Abstract
Background
A procedure-based laparoscopic liver resection (LLR) classification (IMM classification) stratified 11 different LLR procedures into 3 grades. IMM classification assessed the difficulty of LLR differently than an index-based LLR classification (IWATE criteria), which scored each procedure on an index scale of 12. We validated the difference of 3 IMM grades using an external cohort, evaluated the IMM classification using the scores of the IWATE criteria, and compared the performance of IMM classification with the IWATE criteria and the minor/major classification.
Methods
Patients undergoing LLR without simultaneous procedures were selected from a prospectively maintained database at the Institut Mutualiste Montsouris (IMM cohort) and from the database of 43 Japanese institutions (JMI cohort). Surgical and postoperative outcomes were evaluated according to the 3 IMM grades using the JMI cohort. The 11 LLR procedures included in the IMM classification were scored according to the IWATE criteria. The area under the curves (AUCs) for surgical and postoperative outcomes were compared.
Results
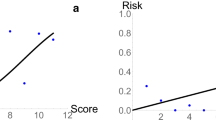
In the JMI (n = 1867) cohort, operative time, blood loss, conversion rate, and major complication rate were significantly associated with a stepwise increase in grades from I to III (all, P < 0.001). In the IMM (n = 433) and JMI cohorts, IMM grades I, II, and III corresponded to three low-scoring, two intermediate-scoring, and six high-scoring LLR procedures as per the IWATE criteria, respectively. Mean ± standard deviation among the IMM grades were significantly different: 3.7 ± 1.4 (grade I) versus 7.5 ± 1.7 (grade II) versus 10.2 ± 1.0 (grade III) (P < 0.001) in the IMM cohort and 3.6 ± 1.4 (grade I) versus 6.7 ± 1.5 (grade II) versus 9.3 ± 1.4 (grade III) (P < 0.001) in the JMI cohort. The AUCs for surgical and postoperative outcomes are higher for the 3-level IMM classification than for the minor/major classification.
Conclusions
The difference of 3 IMM grades with respect to surgical and postoperative outcomes was validated using an external cohort. The 3-level procedure-based IMM classification was in accordance with the index-based IWATE criteria. The IMM classification performed better than the minor/major classification for stratifying LLR procedures.


Similar content being viewed by others
Abbreviations
- LLR:
-
Laparoscopic liver resection
- EBL:
-
Estimated blood loss
- ICCLLR:
-
International consensus conference on laparoscopic liver resection
- IMM:
-
Institut Mutualiste Montsouris
- AL:
-
Anterolateral
- PS:
-
Posterosuperior
- ROC:
-
Receiver-operating characteristics
- AUC:
-
Areas under the receiver-operating characteristics curve
- Wedge-AL:
-
Wedge resection for anterolateral segment
- Wedge-PS:
-
Wedge resection for posterosuperior segment
References
Kaneko H, Takagi S, Otsuka Y, Tsuchiya M, Tamura A, Katagiri T, Maeda T, Shiba T (2005) Laparoscopic liver resection of hepatocellular carcinoma. Am J Surg 189:190–194
Topal B, Fieuws S, Aerts R, Vandeweyer H, Penninckx F (2008) Laparoscopic versus open liver resection of hepatic neoplasms: comparative analysis of short-term results. Surg Endosc 22:2208–2213
Belli G, Limongelli P, Fantini C, D’Agostino A, Cioffi L, Belli A, Russo G (2009) Laparoscopic and open treatment of hepatocellular carcinoma in patients with cirrhosis. Br J Surg 96:1041–1048
Castaing D, Vibert E, Ricca L, Azoulay D, Adam R, Gayet B (2009) Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg 250:849–855
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection-2,804 patients. Ann Surg 250:831–841
Ciria R, Cherqui D, Geller DA, Briceno J, Wakabayashi G (2016) Comparative short-term benefits of laparoscopic liver resection: 9000 cases and climbing. Ann Surg 263:761–777
Kaneko H, Otsuka Y, Kubota Y, Wakabayashi G (2017) Evolution and revolution of laparoscopic liver resection in Japan. Ann Gastroenterol Surg 1:33–43
Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker C-G, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D’Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey J-N, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil R, Belghiti J, Strasberg S, Chari RS (2009) The international position on laparoscopic liver surgery. Ann Surg 250:825–830
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, O’Rourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schon MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J, Strasberg SM (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in morioka. Ann Surg 261:619–629
