Abstract
Background
Minimally invasive approach has been increasingly applied in liver resection. However, laparoscopic major hepatectomy is technically demanding and is practiced only in expert centers around the world. Conversely, use of robot may help to overcome the difficulty and facilitate major hepatectomy.
Methods
Between September 2010 and March 2019, 151 patients received robotic hepatectomy for various indications in our center. 36 patients received robotic hemihepatectomy: 26 left hepatectomy and 10 right hepatectomy. During the same period, 737 patients received open hepatectomy and out of these, 173 patients received open hemihepatectomy. A propensity score-matched analysis was performed in a 1:1 ratio.
Results
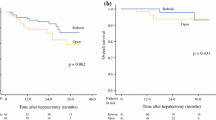
After matching, there were 36 patients each in the robotic and open group. The two groups were comparable in demographic data, type of hemihepatectomy, underlying pathology, size of tumor, and background cirrhosis. Conversion was needed in 3 patients (8.3%) in the robotic group. There was no operative mortality. The operative blood loss and resection margin were similar. Though not significantly different, there was a higher rate of complications in the robotic group (36.1% vs. 22.2%) and this difference was mostly driven by higher intra-abdominal collection (16.7% vs. 5.6%) and bile leak (5.6% vs. 2.8%). Operative time was significantly longer (400.8 ± 136.1 min vs 255.4 ± 74.4 min, P < 0.001) but the postoperative hospital stay was significantly shorter (median 5 days vs 6.5 days, P = 0.040) in the robotic group. When right and left hepatectomy were analyzed separately, the advantage of shorter hospital stay remained in left but not right hepatectomy. For patients with hepatocellular carcinoma, there was no difference between the two groups in 5-year overall and disease-free survival.
Conclusion
Compared with the open approach, robotic hemihepatectomy has longer operation time but shorter hospital stay. Thus, use of robot is feasible and effective in hemihepatectomy with the benefit of shorter hospital stay.

Similar content being viewed by others
References
Reich H, McGlynn F, DeCaprio J, Budin R (1991) Laparoscopic excision of benign liver lesions. Obstet Gynecol 78(5 Pt 2):956–958
Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker CG, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D'Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey JN, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil R, Belghiti J, Strasberg S, Chari RS; World Consensus Conference on Laparoscopic Surgery (2009) The international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann Surg 250:825–830
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, O-rourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schön MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J, Strasberg SM (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261:619–629
Tsung A, Geller DA, Sukato DC, Sabbaghian S, Tohme S, Steel J, Marsh W, Reddy SK, Bartlett DL (2014) Robotic versus laparoscopic hepatectomy: a matched comparison. Ann Surg 259:549–555
Lee KF, Cheung YS, Chong CC, Wong J, Fong AK, Lai PB (2016) Laparoscopic and robotic hepatectomy: experience from a single centre. ANZ J Surg 86:122–126
Strasberg SM (2005) Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg 12:351–355
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Patriti A, Cipriani F, Ratti F, Bartoli A, Ceccarelli G, Casciola L, Aldrighetti L (2014) Robot-assisted versus open liver resection in the right posterior section. JSLS 18(e2014):00040
Croner RS, Perrakis A, Hohenberger W, Brunner M (2016) Robotic liver surgery for minor hepatic resections: a comparison with laparoscopic and open standard procedures. Langenbecks Arch Surg 401:707–714
Morel P, Jung M, Cornateanu S, Buehler L, Majno P, Toso C, Buchs NC, Rubbia-Brandt L, Hagen ME (2017) Robotic versus open liver resections: a case-matched comparison. Int J Med Robot 13:e1800
Nota CL, Woo Y, Raoof M, Boerner T, Molenaar IQ, Choi GH, Kingham TP, Latorre K, Borel Rinkes IHM, Hagendoorn J, Fong Y (2019) Robotic versus open minor liver resections of the posterosuperior segments: a multinational. Propensity Score-Matched Study Ann Surg Oncol 26:583–590
Kingham TP, Leung U, Kuk D, Gönen M, D'Angelica MI, Allen PJ, DeMatteo RP, Laudone VP, Jarnagin WR, Fong Y (2016) Robotic liver resection: a case-matched comparison. World J Surg 40:1422–1428
Sham JG, Richards MK, Seo YD, Pillarisetty VG, Yeung RS, Park JO (2016) Efficacy and cost of robotic hepatectomy: is the robot cost-prohibitive? J Robot Surg 10:307–313
Daskalaki D, Gonzalez-Heredia R, Brown M, Bianco FM, Tzvetanov I, Davis M, Kim J, Benedetti E, Giulianotti PC (2017) Financial impact of the robotic approach in liver surgery: a comparative study of clinical outcomes and costs between the robotic and open technique in a single institution. J Laparoendosc Adv Surg Tech A 27:375–382
Chen PD, Wu CY, Hu RH, Chou WH, Lai HS, Liang JT, Lee PH, Wu YM (2017) Robotic Versus Open Hepatectomy for hepatocellular carcinoma: a matched comparison. Ann Surg Oncol 24:1021–1028
Wang WH, Kuo KK, Wang SN, Lee KT (2018) Oncological and surgical result of hepatoma after robot surgery. Surg Endosc 32:3918–3924
Wong DJ, Wong MJ, Choi GH, Wu YM, Lai PB, Goh BKP (2019) Systematic review and meta-analysis of robotic versus open hepatectomy. ANZ J Surg 89:165–170
Lee KF, Cheung YS, Wong J, Chong CC, Wong JS, Lai PB (2012) Randomized clinical trial of open hepatectomy with or without intermittent Pringle manoeuvre. Br J Surg 99:1203–1209
Nota CL, Rinkes IHB, Molenaar IQ, van Santvoort HC, Fong Y, Hagendoorn J (2016) Robot-assisted laparoscopic liver resection: a systematic review and pooled analysis of minor and major hepatectomies. HPB (Oxford) 18:113–120
Chen PD, Wu CY, Hu RH, Chen CN, Yuan RH, Liang JT, Lai HS, Wu YM (2017) Robotic major hepatectomy: is there a learning curve? Surgery 161:642–649
Abu Hilal M, Aldrighetti L, Dagher I, Edwin B, Troisi RI, Alikhanov R, Aroori S, Belli G, Besselink M, Briceno J, Gayet B, D'Hondt M, Lesurtel M, Menon K, Lodge P, Rotellar F, Santoyo J, Scatton O, Soubrane O, Sutcliffe R, Van Dam R, White S, Halls MC, Cipriani F, Van der Poel M, Ciria R, Barkhatov L, Gomez-Luque Y, Ocana-Garcia S, Cook A, Buell J, Clavien PA, Dervenis C, Fusai G, Geller D, Lang H, Primrose J, Taylor M, Van Gulik T, Wakabayashi G, Asbun H, Cherqui D (2018) The Southampton Consensus Guidelines for laparoscopic liver surgery: from indication to implementation. Ann Surg 268:11–18
Acknowledgements
The authors thank Mr Philip Ip for his assistance with data processing and statistical analysis.
Funding
This study was not supported by any Grant or funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
K.F. Lee, Charing Chong, Sunny Cheung, John Wong, Andrew Fung, H.T. Lok, E. Lo, and Paul Lai have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, Kf., Chong, C., Cheung, S. et al. Robotic versus open hemihepatectomy: a propensity score-matched study. Surg Endosc 35, 2316–2323 (2021). https://doi.org/10.1007/s00464-020-07645-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07645-x