Abstract
Background
The prevalence of smoking among patients undergoing bariatric surgery has been reported to be as high as 40%. The effect of smoking in the perioperative period has been extensively studied for various surgical procedures, but limited data are available for bariatric surgery. The objective of this study is to review the existing literature to assess: (1) the impact of smoking on postoperative morbidity and mortality after bariatric surgery, (2) the relationship between smoking and weight loss after bariatric surgery, and (3) the efficacy of smoking cessation in the perioperative period among bariatric surgery patients.
Methods
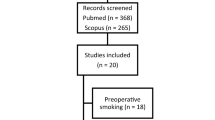
A comprehensive search of electronic databases including MEDLINE, EMBASE and the Cochrane Library from 1946 to February 2020 was performed to identify relevant articles. Following an initial screen of 940 titles and abstracts, 540 full articles were reviewed.
Results
Forty-eight studies met criteria for analysis: five structured interviews, three longitudinal studies, thirty-two retrospective studies and eight prospective studies. Smoking within 1 year prior to bariatric surgery was found to be an independent risk factor for increased 30-day mortality and major postoperative complications, particularly wound and pulmonary complications. Smoking was significantly associated with long-term complications including marginal ulceration and bone fracture. Smoking has little to no effect on weight loss following bariatric surgery, with studies reporting at most a 3% increased percentage excess weight loss. Rates of smoking recidivism are high with studies reporting that up to 17% of patients continue to smoke postoperatively.
Conclusions
Although current best practice guidelines recommend only a minimum of 6 weeks of abstinence from smoking prior to bariatric surgery, the findings of this review suggest that smoking within 1 year prior to bariatric surgery is associated with significant postoperative morbidity. More investigation is needed on strategies to improve smoking cessation compliance among bariatric surgery patients in the perioperative period.

Similar content being viewed by others
References
Gloy VL, Briel M, Bhatt DL, Kashyap SR, Schauer PR, Mingrone G, Nordmann AJ (2013) Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ 347:f5934. https://doi.org/10.1136/bmj.f5934
Angrisani L, Santonicola A, Iovino P, Vitiello A, Zundel N, Buchwald H, Scopinaro N (2017) Bariatric surgery and endoluminal procedures: IFSO worldwide survey 2014. Obes Surg 27(9):2279–2289
Flum DR, Belle SH, King WC, Wahed AS, Berk P, Chapman W, Longitudinal Assessment of Bariatric Surgery (LABS) Consortium (2009) Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med 361(5):445–454
Li JF, Lai DD, Lin ZH, Jiang TY, Zhang AM, Dai JF (2014) Comparison of the long-term results of Roux-en-Y gastric bypass and sleeve gastrectomy for morbid obesity: a systematic review and meta-analysis of randomized and nonrandomized trials. Surg Laparosc Endosc Percutan Tech 24(1):1–11
Finks JF, Kole KL, Yenumula PR, English WJ, Krause KR, Carlin AM (2011) Predicting risk for serious complications with bariatric surgery: results from the Michigan Bariatric Surgery Collaborative. Ann Surg 254(4):633–640
Schumann R, Jones SB, Cooper B, Kelley SD, Bosch MV, Ortiz VE, Carr DB (2009) Update on best practice recommendations for anesthetic perioperative care and pain management in weight loss surgery, 2004–2007. Obesity (Silver Spring) 17(5):889–894
Mechanick JI, Youdim A, Jones DB, Garvey WT, Hurley DL, McMahon MM (2013) Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient–2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocr Pract 19(2):337–372
Myers K, Hajek P, Hinds C, McRobbie H (2011) Stopping smoking shortly before surgery and postoperative complications: a systematic review and meta-analysis. Arch Intern Med 171(11):983–989
