Abstract
Background
Peroral endoscopic myotomy (POEM) is gaining traction as a minimally invasive treatment of achalasia. Increased reflux is reported after POEM but the incidence, type and severity of reflux are not fully understood. We aimed to study the prevalence and nature of reflux after POEM and correlate reflux with endoscopy and pH-impedance findings.
Methods
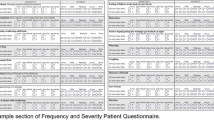
This is a prospective cohort study of achalasia patients undergoing POEM since 2014. Data from Eckardt and GERD symptom scores, high-resolution oesophageal manometry (HRM) and gastroscopy were performed pre-procedure and repeated at 1-year follow-up. Data from 24-h pH-impedance, if performed, were also recorded. A standardized questionnaire was used to determine the severity and frequency of heartburn symptoms and the composite score for each patient was calculated.
Results
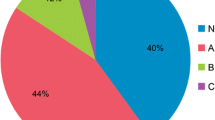
58 patients underwent POEM between January 2014 and October 2018. The efficacy of POEM at 1 year was 93.0%. We observed reduction of median Integrated Relaxation Pressure (IRP) from 23.5 ± 33.1 mmHg to 13.4 ± 7.71 mmHg (p = 0.005) and mean Eckardt score improved from 6.09 ± 2.43 points to 1.16 ± 1.70 points (p < 0.001). At 1 year, 43.1% (n = 25) had symptomatic reflux. Of the 40 patients who underwent repeated gastroscopy, 60.0% (n = 24) had endoscopic evidence of oesophagitis with seven patients (18%) diagnosed with Grade C or D oesophagitis. 43.1% (n = 25) of patients had pH-impedance done post-POEM off PPIs. 14 patients (56%) had increased acid exposure. Sixteen percent of reflux episodes were acidic and 77.3% were weakly acidic.
Conclusion
POEM was an effective treatment for achalasia. However, GERD was common after POEM with incidence of 43% on symptom score, 60% on endoscopy and 56% on pH-impedance test. Post-POEM reflux appeared to be predominantly acidic in nature. Routine surveillance for GERD after POEM is recommended.

Similar content being viewed by others
References
Akintoye E et al (2016) Peroral endoscopic myotomy: a meta-analysis. Endoscopy 48(12):1059–1068
Werner YB et al (2019) Endoscopic or surgical myotomy in patients with idiopathic achalasia. N Engl J Med 381(23):2219–2229
Chan SM et al (2016) Comparison of early outcomes and quality of life after laparoscopic Heller’s cardiomyotomy to peroral endoscopic myotomy for treatment of achalasia. Dig Endosc 28(1):27–32
Docimo S Jr et al (2017) Reduced postoperative pain scores and narcotic use favor per-oral endoscopic myotomy over laparoscopic Heller myotomy. Surg Endosc 31(2):795–800
Costantini A et al (2020) Poem versus laparoscopic heller myotomy in the treatment of esophageal achalasia: a case-control study from two high volume centers using the propensity score. J Gastrointest Surg 24(3):505–515
de Pascale S et al (2017) Peroral endoscopic myotomy versus surgical myotomy for primary achalasia: single-center, retrospective analysis of 74 patients. Dis Esophagus 30(8):1–7
Wang XH et al (2016) Full-thickness myotomy is associated with higher rate of postoperative gastroesophageal reflux disease. World J Gastroenterol 22(42):9419–9426
Mota RCL et al (2020) Risk factors for gastroesophageal reflux after POEM for achalasia: a systematic review and meta-analysis. Surg Endosc 35:383
Grimes KL et al (2019) Gastric myotomy length affects severity but not rate of post-procedure reflux: 3-year follow-up of a prospective randomized controlled trial of double-scope per-oral endoscopic myotomy (POEM) for esophageal achalasia. Surg Endosc 34:2963
Tan Y et al (2018) Efficacy of anterior versus posterior per-oral endoscopic myotomy for treating achalasia: a randomized, prospective study. Gastrointest Endosc 88(1):46–54
Ramchandani M et al (2018) Outcomes of anterior myotomy versus posterior myotomy during POEM: a randomized pilot study. Endosc Int Open 6(2):E190–E198
Sanaka MR et al (2019) Peroral endoscopic myotomy leads to higher rates of abnormal esophageal acid exposure than laparoscopic Heller myotomy in achalasia. Surg Endosc 33(7):2284–2292
Arevalo G et al (2019) Post-POEM reflux: who’s at risk? Surg Endosc 34:3163
Farre R et al (2008) Short exposure of oesophageal mucosa to bile acids, both in acidic and weakly acidic conditions, can impair mucosal integrity and provoke dilated intercellular spaces. Gut 57(10):1366–1374
Monaco L et al (2009) Prevalence of bile reflux in gastroesophageal reflux disease patients not responsive to proton pump inhibitors. World J Gastroenterol 15(3):334–338
Takahashi Y et al (2011) Impact of the composition of gastric reflux bile acids on Barrett’s oesophagus. Dig Liver Dis 43(9):692–697
