Abstract
Background
In endoscopic retrograde cholangiopancreatography (ERCP), reduction of pressure inside of the bile duct by bile aspiration is a well-known method to lower the rate of adverse events (AEs) including cholangitis. Endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) has been introduced as an alternative to ERCP. The use of self-expandable metallic stents is recommended in EUS-HGS to reduce bile leak; however, other methods to reduce the rate of AEs including bile leak, abdominal pain, fever, and sepsis, have not been elucidated yet. This study investigated whether bile aspiration during EUS-HGS decreased the rate of postprocedural AEs.
Methods
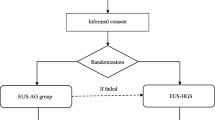
Consecutive patients who underwent EUS-HGS between July 2016 and April 2020 were retrospectively evaluated in this study. EUS-HGS was performed at a tertiary cancer center. Patient characteristics, site of biliary obstruction, the quantity of bile aspirated during EUS-HGS, type of stent, whether or not antegrade stenting (AS) was performed, procedure time, and AEs were assessed based on a prospectively recorded institutional endoscopy database. Logistic regression analysis was performed to identify factors affecting postprocedural AEs.
Results
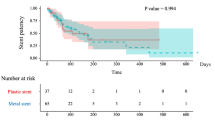
Ninety-six patients were included in the study. EUS-guided HGS with and without AS was performed in 45 and 51 patients, respectively. Bile was aspirated in 71 patients (74%). The quantity of bile aspirated was 0–10 mL and > 10 mL in 40 and 56 patients, respectively. AEs including fever, abdominal pain, postprocedural cholangitis, sepsis, acute pancreatitis, and bleeding occurred in 45 patients (47%). The AE rates were 65% (26/40) and 34% (19/56), for 0–10 mL and > 10 mL bile, respectively (p = 0.004). Using multivariate analysis, the only independent factor affecting the occurrence of AEs was found to be an aspirated bile amount of 0–10 mL (odds ratio: 4.16; 95% CI 1.6–10.8).
Conclusions
Bile aspiration of more than 10 mL during EUS-HGS contributes to reducing the rate of postprocedural AEs.


Similar content being viewed by others
References
Ekkelenkamp VE, de Man RA, Ter Borg F, Borg PC, Bruno MJ, Groenen MJ, Hansen BE, van Tilburg AJ, Rauws EA, Koch AD (2015) Prospective evaluation of ERCP performance: results of a nationwide quality registry. Endoscopy 47:503–507
Baron TH, Petersen BT, Mergener K, Chak A, Cohen J, Deal SE, Hoffman B, Jacobson BC, Petrini JL, Safdi MA, Faigel DO, Pike IM (2006) Quality indicators for endoscopic retrograde cholangiopancreatography. Gastrointest Endosc 63:S29–S34
Teoh AYB, Dhir V, Kida M, Yasuda I, Jin ZD, Seo DW, Almadi M, Ang TL, Hara K, Hilmi I, Itoi T, Lakhtakia S, Matsuda K, Pausawasdi N, Puri R, Tang RS, Wang HP, Yang AM, Hawes R, Varadarajulu S, Yasuda K, Ho LKY (2018) Consensus guidelines on the optimal management in interventional EUS procedures: results from the Asian EUS group RAND/UCLA expert panel. Gut 67:1209–1228
Isayama H, Nakai Y, Itoi T, Yasuda I, Kawakami H, Ryozawa S, Kitano M, Irisawa A, Katanuma A, Hara K, Iwashita T, Fujita N, Yamao K, Yoshida M, Inui K (2019) Clinical practice guidelines for safe performance of endoscopic ultrasound/ultrasonography guided biliary drainage: 2018. J Hepatobiliary Pancreat Sci 26:249–269
Giovannini M, Dotti M, Bories E, Moutardier V, Pesenti C, Danisi C, Delpero JR (2003) Hepaticogastrostomy by echo-endoscopy as a palliative treatment in a patient with metastatic biliary obstruction. Endoscopy 35:1076–1078
Giovannini M, Moutardier V, Pesenti C, Bories E, Lelong B, Delpero JR (2001) Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy 33:898–900
