Abstract
Background
Bariatric surgery is the most effective long-term treatment for morbid obesity; however, it is under-utilized. This study examines the association between morbid obesity rates, bariatric surgeon presence, and utilization of bariatric surgery in the United States.
Methods
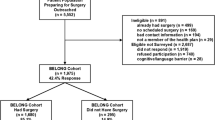
Healthcare Cost and Utilization Project’s 2013 National Inpatient Sample was used to determine the incidence of inpatient bariatric procedures using ICD-9 codes. The Center for Disease Control’s 2013 Behavioral Risk Factor Surveillance System survey was analyzed to determine estimates of bariatric surgery qualified adults, aged 18–70, with BMI ≥ 40 or ≥ 35 with diabetes. The number of bariatric surgeons was determined from four online sources: searches of Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program accredited bariatric programs, American Society for Metabolic and Bariatric Surgery membership, and two adjustable gastric band manufacturer “find a surgeon” search tools. Correlations between rates of morbid obesity, bariatric surgeon presence, and incidence of inpatient bariatric surgery were determined.
Results
The defined bariatric surgery eligible population comprised between 3.6% (New England) to 6.8% (East South Central) of the total division population (p < 0.001). Incident rates of bariatric surgery ranged from 0.9% in East South Central to 2.2% in New England (p < 0.001). 2124 bariatric surgeons were identified. The rate of bariatric surgery by division was negatively correlated with division morbid obesity rates (r = − 0.65) and strongly positively correlated with surgeon presence (r = 0.91). After adjusting for demographic differences between divisions, surgeon presence remained highly associated with surgery utilization (p < 0.001).
Conclusions
Rates of bariatric surgery procedures in the U.S. are minimally correlated with rates of morbid obesity and are strongly correlated with the number of available bariatric surgeons. Effective therapy for the morbidly obese may be limited by the lack of qualified surgeons.




Similar content being viewed by others
References
Sturm R, Hattori A (2013) Morbid obesity rates continue to rise rapidly in the United States. Int J Obes 37:889–891. https://doi.org/10.1038/ijo.2012.159
Sturm R (2003) Increases in clinically severe obesity in the united states, 1986-2000. Arch Intern Med 163:2146–2148. https://doi.org/10.1001/archinte.163.18.2146
Flegal KM, Kit BK, Orpana H, Graubard BI (2013) Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 309:71–82. https://doi.org/10.1001/jama.2012.113905
Haslam DW, James WPT (2005) Obesity. Lancet 366:1197–1209. https://doi.org/10.1016/S0140-6736(05)67483-1
Cawley J, Meyerhoefer C (2012) The medical care costs of obesity: an instrumental variables approach. J Health Econ 31:219–230. https://doi.org/10.1016/j.jhealeco.2011.10.003
Buchwald H, Avidor Y, Braunwald E et al (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737. https://doi.org/10.1001/jama.292.14.1724
Maggard-Gibbons M, Maglione M, Livhits M et al (2013) Bariatric surgery for weight loss and glycemic control in nonmorbidly obese adults with diabetes: a systematic review. JAMA 309:2250–2261. https://doi.org/10.1001/jama.2013.4851
Sjöström L, Peltonen M, Jacobson P et al (2012) Bariatric surgery and long-term cardiovascular events. JAMA 307:56–65. https://doi.org/10.1001/jama.2011.1914
Schauer PR, Bhatt DL, Kirwan JP et al (2014) Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med 370:2002–2013. https://doi.org/10.1056/NEJMoa1401329