Mills E, Eyawo O, Lockhart I, Kelly S, Wu P, Ebbert JO (2011) Smoking cessation reduces postoperative complications: a systematic review and meta-analysis. Am J Med 124(2):144–154
Møller AM, Villebro N, Pedersen T, Tønnesen H (2002) Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet 359(9301):114–117
Wong J, Lam DP, Abrishami A, Chan MT, Chung F (2012) Short-term preoperative smoking cessation and postoperative complications: a systematic review and meta-analysis. Can J Anaesth 59(3):268–279
Adams CE, Gabriele JM, Baillie LE, Dubbert PM (2012) Tobacco use and substance use disorders as predictors of postoperative weight loss 2 years after bariatric surgery. J Behav Health Serv Res 39(4):462–471
Latner JD, Wetzler S, Goodman ER, Glinski J (2004) Gastric bypass in a low-income, inner-city population: eating disturbances and weight loss. Obes Res 12(6):956–961
Lent MR, Hayes SM, Wood GC, Napolitano MA, Argyropoulos G, Gerhard GS, Still CD (2013) Smoking and alcohol use in gastric bypass patients. Eat Behav 14(4):460–463
Conason A, Teixeira J, Hsu CH, Puma L, Knafo D, Geliebter A (2013) Substance use following bariatric weight loss surgery. JAMA Surg 148(2):145–150
Gribsholt SB, Pedersen AM, Svensson E, Thomsen RW, Richelsen B (2016) Prevalence of self-reported symptoms after gastric bypass surgery for obesity. JAMA Surg 151(6):504–511
Tae B, Pelaggi ER, Moreira JG, Waisberg J, de Matos LL, D'Elia G (2014) Impact of bariatric surgery on depression and anxiety symptons, bulimic behaviors and quality of life. Rev Col Bras Cir 41(3):155–160
Grace DM, Pederson L, Speechley KN, McAlpine D (1990) A longitudinal study of smoking status and weight loss following gastroplasty in a group of morbidly obese patients. Int J Obes 14(4):311–317
Atilla N, Arpag H, Bozkus F, Kahraman H, Cengiz E, Bulbuloglu E, Atilla S (2017) Can we predict the perioperative pulmonary complications before laparoscopic sleeve gastrectomy: original research. Obes Surg 27(6):1524–1528
Arterburn D, Livingston EH, Schifftner T, Kahwati LC, Henderson WG, Maciejewski ML (2009) Predictors of long-term mortality after bariatric surgery performed in Veterans Affairs medical centers. Arch Surg 144(10):914–920
Arterburn D, Livingston EH, Olsen MK, Smith VA, Kavee AL, Kahwati LC, Maciejewski ML (2013) Predictors of initial weight loss after gastric bypass surgery in twelve Veterans Affairs Medical Centers. Obes Res Clin Pract 7(5):e367–376
Inadomi M, Iyengar R, Fischer I, Chen X, Flagler E, Ghaferi AA (2018) Effect of patient-reported smoking status on short-term bariatric surgery outcomes. Surg Endosc 32(2):720–726
Kowalewski PK, Olszewski R, Walędziak MS, Janik MR, Kwiatkowski A, Paśnik K (2018) Cigarette smoking and its impact on weight loss after bariatric surgery: a single center, retrospective study. Surg Obes Relat Dis 14(8):1163–1166
Moser F, Signorini FJ, Maldonado PS, Lopez Sivilat A, Gorodner V, Viscido G, Obeide LR (2016) Relationship between tobacco use and weight loss after bariatric surgery. Obes Surg 26(8):1777–1781
Signorini FJ, Polero V, Viscido G, Navarro L, Obeide L, Moser F (2018) Long-term relationship between tobacco use and weight loss after sleeve gastrectomy. Obes Surg 28(9):2644–2649
Wood GC, Benotti PN, Lee CJ, Mirshahi T, Still CD, Gerhard GS, Lent MR (2016) Evaluation of the association between preoperative clinical factors and long-term weight loss after Roux-en-Y gastric bypass. JAMA Surg 151(11):1056–1062
Zhang W, Mason EE, Renquist KE, Zimmerman MB, Contributors I (2005) Factors influencing survival following surgical treatment of obesity. Obes Surg 15(1):43–50
Yuce TK, Khorfan R, Soper NJ, Hungness ES, Nagle AP, Teitelbaum EN, Odell DD (2019) Post-operative complications and readmissions associated with smoking following bariatric surgery. J Gastrointest Surg. https://doi.org/10.1007/s11605-019-04488-3
