Abstract
Background
Optimal visualization and safety have always been essential in performing any type of endoscopic surgery. However, the safety of automatic gastrointestinal (GI) insufflation has yet to be thoroughly studied, especially when combined with manual insufflation. The current study aimed to verify whether the pressure limiter could lower GI endoluminal pressure during endoscopic procedures and affect the behavioral patterns of endoscopists.
Methods
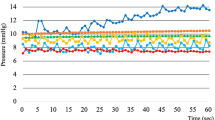
A preclinical blinded trial was conducted on endoscopists who had no knowledge regarding the presence of the pressure limiter that prevents a GI endoluminal pressure above 25 mmHg. Endoscopists in group A performed esophageal endoscopic submucosal dissection (ESD) with our insufflation device equipped with the pressure limiter, whereas those in group B performed the same procedure without the pressure limiter. During all procedures, endoluminal pressure was continuously monitored. The primary endpoint of the current study was to measure the endoluminal pressure with or without the pressure limiter during esophageal ESD, while the secondary endpoint was to evaluate the effect of the pressure limiter on intraesophageal pressure and perioperative outcomes during esophageal ESD. A questionnaire survey was conducted after each session.
Results
A total of 79 endoscopists were included in this randomized control study. Group A had significantly lower endoluminal pressure than group B (10.6 ± 4.61 vs. 16.25 ± 7.51 mmHg, respectively; p < 0.05). Although two pigs in group B died from tension pneumothorax, none in group A died. Evaluation of lumen expansion, ease of aspiration, and visual field reproducibility were poorer in group A than in group B, although all fell within the acceptable range. Subjective evaluation of usability was divided into two categories, Excellent/Good and Poor/Bad, with no significant differences in any of the items.
Conclusions
This preclinical study showed that endoscopic treatment with an automatic insufflation system could be performed at lower endoluminal pressure with a pressure limiter, which had no adverse effects on the endoscopist's feels on endoscopic procedures with the device.





Similar content being viewed by others
References
Ishizaki Y, Bandai Y, Shimomura K, Abe H, Ohtomo Y, Idezuki Y (1993) Safe intraabdominal pressure of carbon dioxide pneumoperitoneum during laparoscopic surgery. Surgery 114:549–554
Nakajima K, Nishida T, Milsom JW, Takahashi T, Souma Y, Miyazaki Y et al (2010) Current limitations in endoscopic CO2 insufflation for NOTES: flow and pressure study. Gastrointest Endosc 72:1036–1042
la Chapelle CF, Bemelman WA, Rademaker BM, van Barneveld TA, Jansen FW. A multidisciplinary evidence-based guideline for minimally invasive surgery.: Part 1: entry techniques and the pneumoperitoneum. Gynecol Surg. 2012;9:271–282.
Neudecker J, Sauerland S, Neugebauer E, Bergamaschi R, Bonjer HJ, Cuschieri A et al (2002) The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc 16:1121–1143
Joshipura VP, Haribhakti SP, Patel NR, Naik RP, Soni HN, Patel B et al (2009) A prospective randomized, controlled study comparing low pressure versus high pressure pneumoperitoneum during laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 19:234–240
Angioli R, Terranova C, Plotti F, Cafà EV, Gennari P, Ricciardi R et al (2015) Influence of pneumoperitoneum pressure on surgical field during robotic and laparoscopic surgery: a comparative study. Arch Gynecol Obstet 291:865–868
Cho YJ, Paik H, Jeong SY, Park JW, Jo WY, Jeon Y et al (2018) Lower intra-abdominal pressure has no cardiopulmonary benefits during laparoscopic colorectal surgery: a double-blind, randomized controlled trial. Surg Endosc 32:4533–4542
Vijayaraghavan N, Sistla SC, Kundra P, Ananthanarayan PH, Karthikeyan VS, Ali SM et al (2014) Comparison of standard-pressure and low-pressure pneumoperitoneum in laparoscopic cholecystectomy: a double blinded randomized controlled study. Surg Laparosc Endosc Percutan Tech 24:127–133
Cheng H, Chen BP, Soleas IM, Ferko NC, Cameron CG, Hinoul P (2017) Prolonged operative duration increases risk of surgical site infections: a systematic review. Surg Infect (Larchmt) 18:722–735
Procter LD, Davenport DL, Bernard AC, Zwischenberger JB (2010) General surgical operative duration is associated with increased risk-adjusted infectious complication rates and length of hospital stay. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2009.09.034
