Abstract
Background
Controversy exists regarding the safety and effectiveness of minimally invasive inguinal hernia repairs in patients with a history of prior urologic pelvic operations (PUPO), such as a prostatectomy, which causes scarring and disruption of the retropubic tissue planes. Our study sought to examine whether a history of PUPO impacts surgical outcomes in males undergoing robotic-assisted inguinal hernia repair.
Methods
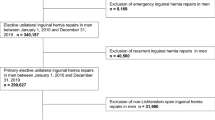
The Americas Hernia Society Quality Collaborative (AHSQC) database was queried to identify male patients who underwent a robotic inguinal hernia repair with 30-day follow-up. A sub-query was performed to identify subjects within the cohort with a documented history of PUPO. Propensity score matching was subsequently utilized to evaluate for differences in intra-operative complications and short-term post-operative outcomes.
Results
In total, 1664 male patients underwent robotic-assisted inguinal hernia repair, of whom 65 (3.9%) had a PUPO. After a 3:1 propensity score matching with hernia repair patients who did not have prior procedures, 195 (11.7%) males were included in the comparison cohort. There were no documented vascular, bladder, or spermatic cord injuries in either group. There was no difference in 30-day readmission rate (5% vs. 3%, respectively, p = 0.41). No hernia recurrences were recorded within the 30-day follow-up period in either group. There was no statistical difference in post-operative complications (including seroma formation, hematoma, and surgical site occurrences) between the two groups (14% vs. 8%, p = 0.18).
Conclusions
In an experienced surgeon’s hands, robotic-assisted minimally invasive inguinal hernia repair may be an alternative to open repair in patients with PUPO who were previously thought to be poor minimally invasive surgical candidates.
Similar content being viewed by others
References
Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362:1561–1571
Trevisonno M, Kaneva P, Watanabe Y et al (2015) A survey of general surgeons regarding laparoscopic inguinal hernia repair: practice patterns, barriers, and educational needs. Hernia 19:719–724
Group H (2018) International guidelines for groin hernia management. Hernia 22:1–165
Gamagami R, Dickens E, Gonzalez A et al (2018) Open versus robotic-assisted transabdominal preperitoneal (R-TAPP) inguinal hernia repair: a multicenter matched analysis of clinical outcomes. Hernia 22:827–836
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70:7–30
Nilsson H, Stranne J, Stattin P, Nordin P (2014) Incidence of groin hernia repair after radical prostatectomy: a population-based nationwide study. Ann Surg 259:1223–1227
Yamada Y, Fujimura T, Fukuhara H et al (2017) Incidence and risk factors of inguinal hernia after robot-assisted radical prostatectomy. World J Surg Oncol 15:61
Zhu S, Zhang H, Xie L, Chen J, Niu Y (2013) Risk factors and prevention of inguinal hernia after radical prostatectomy: a systematic review and meta-analysis. J Urol 189:884–890
Iwamoto H, Morizane S, Hikita K, Honda M, Takenaka A (2019) Postoperative inguinal hernia after robotic-assisted radical prostatectomy for prostate cancer: evaluation of risk factors and recommendation of a convenient prophylactic procedure. Cent European J Urol 72:418–424
Majima T, Yoshino Y, Matsukawa Y et al (2018) Causative factors for de novo inguinal hernia after robot-assisted radical prostatectomy. J Robot Surg 12:277–282
Finley DS, Savatta D, Rodriguez E, Kopelan A, Ahlering TE (2008) Transperitoneal robotic-assisted laparoscopic radical prostatectomy and inguinal herniorrhaphy. J Robot Surg 1:269–272
Rogers T, Parra-Davila E, Malcher F et al (2018) Robotic radical prostatectomy with concomitant repair of inguinal hernia: is it safe? J Robot Surg 12:325–330
Miyajima A (2018) Inseparable interaction of the prostate and inguinal hernia. Int J Urol 25:644–648
Peitsch WKJ (2019) Laparoscopic transperitoneal inguinal hernioplasty (TAPP) after radical open retropubic prostatectomy: special features and clinical outcomes. Hernia 23:281–286
Le Page P, Smialkowski A, Morton J, Fenton-Lee D (2013) Totally extraperitoneal inguinal hernia repair in patients previously having prostatectomy is feasible, safe, and effective. Surg Endosc 27:4485–4490
Dulucq JL, Wintringer P, Mahajna A (2006) Totally extraperitoneal (TEP) hernia repair after radical prostatectomy or previous lower abdominal surgery: is it safe? A prospective study. Surg Endosc 20:473–476
Prassas D, Ntolia A, Brosa J et al (2019) Effect of previous lower abdominal surgery on outcomes following totally extraperitoneal (TEP) inguinal hernia repair. Surg Laparosc Endosc Percutan Tech 29:267–270
Wauschkuhn CA, Schwarz J, Bittner R (2009) Laparoscopic transperitoneal inguinal hernia repair (TAPP) after radical prostatectomy: is it safe? Results of prospectively collected data of more than 200 cases. Surg Endosc 23:973–977
Sakon M, Sekino Y, Okada M, Seki H, Munakata Y (2017) Laparoscopic inguinal hernioplasty after robot-assisted laparoscopic radical prostatectomy. Hernia 21:745–748
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Anthony Iacco serves as a proctoring consultant for Intuitive Surgical, Inc. Andrew Angus and Alexander DeMare have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Angus, A., DeMare, A. & Iacco, A. Evaluating outcomes for robotic-assisted inguinal hernia repair in males with prior urologic surgery: a propensity-matched analysis from a national database. Surg Endosc 35, 5310–5314 (2021). https://doi.org/10.1007/s00464-020-08020-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08020-6