 1 and 2. A PONV Impact Scale score of ≥ 5 defines clinically important PONV.
*count distinct episodes: several vomits or retching events occurring over a short time frame, say 5 min, should be counted as one vomiting/dry-retching episode; multiple episodes require distinct time periods without vomiting/dry-retching.
Readiness for discharge checklist components
-
1.
Tolerate a minimum of 450 ml of bariatric liquid diet over a period of 8 h (rolling time) after starting the bariatric clear liquid diet.
-
2.
Ambulate without assistance or same level of assistance as prior to surgery.
-
3.
Attain pulse rate < 90 beats/min, temperature ≤ 37.6 °C, respiratory rate < 20 breaths/min.
-
4.
Attain pain score of 6 or less (on the 0 to 10 scale).
-
5.
Attain PONV score of 3 or less (on the 0–6 scale).
Statistical details
For categorical measures, we report the effect size as an odds ratio of the presence of the characteristic or outcome compared with its absence; for gender and ethnicity, the reference groups are male and Caucasian, respectively. For continuous variables, the effect size is typically calculated as difference in means divided by standard deviation but as distributions were not normal and non-parametric statistics were employed, the effect size reported is Cohen’s d, calculated from Cohen’s r which is recommended for Wilcoxon [22, 23] and based on the z statistic calculated for Wilcoxon. The 95% confidence interval was then calculated for Cohen’s d [24].
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Papasavas, P., Seip, R.L., McLaughlin, T. et al. A randomized controlled trial of an enhanced recovery after surgery protocol in patients undergoing laparoscopic sleeve gastrectomy. Surg Endosc 37, 921–931 (2023). https://doi.org/10.1007/s00464-022-09512-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09512-3