Abstract
Background and aims
POEM is a rescue endoscopic therapy for patients who had previously failed surgical or endoscopic treatment. However, data regarding its effectiveness after failed pneumatic dilation (PD) and its long-term effects are limited. We aimed to retrospectively investigate the long-term outcomes in patients who had undergone POEM after failed PD.
Methods
Data from 66 achalasia patients with a 2-year follow-up period were analyzed. Intraprocedural events were compared between the first POEM group (patients without prior-endoscopic intervention) and prior PD group (patients who had pre-POEM PD). Symptom evaluation, HRM and 24 h-pH DeMeester scores between the two groups were performed at 2 years after the POEM procedure. Muscularis externa samples were obtained from the lower esophagus using POEM to assess the muscle fibrosis with Azan-Mallory staining.
Results
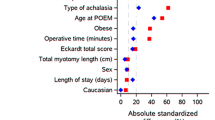
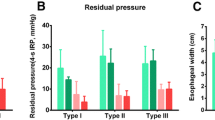
POEM was successfully performed for all achalasia patients. During the 2-year follow-up period, the success rate of POEM was 96.15% (25/26) for patients with prior PD and 95% (38/40) with primary POEM. For patients with type II achalasia and who underwent prior PD, the post-procedure DeMeester score was higher compared to patients who underwent POEM only (P < 0.05). A larger number of patients who underwent primary POEM (27.50%, 11/40) complained of mild heartburn compared to patients who underwent POEM after PD (7.69%, 2/26) (P < 0.05). With regards to fibrosis, the majority of patients who underwent POEM only were classified as F-1 (45.00%, 18/40), while the majority of patients who underwent prior PD were classified as F-2 (42.3%, 11/26). The degree of fibrosis was significantly different between the two groups (P < 0.05). Both surgical time and prior PD were correlated with the degree of fibrosis (P < 0.05).
Conclusions
Despite the technical challenges, pre-POEM endoscopic treatment does not impact the safety and efficacy of POEM in achalasia patients. Longer follow-up studies using larger cohorts are needed to determine long-term outcomes and complications of POEM.



Similar content being viewed by others
References
Boeckxstaens GE, Zaninotto G, Richter JE (2014) Achalasia. Lancet 383(9911):83–93
Ling T, Guo H, Zou X (2014) Effect of peroral endoscopic myotomy in achalasia patients with failure of prior pneumatic dilation: a prospective case-control study. J Gastroenterol Hepatol 29(8):1609–1613
Kilic A, Schuchert MJ, Pennathur A et al (2009) Long-term outcomes of laparoscopic Heller myotomy for achalasia. Surgery 146(4):826–833
Borges AA, Lemme EM, Abrahao LJ et al (2014) Pneumatic dilation versus laparoscopic Heller myotomy for the treatment of achalasia: variables related to a good response. Dis Esophagus 27(1):18–23
Bonifacio P, de Moura DTH, Bernardo WM et al (2018) Pneumatic dilation versus laparoscopic Heller’s myotomy in the treatment of achalasia: systematic review and meta-analysis based on randomized controlled trials. Dis Esophagus 32:1–9
Emami MH, Raisi M, Amini J et al (2008) Pneumatic balloon dilation therapy is as effective as esophagomyotomy for achalasia. Dysphagia 23(2):155–160
Kumbhari V, Behary J, Szczesniak M et al (2013) Efficacy and safety of pneumatic dilatation for achalasia in the treatment of post-myotomy symptom relapse. Am J Gastroenterol 108(7):1076–1081
Yaghoobi M, Mayrand S, Martel M et al (2013) Laparoscopic Heller’s myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized, controlled trials. Gastrointest Endosc 78(3):468–475
Inoue H, Tianle KM, Ikeda H et al (2011) Peroral endoscopic myotomy for esophageal achalasia: technique, indication, and outcomes. Thorac Surg Clin 21(4):519–525
Orenstein SB, Raigani S, Wu YV et al (2015) Peroral endoscopic myotomy (POEM) leads to similar results in patients with and without prior endoscopic or surgical therapy. Surg Endosc 29(5):1064–1070
Jones EL, Meara MP, Pittman MR et al (2016) Prior treatment does not influence the performance or early outcome of per-oral endoscopic myotomy for achalasia. Surg Endosc 30(4):1282–1286