Kovacs Z, Valentin JB, Nielsen RE (2017) Risk of psychiatric disorders, self-harm behaviour and service use associated with bariatric surgery. Acta Psychiatr Scand 135(2):149–158
Altieri MS, Pryor A, Yang J, Yin D, Docimo S, Bates A, Spaniolas K (2018) The natural history of perforated marginal ulcers after gastric bypass surgery. Surg Endosc 32(3):1215–1222
Azagury DE, Abu Dayyeh BK, Greenwalt IT, Thompson CC (2011) Marginal ulceration after Roux-en-Y gastric bypass surgery: characteristics, risk factors, treatment, and outcomes. Endoscopy 43(11):950–954
Benotti P, Wood GC, Winegar DA, Petrick AT, Still CD, Argyropoulos G, Gerhard GS (2014) Risk factors associated with mortality after Roux-en-Y gastric bypass surgery. Ann Surg 259(1):123–130
Dittrich L, Schwenninger MV, Dittrich K, Pratschke J, Aigner F, Raakow J (2019) Marginal ulcers after laparoscopic Roux-en-Y gastric bypass: analysis of the amount of daily and lifetime smoking on postoperative risk. Surg Obes Relat Dis. https://doi.org/10.1016/j.soard.2019.11.022
El-Hayek K, Timratana P, Shimizu H, Chand B (2012) Marginal ulcer after Roux-en-Y gastric bypass: what have we really learned? Surg Endosc 26(10):2789–2796
Fashandi AZ, Mehaffey JH, Hawkins RB, Schirmer B, Hallowell PT (2018) Bariatric surgery increases risk of bone fracture. Surg Endosc 32(6):2650–2655
Gonzalez R, Haines K, Nelson LG, Gallagher SF, Murr MM (2006) Predictive factors of thromboembolic events in patients undergoing Roux-en-Y gastric bypass. Surg Obes Relat Dis 2(1):30–35 discussion 35-36
Gupta PK, Franck C, Miller WJ, Gupta H, Forse RA (2011) Development and validation of a bariatric surgery morbidity risk calculator using the prospective, multicenter NSQIP dataset. J Am Coll Surg 212(3):301–309
Gupta PK, Gupta H, Kaushik M, Fang X, Miller WJ, Morrow LE, Armour-Forse R (2012) Predictors of pulmonary complications after bariatric surgery. Surg Obes Relat Dis 8(5):574–581
Haskins IN, Amdur R, Vaziri K (2014) The effect of smoking on bariatric surgical outcomes. Surg Endosc 28(11):3074–3080
Haskins IN, Nowacki AS, Khorgami Z, Schulz K, Heinberg LJ, Schauer PR, Aminian A (2017) Should recent smoking be a contraindication for sleeve gastrectomy? Surg Obes Relat Dis 13(7):1130–1135
Lautz DB, Jackson TD, Clancy KA, Escareno CE, Schifftner T, Henderson WG, Khuri S (2007) Bariatric operations in Veterans Affairs and selected university medical centers: results of the patient safety in surgery study. J Am Coll Surg 204(6):1261–1272
Livingston EH, Huerta S, Arthur D, Lee S, De Shields S, Heber D (2002) Male gender is a predictor of morbidity and age a predictor of mortality for patients undergoing gastric bypass surgery. Ann Surg 236(5):576–582
Livingston EH, Arterburn D, Schifftner TL, Henderson WG, DePalma RG (2006) National Surgical Quality Improvement Program analysis of bariatric operations: modifiable risk factors contribute to bariatric surgical adverse outcomes. J Am Coll Surg 203(5):625–633
Major P, Wysocki M, Torbicz G, Gajewska N, Dudek A, Małczak P, Budzyński A (2018) Risk factors for prolonged length of hospital stay and readmissions after laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass. Obes Surg 28(2):323–332
Marchini JF, Souza FL, Schmidt A, Cunha SF, Salgado W, Marchini JS, Santos JE (2012) Low educational status, smoking, and multidisciplinary team experience predict hospital length of stay after bariatric surgery. Nutr Metab Insights 5:71–76
Moon RC, Ghanem M, Teixeira AF, De La Cruz-Munoz N, Young MK, Domkowski P, Jawad MA (2018) Assessing risk factors, presentation, and management of portomesenteric vein thrombosis after sleeve gastrectomy: a multicenter case-control study. Surg Obes Relat Dis 14(4):478–483
Nguyen NT, Rivers R, Wolfe BM (2003) Factors associated with operative outcomes in laparoscopic gastric bypass. J Am Coll Surg 197(4):548–555 discussion 555-547
Turner PL, Saager L, Dalton J, Abd-Elsayed A, Roberman D, Melara P, Turan A (2011) A nomogram for predicting surgical complications in bariatric surgery patients. Obes Surg 21(5):655–662