Ban D, Tanabe M, Ito H, Otsuka Y, Nitta H, Abe Y, Hasegawa Y, Katagiri T, Takagi C, Itano O, Kaneko H, Wakabayashi G (2014) A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci 21:745–753
Tanaka S, Kubo S, Kanazawa A, Takeda Y, Hirokawa F, Nitta H, Nakajima T, Kaizu T, Kaneko H, Wakabayashi G (2017) Validation of a difficulty scoring system for laparoscopic liver resection: a multicenter analysis by the endoscopic liver surgery study group in Japan. J Am Coll Surg 225(249–58):e1
Wakabayashi G (2016) What has changed after the Morioka consensus conference 2014 on laparoscopic liver resection? Hepatobiliary Surg Nutr 5:281–289
Kawaguchi Y, Fuks D, Kokudo N, Gayet B (2018) Difficulty of laparoscopic liver resection: proposal for a new classification. Ann Surg 267:13–17
Jang JS, Cho JY, Ahn S, Han HS, Yoon YS, Choi Y, Kwon SU, Kim S, Guro H (2018) Comparative performance of the complexity classification and the conventional major/minor classification for predicting the difficulty of liver resection for hepatocellular carcinoma. Ann Surg 267:18–23
Lee MKT, Gao F, Strasberg SM (2016) Completion of a liver surgery complexity score and classification based on an international survey of experts. J Am Coll Surg 223:332–342
Lee MKT, Gao F, Strasberg SM (2015) Perceived complexity of various liver resections: results of a survey of experts with development of a complexity score and classification. J Am Coll Surg 220:64–69
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Buchler MW, Weitz J (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group Of Liver Surgery. Surgery 149:680–688
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, Koch M, Makuuchi M, Dematteo RP, Christophi C, Banting S, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Yokoyama Y, Fan ST, Nimura Y, Figueras J, Capussotti L, Buchler MW, Weitz J (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149:713–724
Strasberg SM, Phillips C (2013) Use and dissemination of the brisbane 2000 nomenclature of liver anatomy and resections. Ann Surg 257:377–382
Holm S (1979) A simple secuentially rejective multiple test procedure. Scand J Stat 6:65–70
Bansal S, Buring JE, Rifai N, Mora S, Sacks FM, Ridker PM (2007) Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. JAMA 298:309–316
Mikami S, Hamano T, Fujii N, Nagasawa Y, Isaka Y, Moriyama T, Matsuhisa M, Ito T, Imai E, Hori M (2008) Serum osteoprotegerin as a screening tool for coronary artery calcification score in diabetic pre-dialysis patients. Hypertens Res 31:1163–1170
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458
Halls MC, Berardi G, Cipriani F, Barkhatov L, Lainas P, Harris S, D’Hondt M, Rotellar F, Dagher I, Aldrighetti L, Troisi RI, Edwin B, Abu Hilal M (2018) Development and validation of a difficulty score to predict intraoperative complications during laparoscopic liver resection. Br J Surg 105:1182–1191
Hasegawa Y, Wakabayashi G, Nitta H, Takahara T, Katagiri H, Umemura A, Makabe K, Sasaki A (2017) A novel model for prediction of pure laparoscopic liver resection surgical difficulty. Surg Endosc 31:5356–5363
Abu Hilal M, Aldrighetti L, Dagher I, Edwin B, Troisi RI, Alikhanov R, Aroori S, Belli G, Besselink M, Briceno J, Gayet B, D’Hondt M, Lesurtel M, Menon K, Lodge P, Rotellar F, Santoyo J, Scatton O, Soubrane O, Sutcliffe R, Van Dam R, White S, Halls MC, Cipriani F, Van der Poel M, Ciria R, Barkhatov L, Gomez-Luque Y, Ocana-Garcia S, Cook A, Buell J, Clavien PA, Dervenis C, Fusai G, Geller D, Lang H, Primrose J, Taylor M, Van Gulik T, Wakabayashi G, Asbun H, Cherqui D (2017) The southampton consensus guidelines for laparoscopic liver surgery: from indication to implementation. Ann Surg 268:11–18
Acknowledgements
The authors sincerely thank the surgeons for providing relevant data and valuable insights for the Endoscopic Liver Surgery Study Group in Japan (Supplementary Table 5).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Drs. Yoshikuni Kawaguchi, Shogo Tanaka, David Fuks, Akishige Kanazawa, Yutaka Takeda, Fumitoshi Hirokawa, Hiroyuki Nitta, Takayoshi Nakajima, Takashi Kaizu, Masaki Kaibori, Toru Kojima, Yuichiro Otsuka, Shoji Kubo, Kiyoshi Hasegawa, Norihiro Kokudo, Hironori Kaneko, Go Wakabayashi, and Brice Gayet have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kawaguchi, Y., Tanaka, S., Fuks, D. et al. Validation and performance of three-level procedure-based classification for laparoscopic liver resection. Surg Endosc 34, 2056–2066 (2020). https://doi.org/10.1007/s00464-019-06986-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06986-6