Chan DK et al (2017) A training model for introducing a novel surgical procedure into clinical practice: our experience on peroral endoscopic myotomy for achalasia. Ann Acad Med Singap 46(3):111–114
Kahrilas PJ et al (2015) The Chicago Classification of esophageal motility disorders, v.30. Neurogastroenterol Motil 27(2):160–74
Grimes KL et al (2016) Double-scope per oral endoscopic myotomy (POEM): a prospective randomized controlled trial. Surg Endosc 30(4):1344–1351
Gaspar LE et al (2001) Swallowing function and weight change observed in a phase I/II study of external-beam radiation, brachytherapy and concurrent chemotherapy in localized cancer of the esophagus (RTOG 9207). Cancer J 7(5):388–394
American Society for Gastrointestinal Endoscopy, P.C. et al (2015) The American Society for Gastrointestinal Endoscopy PIVI (preservation and incorporation of valuable endoscopic innovations) on peroral endoscopic myotomy. Gastrointest Endosc 81(5):1087–100 e1
Amarasiri LD et al (2010) Comparison of a composite symptom score assessing both symptom frequency and severity with a score that assesses frequency alone: a preliminary study to develop a practical symptom score to detect gastro-oesophageal reflux disease in a resource-poor setting. Eur J Gastroenterol Hepatol 22(6):662–668
Allen CJ et al (2000) Reproducibility, validity, and responsiveness of a disease-specific symptom questionnaire for gastroesophageal reflux disease. Dis Esophagus 13(4):265–270
Von Renteln D et al (2013) Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology 145(2):309–11 e1–3
Kumbhari V et al (2017) Gastroesophageal reflux after peroral endoscopic myotomy: a multicenter case-control study. Endoscopy 49(7):634–642
Shoenut JP et al (1995) Reflux in untreated achalasia patients. J Clin Gastroenterol 20(1):6–11
Crookes PF, Corkill S, DeMeester TR (1997) Gastroesophageal reflux in achalasia. When is reflux really reflux? Dig Dis Sci 42(7):1354–61
Katz PO et al (1986) Apparent complete lower esophageal sphincter relaxation in achalasia. Gastroenterology 90(4):978–983
Koetje JH et al (2016) Measuring outcomes of laparoscopic anti-reflux surgery: quality of life versus symptom scores? World J Surg 40(5):1137–1144
Zhong C et al (2020) Quality of life following peroral endoscopic myotomy for esophageal achalasia: a systematic review and meta-analysis. Ann Thorac Cardiovasc Surg 26:113
Familiari P et al (2016) Gastroesophageal reflux disease after peroral endoscopic myotomy: analysis of clinical, procedural and functional factors, associated with gastroesophageal reflux disease and esophagitis. Dig Endosc 28(1):33–41
Jones EL et al (2016) Gastroesophageal reflux symptoms do not correlate with objective pH testing after peroral endoscopic myotomy. Surg Endosc 30(3):947–952
Mermelstein J, Chait Mermelstein A, Chait MM (2018) Proton pump inhibitor-refractory gastroesophageal reflux disease: challenges and solutions. Clin Exp Gastroenterol 11:119–134
Vaezi MF, Richter JE (2001) Duodenogastroesophageal reflux and methods to monitor nonacidic reflux. Am J Med 111(Suppl 8A):160S-168S
Ren Y et al (2016) Myotomy of distal esophagus influences proximal esophageal contraction and upper esophageal sphincter relaxation in patients with achalasia after peroral endoscopic myotomy. J Neurogastroenterol Motil 22(1):78–85
Gyawali CP et al (2018) Modern diagnosis of GERD: the Lyon Consensus. Gut 67(7):1351–1362
Inoue H et al (2019) Peroral endoscopic myotomy and fundoplication: a novel NOTES procedure. Endoscopy 51(2):161–164
Knight BC et al (2017) Long-term efficacy of laparoscopic antireflux surgery on regression of Barrett’s esophagus using BRAVO wireless pH monitoring: a prospective clinical cohort study. Ann Surg 266(6):1000–1005
Chang EY et al (2007) The effect of antireflux surgery on esophageal carcinogenesis in patients with Barrett esophagus: a systematic review. Ann Surg 246(1):11–21
Corey KE, Schmitz SM, Shaheen NJ (2003) Does a surgical antireflux procedure decrease the incidence of esophageal adenocarcinoma in Barrett’s esophagus? A meta-analysis. Am J Gastroenterol 98(11):2390–2394
Nurczyk K, Farrell TM, Patti MG (2020) Antireflux surgery for gastroesophageal reflux refractory to medical treatment after peroral endoscopic myotomy. J Laparoendosc Adv Surg Tech A 30:612
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. JL Teh, HY Tham, A Soh, A Shabbir, GW Kim, R Wong and JBY So have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Teh, J.L., Tham, H.Y., Soh, A.Y.S. et al. Gastro-esophageal reflux disease (GERD) after peroral endoscopic myotomy (POEM). Surg Endosc 36, 3308–3316 (2022). https://doi.org/10.1007/s00464-021-08644-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08644-2