Abstract
Introduction
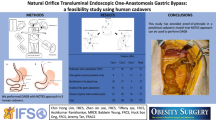
Endoscopic bariatric therapies (EBT) are emerging as effective therapies in the management of overweight patient with or without metabolic syndrome. Unfortunately most procedures only restrict the gastric volume without altering the underlying metabolism which is seen in surgical patients. The aim of this study was to investigate the feasibility and limitations of a natural orifice trans-luminal endoscopic surgery (NOTES) one anastomosis gastric bypass (OAGB).
Methods
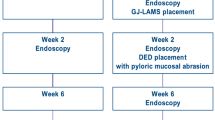
NOTES OAGB was performed in three porcine models. The steps of the procedure can be divide as follows:
-
(1) Endoscopic sleeve gastroplasty.
-
(2) Trans-gastric access to peritoneal cavity.
-
(3) Identification of a loop of jejunum.
-
(4) Introduction of the jejunal loop into the stomach.
-
(5) Creation of the gastro-jejunostomy with lumen-apposing metal stent (LAMS).
-
(6) Closure of gastric pylorus with overstitch system.
Results
All the animals underwent successful NOTES of OAGB. The mean weight for the animals was 34.3 kg (32–37 kg). The mean procedure time was 250 min (300 min for first animal and 180 min for third animal). The average bypassed bilio-pancreatic limb was 98 cm (range 65–130 cm).
Conclusions
This study has provided proof-of-principle in a preclinical model that a NOTES approach can be used to perform OAGB and, therefore, merits additional evaluation and consideration.







Similar content being viewed by others
References
International Diabetes Federation Website (2013) http://www.idf.org/diabetesatlas. Accessed 19 Jan 2021
Pories WJ et al (1995) Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 222(3):339–350
Sjostrom L, Narbo K, Sjostrom D et al (2007) Effects of bariatric surgery on mortality in Swedish obese subjects. New Engl J Med 357:741–752
ASMBS (2018) Estimate of bariatric surgery numbers 2011–2017 Gainesville, FL. https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers. 21 Jan 2012
Hickey MS, Pories WJ, MacDonald KG Jr et al (1998) A new paradigm for type 2 diabetes mellitus: could it be a disease of the foregut? Ann Surg 227:637–643
Pories WJ, Albrecht RJ (2001) Etiology of type II diabetes mellitus: role of the foregut. World J Surg 25:527–531
Rubino F, Forgione A, Cummings DE et al (2006) The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg 244:741–749
Rubino F, Marescaux J (2004) Effect of duodenal-jejunal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease. Ann Surg 239:1–11
van Baar ACG, Holleman F, Crenier L, Haidry R, Magee C et al (2019) Endoscopic duodenal mucosal resurfacing for the treatment of type 2 diabetes mellitus: one year results from the first international, open-label, prospective, multicentre study. Gut 69(2):295–303
Schouten R, Rijs CS, Bouvy ND et al (2010) A multicentre, randomized efficacy study of the endobarrier gastrointestinal liner for pre-surgical weight loss prior to bariatric surgery. Ann Surg 251(2):236–243
Rutledge R, Walsh TR (2005) Continued excellent results with the mini-gastric bypass six-year study in 2410 patients. Obes Surg 15(9):1304–1308
Lee WJ, Yu PJ, Wang W et al (2005) Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity. Ann Surg 242(1):20–28
Lee WJ, Chong K, Ser KH et al (2011) Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch Surg 146(2):143–148
Hagen ME, Wagner OJ, Swain P et al (2008) Hybrid natural orifice transluminal endoscopic surgery (NOTES) for Roux-en-Y gastric bypass: an experimental surgical study in human cadavers. Endoscopy 40(11):918–924
Madan AK, Tichansky DS, Khan KA et al (2008) Natural orifice transluminal endoscopic gastric bypass performed in cadaver. Obes Surg 18(9):1192–1199
Chang JHE, Tan D, Chan WH, Lim CH (2019) Endoscopic partial reversal of complicated single anastomosis gastric bypass. Endoscopy 51(5):E108–E110
Lim CH, Amateur SK, McDonald NM et al (2018) EUS-guided endoscopic gastrointestinal anastomosis with lumen-apposing metal stent: feasibility, safety, and efficacy. Obes Surg 28(5):1445–1451
Lim CH, Ikramuddin S, Leslie DB, Amateau SK et al (2016) Novel endoscopic management of a pancreatico-biliary limb obstruction by the creation of an entero-enterostomy following Roux-en-Y gastric bypass. Endoscopy 48(01):99–100
Lauti M, Kularatna M, Hill AG (2016) Weight regain following sleeve gastrectomy: a systematic review. Obes Surg 26:1326–1334
Tankel J, Neumann M, Mintz A (2017) Weight regain 5 years after laparoscopic sleeve gastrectomy: balancing the benefits. Surg Obes Relat Dis 13:S112
Chow A, Purkayastha S, Dosanjh D et al (2012) Patient reported outcomes and their importance in the development of novel surgical techniques. Surg Innov 19(3):327–334
Swanstorm LL, Volckmann E, Hungness E et al (2009) Patient attitudes and expectations regarding natural orifice tramsluminal endoscopic surgery. Surg Endosc 23(7):1519–1525
Bowrey DJ, Blom D, Crookes PF et al (2001) Risk factors and the prevalence of trocar-site herniation after laparoscopic fundoplication. Surg Endosc 15:663–666
Pizzicannella M, Lapergola A, Fiorillo C et al (2020) Does endoscopic sleeve gastroplasty stand the test of time? Objective assessment of endoscopic ESG appearance and its relation to weight loss in a large group of consecutive patients. Surg Endosc 34:3696–3705
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Chin Hong Lim, Zhen Jin Lee, Baldwin Yeung, Tiffany Lye, Hock Soo Ong and Jeremy Tan have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 174973 kb) Video 1: One anastomosis gastric bypass with natural orifice trans-luminal endoscopic surgery approach.
Rights and permissions
About this article
Cite this article
Lim, C.H., Lee, Z.J., Yeung, B. et al. Natural orifice transluminal endoscopic one-anastomosis gastric bypass: a feasibility study using porcine model. Surg Endosc 35, 5842–5851 (2021). https://doi.org/10.1007/s00464-021-08547-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08547-2