Fujii T, Iishi H, Tatsuta M, Hirasawa R, Uedo N, Hifumi K et al (1998) Effectiveness of premedication with pronase for improving visibility during gastroendoscopy: a randomized controlled trial. Gastrointest Endosc 47:382–387
Lee GJ, Park SJ, Kim SJ, Kim HH, Park MI, Moon W (2012) Effectiveness of premedication with pronase for visualization of the mucosa during endoscopy: a randomized. Control Trial Clin Endosc 45:161–164
Nakajima K, Yasumasa K, Endo S, Takahashi T, Nishitani A, Nezu R et al (2006) A versatile dual-channel carbon dioxide (CO2) insufflator for various CO2)applications. Prototype Surg Endosc 20:334–338
Oyama T, Tomori A, Hotta K, Morita S, Kominato K, Tanaka M et al (2005) Endoscopic submucosal dissection of early esophageal cancer. Clin Gastroenterol Hepatol 3:S67-70
Maeda Y, Hirasawa D, Fujita N, Obana T, Sugawara T, Ohira T et al (2012) A pilot study to assess mediastinal emphysema after esophageal endoscopic submucosal dissection with carbon dioxide insufflation. Endoscopy 44:565–571
Maeda Y, Hirasawa D, Fujita N, Suzuki T, Obana T, Sugawara T et al (2011) Mediastinal emphysema after esophageal endoscopic submucosal dissection: its prevalence and clinical significance. Dig Endosc 23:221–226
Oh SK, Cho SI, Won YJ, Yun JH (2021) Bilateral tension pneumothorax during endoscopic submucosal dissection under general anesthesia diagnosed by point-of-care ultrasound - A case report. Anesth Pain Med (Seoul) 16:171–176
Paspatis GA, Arvanitakis M, Dumonceau JM, Barthet M, Saunders B, Turino SY et al (2020) Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement - Update 2020. Endoscopy 52:792–810
Guo HM, Zhang XQ, Chen M, Huang SL, Zou XP (2014) Endoscopic submucosal dissection vs endoscopic mucosal resection for superficial esophageal cancer. World J Gastroenterol 20:5540–5547
Ishihara R, Iishi H, Uedo N, Takeuchi Y, Yamamoto S, Yamada T et al (2008) Comparison of EMR and endoscopic submucosal dissection for en bloc resection of early esophageal cancers in Japan. Gastrointest Endosc 68:1066–1072
Kjellberg A, Nyström H, Söderberg M, Dlugosz A, Jörnvall H, Steinberg A (2018) Massive air embolism as a complication of upper gastrointestinal endoscopy: A case report illustrating a stroke mimic, literature review, and suggested management. Clin Case Rep 6:1862–1867
Lanke G, Adler DG (2019) Gas embolism during endoscopic retrograde cholangiopancreatography: diagnosis and management. Ann Gastroenterol 32:156–167
Hirasawa D, Fujita N, Ishida K, Matsunaga A, Senoo S, Yonechi M et al (2005) Handmade outer flushing channel for safe endoscopic submucosal dissection. Dig Endosc 17:183–185
Fujishiro M, Kodashima S, Goto O, Ono S, Niimi K, Yamamichi N et al (2009) Endoscopic submucosal dissection for esophageal squamous cell neoplasms. Dig Endosc 21:109–115
Ono S, Fujishiro M, Niimi K, Goto O, Kodashima S, Yamamichi N et al (2009) Long-term outcomes of endoscopic submucosal dissection for superficial esophageal squamous cell neoplasms. Gastrointest Endosc 70:860–866
Nakajima K, Moon JH, Tsutsui S, Miyazaki Y, Yamasaki M, Yamada T et al (2012) Esophageal submucosal dissection under steady pressure automatically controlled endoscopy (SPACE): a randomized preclinical trial. Endoscopy 44:1139–1148
Hirota M, Miyazaki Y, Takahashi T, Yamasaki M, Takiguchi S, Mori M et al (2014) Dynamic article: steady pressure CO2 colonoscopy; its feasibility and underlying mechanism. Dis Colon Rectum 57:1120–1128
Kato M, Nakajima K, Yamada T, Hirota M, Miyazaki Y, Yamasaki M et al (2014) Esophageal submucosal dissection under steady pressure automatically controlled endoscopy (SPACE): a clinical feasibility study. Endoscopy 46:680–684
Yamada T, Hirota M, Tsutsui S, Kato M, Takahashi T, Yasuda K et al (2015) Gastric endoscopic submucosal dissection under steady pressure automatically controlled endoscopy (SPACE); a multicenter randomized preclinical trial. Surg Endosc 29:2748–2755
Imaeda H, Nakajima K, Hosoe N, Nakahara M, Zushi S, Kato M et al (2016) Percutaneous endoscopic gastrostomy under steady pressure automatically controlled endoscopy: First clinical series. World J Gastrointestinal Endosc 8:186–191
Ushimaru Y, Nakajima K, Hirota M, Miyazaki Y, Yamashita K, Saito T et al (2020) The endoluminal pressures during flexible gastrointestinal endoscopy. Sci Rep 10:18169