Wilson JA, Romagnuolo J, Byrne TK, Morgan K, Wilson FA (2006) Predictors of endoscopic findings after Roux-en-Y gastric bypass. Am J Gastroenterol 101(10):2194–2199
Spaniolas K, Yang J, Crowley S, Yin D, Docimo S, Bates AT, Pryor AD (2018) Association of long-term anastomotic ulceration after Roux-en-Y gastric bypass with tobacco smoking. JAMA Surg 153(9):862–864
Andersen JR, Aadland E, Nilsen RM, Våge V (2014) Predictors of weight loss are different in men and women after sleeve gastrectomy. Obes Surg 24(4):594–598
Courcoulas AP, Christian NJ, O'Rourke RW, Dakin G, Patchen Dellinger E, Flum DR, Belle SH (2015) Preoperative factors and 3-year weight change in the Longitudinal Assessment of Bariatric Surgery (LABS) consortium. Surg Obes Relat Dis 11(5):1109–1118
King WC, Belle SH, Hinerman AS, Mitchell JE, Steffen KJ, Courcoulas AP (2019) Patient behaviors and characteristics related to weight regain after Roux-en-Y gastric bypass: a multicenter prospective cohort study. Ann Surg. https://doi.org/10.1097/SLA.0000000000003281
Parri A, Benaiges D, Schröder H, Izquierdo-Pulido M, Ramón J, Villatoro M, Goday A (2015) Preoperative predictors of weight loss at 4 years following bariatric surgery. Nutr Clin Pract 30(3):420–424
Still CD, Wood GC, Chu X, Manney C, Strodel W, Petrick A, Gerhard GS (2014) Clinical factors associated with weight loss outcomes after Roux-en-Y gastric bypass surgery. Obesity (Silver Spring) 22(3):888–894
Cena H, De Giuseppe R, Biino G, Persico F, Ciliberto A, Giovanelli A, Stanford FC (2016) Evaluation of eating habits and lifestyle in patients with obesity before and after bariatric surgery: a single Italian center experience. Springerplus 5(1):1467
Maniscalco M, Carratù P, Faraone S, Cerbone MR, Cristiano S, Zedda A, Resta O (2015) Smoking habit in severe obese after bariatric procedures. Tob Induc Dis 13(1):20
King WC, White GE, Belle SH, Yanovski SZ, Pomp A, Pories WJ, Courcoulas AP (2020) Changes in smoking behavior before and after gastric bypass: a 7-year study. Ann Surg. https://doi.org/10.1097/SLA.0000000000003828
Buchwald H, Oien DM (2013) Metabolic/bariatric surgery worldwide 2011. Obes Surg 23(4):427–436
English WJ, DeMaria EJ, Brethauer SA, Mattar SG, Rosenthal RJ, Morton JM (2018) American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis 14(3):259–263
Young MT, Gebhart A, Phelan MJ, Nguyen NT (2015) Use and outcomes of laparoscopic sleeve gastrectomy vs laparoscopic gastric bypass: analysis of the American College of Surgeons NSQIP. J Am Coll Surg 220(5):880–885
Levine MD, Kalarchian MA, Courcoulas AP, Wisinski MS, Marcus MD (2007) History of smoking and postcessation weight gain among weight loss surgery candidates. Addict Behav 32(10):2365–2371
Spadola CE, Wagner EF, Dillon FR, Trepka MJ, De La Cruz-Munoz N, Messiah SE (2015) Alcohol and drug use among postoperative bariatric patients: a systematic review of the emerging research and Its implications. Alcohol Clin Exp Res 39(9):1582–1601
King WC, Chen JY, Mitchell JE, Kalarchian MA, Steffen KJ, Engel SG, Yanovski SZ (2012) Prevalence of alcohol use disorders before and after bariatric surgery. JAMA 307(23):2516–2525
King WC, Chen JY, Courcoulas AP, Dakin GF, Engel SG, Flum DR, Yanovski SZ (2017) Alcohol and other substance use after bariatric surgery: prospective evidence from a U.S. multicenter cohort study. Surg Obes Relat Dis 13(8):1392–1402
Li L, Wu LT (2016) Substance use after bariatric surgery: a review. J Psychiatr Res 76:16–29
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Alexandra Chow, Amy Neville and Nicole Kolozsvari have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chow, A., Neville, A. & Kolozsvari, N. Smoking in bariatric surgery: a systematic review. Surg Endosc 35, 3047–3066 (2021). https://doi.org/10.1007/s00464-020-07669-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07669-3