Ishiwatari H, Satoh T, Sato J, Kaneko J, Ohgi K, Matsubayashi H, Uesaka K (2019) Endoscopic ultrasound-guided rendezvous for access to the right posterior bile duct in a surgical candidate. Endoscopy. https://doi.org/10.1055/a-1046-1475
Ishiwatari H, Satoh T, Sato J, Kaneko J, Matsubayashi H, Ono H (2019) Double-guidewire technique facilitates endoscopic ultrasound-guided biliary drainage for hilar biliary obstruction. Endoscopy 51:E321–E322
Sato J, Ishiwatari H, Satoh T, Fujie S, Kaneko J, Matsubayashi H, Ono H (2019) Two-step endoscopic ultrasound-guided drainage of an isolated posterior bile duct because of an enlarged gallbladder. Endoscopy 51:E347–E348
Ishiwatari H, Sato J, Kaneko J (2019) Hepaticojejunostomy for the right hepatic bile duct using a forward-viewing echoendoscope in a patient after pancreatoduodenectomy. Dig Endosc 31:e82–e83
Park SJ, Choi JH, Park DH, Choi JH, Lee SS, Seo DW, Lee SK, Kim MH (2013) Expanding indication: EUS-guided hepaticoduodenostomy for isolated right intrahepatic duct obstruction (with video). Gastrointest Endosc 78:374–380
Gupta K, Perez-Miranda M, Kahaleh M, Artifon EL, Itoi T, Freeman ML, de Serna C, Sauer B, Giovannini M, InEBD STUDY GROUP (2014) Endoscopic ultrasound-assisted bile duct access and drainage: Multicenter, long-term analysis of approach, outcomes, and complications of a technique in evolution. J Clin Gastroenterol 48:80–87
Hedjoudje A, Sportes A, Grabar S, Zhang A, Koch S, Vuitton L, Prat F (2019) Outcomes of endoscopic ultrasound-guided biliary drainage: a systematic review and meta-analysis. United Eur Gastroenterol J 7:60–68
Khashab MA, Messallam AA, Penas I, Nakai Y, Modayil RJ, De la Serna C, Hara K, El Zein M, Stavropoulos SN, Perez-Miranda M, Kumbhari V, Ngamruengphong S, Dhir VK, Park DH (2016) International multicentre comparative trial of transluminal EUS0guided biliary drainage via hepatogastrostomy vs. choledochoduodenostomy approaches. Endosc Int Open 4:E175–E181
Krishnamoorthi R, Dasari CS, Thoguluva Chandrasekar V, Priyan H, Jayaraj M, Law J, Larsen M, Kozarek R, Ross A, Irani S (2020) Effectiveness and safety of EUS-guided choledochoduodenostomy using lumen-apposing metal stents (LAMS): a systematic review and meta-analysis. Surg Endosc 34:2866–2877
Hara K, Yamao K, Mizuno N, Hijioka S, Imaoka H, Tajika M, Tanaka T, Ishihara M, Okuno N, Hieda N, Yoshida T, Niwa Y (2016) Endoscopic ultrasonography-guided biliary drainage: who, when, which, and how? World J Gastroenterol 22:1297–1303
Kumta NA, Torres-Ruiz F, Reinoso PJ, Kahaleh M (2016) Endoscopic management of hepatic abscess after EUS-guided hepaticogastrostomy. Gastrointest Endosc 84:1054–1055
Ogura T, Okuda A, Miyano A, Nishioka N, Higuchi K (2018) Successful treatment for infected biloma after endoscopic ultrasound-guided hepaticogastrostomy using double stent placement technique. Mini-invasive Surg 2:8
Navaneethan U, Lourdusamy D, Gutierrez NG, Zhu X, Vargo JJ, Parsi MA (2017) New approach to decrease post-ERCP adverse events in patients with primary sclerosing cholangitis. Endosc Int Open 5:E710–E717
Navaneethan U, Lourdusamy V, Jegadeesan R, Sanaka MR, Vargo JJ (2015) Su1626 Bile aspiration during ERCP is associated with lower risk of post-ERCP cholangitis: a single center prospective study. Gastrointest Endosc 81:357
Ishiwatari H, Satoh T, Sato J, Fujie S, Kaneko J, Matsubayashi H, Ono H (2019) Bent needle technique as a rescue for bile duct puncture in endoscopic ultrasonography-guided intrahepatic biliary drainage. Endoscopy 51:E103–E104
Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71:446–454