Bhattacharya K (2007) Kurt Semm: A laparoscopic crusader. J Minim Access Surg 3:35–36
Mikami O, Fujise K, Matsumoto S, Shingu K, Ashida M, Matsuda T (1998) High intra-abdominal pressure increases plasma catecholamine concentrations during pneumoperitoneum for laparoscopic procedures. Arch Surg 133:39–43
Struthers AD, Cuschieri A (1998) Cardiovascular consequences of laparoscopic surgery. Lancet (London, England) 352:568–570
Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A et al (2015) Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 47:829–854
Oda I, Gotoda T, Hamanaka H, Eguchi T, Saito Y, Matsuda T et al (2005) Endoscopic submucosal dissection for early gastric cancer : Technical feasibility, operation time and complications from a large consecutive series. Dig Endosc 17:54–58
Onozato Y, Ishihara H, Iizuka H, Sohara N, Kakizaki S, Okamura S et al (2006) Endoscopic submucosal dissection for early gastric cancers and large flat adenomas. Endoscopy 38:980–986
Hamada K, Kawano K, Yamauchi A, Koyanagi R, Horikawa Y, Nishida S et al (2019) Efficacy of endoscopic submucosal dissection of esophageal neoplasms under general anesthesia. Clinical endoscopy 52:252–257
Ushimaru Y, Doki Y, Nakajima K (2021) Monitoring of surgeon’s surgical skills using internet of things-enabled medical instruments. In: Takenoshita S, Yasuhara H (eds) Surgery and operating room innovation. Springer Singapore, Singapore, pp 33–43
Ushimaru Y, Takahashi T, Souma Y, Yanagimoto Y, Nagase H, Tanaka K et al (2019) Innovation in surgery/operating room driven by Internet of Things on medical devices. Surg Endosc 33:3469–3477
Kamba S, Kobayashi M, Koizumi A, Ono S, Hara Y, Shimamoto N et al (2019) Intra-abdominal pressure during endoscopic full-thickness resection comparing manual and automatic control insufflation: a block-randomized porcine study. Surg Endosc 34:1625–1633
Acknowledgements
This research project benefited from the support and time of many individuals. The authors would like to acknowledgement the support, help and guidance of Drs. N. Abe, S. Abe, M. Aimi, Y. Ban, R. Fujii. Y. Makino, H. Matsui, H. Mikami, T. Mitani, Y. Miyabe, R. Mizumoto, H. Mori, Y. Morita, M. Murata, K. Nagai, H. Nakashima, T. Nishida, A. Nishihara, Y. Nishizawa, S. Nonaka, N. Hayashi, K. Hara, M. Horie, J. Horii, S. Hoteya, Y. Ida, A. Iida, H. Imaeda, T. Ishida, M. Ishihara, R. Ishihara, M. Ito, H. Kageyama, M. Kaise, H. Kawahira, D. Kikuchi, M. Kobayashi, H. Kondo, Y. Ochiai, H. Ogawa, H. Ogiyama, A. Ohki, T. Ohya, H. Okuda, A. Onishi, K. Ota, Y. Saida, Y. Saito, K. Sato, H. Shiroshita, Y. Souma, K. Sumiyama, T. Sumiyoshi, T. Takao, H. Takeuchi, T. Tanaka, A. Tomita, S. Tsutsui, T. Uraoka, M. Yagi, S. Yamaguchi, K. Yamamoto, Y. Yamamoto, S. Yamamoto, K. Yasuda, and S. Yoshii. This study received no specific funding.
Author information
Authors and Affiliations
Contributions
Nakajima designed the study, and Ushimaru wrote the initial draft of the manuscript. Nakajima and Ushimaru also contributed to the interpretation of the data and critical revision of the manuscript for important intellectual content. All the other authors (Takahashi, Yamashita, Saito, Tanaka, Yamamoto, Makino, Kurokawa, and Eguchi, Doki) contributed to data collection and interpretation and critical review of the manuscript. All the authors have read and approved the final version of the manuscript and have agreed to the accountability of all aspects of the study, ensuring its accuracy and integrity.
Corresponding author
Ethics declarations
Disclosures
Yuki Ushimaru, Tsuyoshi Takahashi, Kotaro Yamashita, Takuro Saito, Koji Tanaka, Kazuyoshi Yamamoto, Tomoki Makino, Yukinori Kurokawa, Hidetoshi Eguchi, Yuichiro Doki, and Kiyokazu Nakajima have no conflicts of interest or financial ties to declare.
Ethical approval
All procedures in this study were performed in accordance with the ethical standards of the responsible committee on institutional human experimentation and with the Helsinki Declaration of 1964 and later versions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ushimaru, Y., Takahashi, T., Yamashita, K. et al. Translation from manual to automatic endoscopic insufflation enhanced by a pressure limiter. Surg Endosc 36, 7038–7046 (2022). https://doi.org/10.1007/s00464-022-09040-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09040-0