Louie BE, Schneider AM, Schembre DB et al (2017) Impact of prior interventions on outcomes during per oral endoscopic myotomy. Surg Endosc 31(4):1841–1848
Ngamruengphong S, Inoue H, Ujiki MB et al (2017) Efficacy and safety of peroral endoscopic myotomy for treatment of achalasia after failed Heller myotomy. Clin Gastroenterol Hepatol 15(10):1531–1537
Wu QN, Xu XY, Zhang XC et al (2017) Submucosal fibrosis in achalasia patients is a rare cause of aborted peroral endoscopic myotomy procedures. Endoscopy 49(8):736–744
Stavropoulos SN, Modayil R, Friedel D (2015) Per oral endoscopic myotomy for the treatment of achalasia. Curr Opin Gastroenterol 31(5):430–440
Patel KS, Calixte R, Modayil RJ et al (2015) The light at the end of the tunnel: a single-operator learning curve analysis for per oral endoscopic myotomy. Gastrointest Endosc 81(5):1181–1187
Zhang X, Modayil RJ, Friedel D et al (2018) Per-oral endoscopic myotomy in patients with or without prior Heller’s myotomy: comparing long-term outcomes in a large US single-center cohort (with videos). Gastrointest Endosc 87(4):972–985
Nakajima N, Sato H, Takahashi K et al (2017) Muscle layer histopathology and manometry pattern of primary esophageal motility disorders including achalasia. Neurogastroenterol Motil. https://doi.org/10.1111/nmo.12968
Ramchandani M, Nageshwar RD, Nabi Z et al (2018) Management of achalasia cardia: expert consensus statements. J Gastroenterol Hepatol 33:1436–1444
Boeckxstaens GE, Annese V et al (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364(19):1807–1816
Tang X, Gong W, Deng Z et al (2017) Feasibility and safety of peroral endoscopic myotomy for achalasia after failed endoscopic interventions. Dis Esophagus 30(3):1–6
Sharata A, Kurian AA, Dunst CM et al (2013) Peroral endoscopic myotomy (POEM) is safe and effective in the setting of prior endoscopic intervention. J Gastrointest Surg 17(7):1188–1192
Liu ZQ, Li QL, Chen WF et al (2019) The effect of prior treatment on clinical outcomes in patients with achalasia undergoing peroral endoscopic myotomy. Endoscopy 51(04):307–316
Hungness ES, Teitelbaum EN, Santos BF et al (2013) Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg 17(2):228–235
Ujiki MB, Yetasook AK, Zapf M et al (2013) Peroral endoscopic myotomy: a short-term comparison with the standard laparoscopic approach. Surgery 154(4):893–900
Rohof WO, Salvador R, Annese V et al (2013) Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology 144(4):718–725
Novais PA, Lemme EM (2010) 24-h pH monitoring patterns and clinical response after achalasia treatment with pneumatic dilation or laparoscopic Heller myotomy. Aliment Pharmacol Ther 32(10):1257–1265
Mauro A, Franchina M, Elvevi A et al (2017) Yield of prolonged wireless pH monitoring in achalasia patients successfully treated with pneumatic dilation. United Eur Gastroenterol J 5(6):789–795
Xu S, Chai N, Tang X et al (2020) Outcomes of peroral endoscopic myotomy in challenging achalasia patients: a long-term follow-up study. Surg Endosc. https://doi.org/10.1007/s00464-020-07864-2
Sato H, Takahashi K, Mizuno KI et al (2018) Esophageal motility disorders: new perspectives from high-resolution manometry and histopathology. J Gastroenterol 53(4):484–493
Acknowledgements
Ethical NO. IRB2014-YX-064. This work was supported by the National Natural Science Foundation of China under Grant [No. 81370492]. This work was supported by the Tianjin Zhao Yicheng Medical Science Foundation [No. ZYYFY 2018021].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Hong Jin, Bin Wang, Zhong-qing Zheng, Li-li Zhang, Qiu-yu Chen, Chun Shan Zhao, Bang-mao Wang and Wei Zhao have no conflict of interest of financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jin, H., Wang, B., Zheng, Zq. et al. Peroral endoscopic myotomy for the treatment of achalasia after failed pneumatic dilation. Surg Endosc 35, 6960–6968 (2021). https://doi.org/10.1007/s00464-020-08207-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08207-x