Ikramuddin S, Billington CJ, Lee W-J et al (2015) Roux-en-Y gastric bypass for diabetes (the Diabetes Surgery Study): 2-year outcomes of a 5-year, randomised, controlled trial. Lancet Diabetes Endocrinol 3:413–422. https://doi.org/10.1016/S2213-8587(15)00089-3
Mingrone G, Panunzi S, De Gaetano A et al (2015) Bariatric–metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet 386:964–973. https://doi.org/10.1016/S0140-6736(15)00075-6
Arterburn DE, Olsen MK, Smith VA et al (2015) Association between bariatric surgery and long-term survival. JAMA 313:62–70. https://doi.org/10.1001/jama.2014.16968
Sjöström L, Narbro K, Sjöström CD et al (2007) Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 357:741–752. https://doi.org/10.1056/NEJMoa066254
English WJ, DeMaria EJ, Brethauer SA et al (2018) American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis 14:259–263. https://doi.org/10.1016/j.soard.2017.12.013
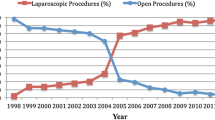
Nguyen NT, Masoomi H, Magno CP et al (2011) Trends in use of bariatric surgery, 2003–2008. J Am Coll Surg 213:261–266. https://doi.org/10.1016/j.jamcollsurg.2011.04.030
Nguyen NT, Vu S, Kim E et al (2016) Trends in utilization of bariatric surgery, 2009–2012. Surg Endosc 30:2723–2727. https://doi.org/10.1007/s00464-015-4535-9
Flum DR, Khan TV, Dellinger EP (2007) Toward the rational and equitable use of bariatric surgery. JAMA 298:1442–1444. https://doi.org/10.1001/jama.298.12.1442
Poulose BK, Holzman MD, Zhu Y et al (2005) National variations in morbid obesity and bariatric surgery use. J Am Coll Surg 201:77–84. https://doi.org/10.1016/j.jamcollsurg.2005.03.022
Livingston EH, Ko CY (2004) Socioeconomic characteristics of the population eligible for obesity surgery. Surgery 135:288–296. https://doi.org/10.1016/j.surg.2003.07.008
Martin M, Beekley A, Kjorstad R, Sebesta J (2010) Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. Surg Obes Relat Dis 6:8–15. https://doi.org/10.1016/j.soard.2009.07.003
CDC - BRFSS 2013 Survey Data and Documentation. https://www.cdc.gov/brfss/annual_data/annual_2013.html. Accessed 1 Feb 2019
HCUP-US NIS Overview. https://www.hcup-us.ahrq.gov/nisoverview.jsp#about. Accessed 1 Feb 2019
Surgeon Locator| Health Partner for Weight Loss Surgery. https://weightlosssurgery.thehealthpartner.com/surgeon-locator?utm_source=redirects&utm_medium=realize.com&utm_campaign=301_redirects#!/. Accessed 10 July 2017
Find a LAP-BAND® Specialist | LAP-BAND® http://www.lapband.com/find-a-specialist. Accessed 10 July 2017
Data By Region - Dartmouth Atlas of Health Care. http://www.dartmouthatlas.org/data/region/. Accessed 1 Feb 2019
Cremieux P-Y, Buchwald H, Shikora SA et al (2008) A study on the economic impact of bariatric surgery. Am J Manag Care 14:589–596
Glover J (1938) The incidence of tonsillectomy in school children: (Section of Epidemiology and State Medicine). Proc R Soc Med 31:1219–1236
Surgical Procedures - Dartmouth Atlas of Health Care. http://www.dartmouthatlas.org/data/topic/topic.aspx?cat=22. Accessed 1 Feb 2019
Fuchs VR (1978) The supply of surgeons and the demand for operations. J Hum Resour 13:35–56. https://doi.org/10.2307/145247
Fisher ES (2003) The implications of regional variations in medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med 138:288. https://doi.org/10.7326/0003-4819-138-4-200302180-00007
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs Billmeier, Brickman, and Adrales have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Billmeier, S.E., Atkinson, R.B. & Adrales, G.L. Surgeon presence and utilization of bariatric surgery in the United States. Surg Endosc 34, 2136–2142 (2020). https://doi.org/10.1007/s00464-019-07001-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07001-8