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 315:801–810
Kiriyama S, Kozaka K, Takada T, Strasberg SM, Pitt HA, Gabata T, Hata J, Liau KH, Miura F, Horiguchi A, Liu KH, Su CH, Wada K, Jagannath P, Itoi T, Gouma DJ, Mori Y, Mukai S, Giménez ME, Huang WS, Kim MH, Okamoto K, Belli G, Dervenis C, Chan ACW, Lau WY, Endo I, Gomi H, Yoshida M, Mayumi T, Baron TH, de Santibañes E, Teoh AYB, Hwang TL, Ker CG, Chen MF, Han HS, Yoon YS, Choi IS, Yoon DS, Higuchi R, Kitano S, Inomata M, Deziel DJ, Jonas E, Hirata K, Sumiyama Y, Inui K, Yamamoto M (2018) Tokyo guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci 25:17–30
Imai H, Takenaka M, Omoto S, Kamata K, Miyata T, Minaga K, Yamao K, Sakurai T, Nishida N, Watanabe T, Kitano M, Kudo M (2017) Utility of endoscopic ultrasound-guided hepaticogastrostomy with antegrade stenting for malignant biliary obstruction after failed endoscopic retrograde cholangiopancreatography. Oncology 93:69–75
Park DH, Lee TH, Paik WH, Choi JH, Song TJ, Lee SS, Seo DW, Lee SK, Kim MH (2015) Feasibility and safety of a novel dedicated device for one-step EUS-guided biliary drainage: a randomized trial. J Gastroenterol Hepatol 30:1461–1466
Chandra S, Klair JS, Soota K, Livorsi DJ, Johlin FC (2019) Endoscopic retrograde cholangio-pancreatography-obtained bile culture can guide antibiotic therapy in acute cholangitis. Dig Dis 37:155–160
Gomi H, Solomkin JS, Schlossberg D, Okamoto K, Takada T, Strasberg SM, Ukai T, Endo I, Iwashita Y, Hibi T, Pitt HA, Matsunaga N, Takamori Y, Umezawa A, Asai K, Suzuki K, Han HS, Hwang TL, Mori Y, Yoon YS, Huang WS, Belli G, Dervenis C, Yokoe M, Kiriyama S, Itoi T, Jagannath P, Garden OJ, Miura F, de Santibañes E, Shikata S, Noguchi Y, Wada K, Honda G, Supe AN, Yoshida M, Mayumi T, Gouma DJ, Deziel DJ, Liau KH, Chen MF, Liu KH, Su CH, Chan ACW, Yoon DS, Choi IS, Jonas E, Chen XP, Fan ST, Ker CG, Giménez ME, Kitano S, Inomata M, Mukai S, Higuchi R, Hirata K, Inui K, Sumiyama Y, Yamamoto M (2018) Tokyo Guidelines 2018: antimicrobial therapy for acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 25:3–16
Yamamoto Y, Ogura T, Nishioka N, Yamada T, Yamada M, Ueno S, Higuchi K (2020) Risks factors for adverse events associated with bile leak during EUS-guided hepaticogastrostomy. Endosc Ultrasound 9:110–115
Davidson B, Varsamidakis N, Dooley J, Deery A, Dick R, Kurzawinski T, Hobbs K (1992) Value of exfoliative cytology for investigating bile duct strictures. Gut 33:1408–1411
Sugiyama M, Atomi Y, Wada N, Kuroda A, Muto T (1996) Endoscopic transpapillary bile duct biopsy without sphincterotomy for diagnosing biliary strictures: a prospective comparative study with bile and brush cytology. Am J Gastroenterol 91:465–467
Iwashita T, Doi S, Yasuda I (2014) Endoscopic ultrasound-guided biliary drainage: a review. Am J Gastroenterol 7:94–102
Acknowledgements
We thank all members of the Division of Endoscopy, Shizuoka Cancer Center, for help rendered with this study.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Hirotoshi Ishiwatari, Tatsunori Satoh, Junya Sato, Junichi Kaneko, Hiroyuki Matsubayashi, Yohei Yabuuchi, Yoshihiro Kishida, Masao Yoshida, Sayo Ito, Noboru Kawata, Kenichiro Imai, Kohei Takizawa, Kinichi Hotta, and Hiroyuki Ono have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ishiwatari, H., Satoh, T., Sato, J. et al. Bile aspiration during EUS-guided hepaticogastrostomy is associated with lower risk of postprocedural adverse events: a retrospective single-center study. Surg Endosc 35, 6836–6845 (2021). https://doi.org/10.1007/s00464-020-08189-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08189-w