Abstract
Background
Gastric cancer perforation is rare and difficult to distinguish from gastric ulcer perforation before surgery. Peritonitis caused by gastric perforation requires emergency surgery. The optimal surgical strategy for gastric perforation has not been established.
Material and methods
Data from 43 patients who underwent primary gastrectomy with curative intent for gastric perforation between June 2010 and November 2019 were reviewed. Patients were classified into gastric ulcer and gastric cancer groups. Early surgical outcomes and overall survival were assessed.
Results
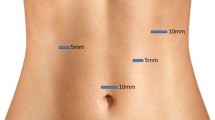
There were no significant differences in clinical characteristics between the two groups except regarding preoperative shock. Laparoscopic gastrectomy was performed in 35 of 43 patients. There were no conversions to open surgery. The surgical findings demonstrated that the gastric cancer group had larger mass lesions with significantly larger perforations than did the gastric ulcer group. There were no significant differences in early surgical outcomes. Severe postoperative complications occurred in nine patients, five of whom died within one month of surgery. The majority of patients (90%) had stage III or IV gastric cancer. The 5-year survival rate was 19.5%.
Conclusion
We found no definitive differences in clinical characteristics distinguishing gastric cancer from ulcers. Considering our surgical outcomes, laparoscopic primary gastrectomy performed by an expert is a useful technique for emergency gastric perforation. However, unless an expert is available, caution should be used when selecting laparoscopic primary gastrectomy with curative intent as a surgical method.

Similar content being viewed by others
References
Hata T, Sakata N, Kudoh K, Shibata C, Unno M (2014) The best surgical approach for perforated gastric cancer: one-stage vs. two-stage gastrectomy. Gastric Cancer 17:578–587
Roviello F, Rossi S, Marrelli D, De Manzoni G, Pedrazzani C, Morgagni P, Corso G, Pinto E (2006) Perforated gastric carcinoma: a report of 10 cases and review of the literature. World J Surg Oncol 4:19
Ozmen MM, Zulfikaroglu B, Kece C, Aslar AK, Ozalp N, Koc M (2002) Factors influencing mortality in spontaneous gastric tumour perforations. J Int Med Res 30:180–184
Mahar AL, Brar SS, Coburn NG, Law C, Helyer LK (2012) Surgical management of gastric perforation in the setting of gastric cancer. Gastric Cancer 15(Suppl 1):S146–152
Moller MH, Adamsen S, Thomsen RW, Moller AM, Peptic Ulcer Perforation trial g (2011) Multicentre trial of a perioperative protocol to reduce mortality in patients with peptic ulcer perforation. Br J Surg 98:802–810
So JB, Yam A, Cheah WK, Kum CK, Goh PM (2000) Risk factors related to operative mortality and morbidity in patients undergoing emergency gastrectomy. Br J Surg 87:1702–1707
Adachi Y, Mori M, Maehara Y, Matsumata T, Okudaira Y, Sugimachi K (1997) Surgical results of perforated gastric carcinoma: an analysis of 155 Japanese patients. Am J Gastroenterol 92:516–518
Jwo SC, Chien RN, Chao TC, Chen HY, Lin CY (2005) Clinicopathological features, surgical management, and disease outcome of perforated gastric cancer. J Surg Oncol 91:219–225
Kim HI, Kim MG (2015) Entirely laparoscopic gastrectomy and colectomy for remnant gastric cancer with gastric outlet obstruction and transverse colon invasion. J Gastric Cancer 15:286–289
Kim MG (2015) Laparoscopic surgery for perforated duodenal ulcer disease: analysis of 70 consecutive cases from a single surgeon. Surg Laparosc Endosc Percutan Tech 25:331–336
Ma CH, Kim MG (2012) Laparoscopic primary repair with omentopexy for duodenal ulcer perforation: a single institution experience of 21 cases. J Gastric Cancer 12:237–242
Kim MG, Park HK, Park JJ, Lee HG, Nam YS (2012) The applicability of laparoscopic gastrectomy in the surgical treatment of giant duodenal ulcer perforation. Surg Laparosc Endosc Percutan Tech 22:122–126
Kim MG, Kim KC, Yook JH, Kim BS, Kim TH, Kim BS (2011) A practical way to overcome the learning period of laparoscopic gastrectomy for gastric cancer. Surg Endosc 25:3838–3844
Japanese Gastric Cancer A (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14:113–123
V AM, C PM, S S, Srinivasarangan M (2014) Efficacy of Mannheim peritonitis index (MPI) score in patients with secondary peritonitis. J Clin Diagn Res 8:NC01–03
Clavien PA, Strasberg SM (2009) Severity grading of surgical complications. Ann Surg 250:197–198
Kasakura Y, Ajani JA, Mochizuki F, Morishita Y, Fujii M, Takayama T (2002) Outcomes after emergency surgery for gastric perforation or severe bleeding in patients with gastric cancer. J Surg Oncol 80:181–185
Kasakura Y, Ajani JA, Fujii M, Mochizuki F, Takayama T (2002) Management of perforated gastric carcinoma: a report of 16 cases and review of world literature. Am Surg 68:434–440
Lehnert T, Buhl K, Dueck M, Hinz U, Herfarth C (2000) Two-stage radical gastrectomy for perforated gastric cancer. Eur J Surg Oncol 26:780–784
Kandel BP, Singh Y, Singh KP, Khakurel M (2013) Gastric cancer perforation: experience from a tertiary care hospital. JNMA J Nepal Med Assoc 52:489–493
Kirshtein B, Bayme M, Mayer T, Lantsberg L, Avinoach E, Mizrahi S (2005) Laparoscopic treatment of gastroduodenal perforations: comparison with conventional surgery. Surg Endosc 19:1487–1490
Kotan C, Sumer A, Baser M, Kiziltan R, Carparlar MA (2008) An analysis of 13 patients with perforated gastric carcinoma: A surgeon's nightmare? World J Emerg Surg 3:17
Orsenigo E, Tomajer V, Palo SD, Carlucci M, Vignali A, Tamburini A, Staudacher C (2007) Impact of age on postoperative outcomes in 1118 gastric cancer patients undergoing surgical treatment. Gastric Cancer 10:39–44
Ergul E, Gozetlik EO (2009) Emergency spontaneous gastric perforations: ulcus versus cancer. Langenbecks Arch Surg 394:643–646
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
None of the authors (Hyung Suk Kim, Jun Ho Lee, or Min Gyu Kim) has any conflicts of interest or financial ties to disclose.
Ethical approval
Approval was obtained from the Institutional Review Board of Hanyang University Guri Hospital of Korea, College of Medicine.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, H.S., Lee, J.H. & Kim, M.G. Outcomes of laparoscopic primary gastrectomy with curative intent for gastric perforation: experience from a single surgeon. Surg Endosc 35, 4206–4213 (2021). https://doi.org/10.1007/s00464-020-07902-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07902-z