Abstract
Introduction
The purpose of this study is to evaluate the utility of using a functional lumen imaging probe (EndoFLIP™) intra-operatively during hiatal hernia repair and fundoplication. Additionally, we hypothesize that these measurements correlate with long-term outcomes.
Methods
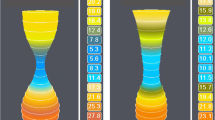
A prospectively maintained quality database was queried. Between 2013 and 2018, 175 patients underwent laparoscopic fundoplication, the majority of which also had a hiatal hernia repair. The EndoFLIP™ was used to measure minimum diameter (Dmin), balloon pressure, and distensibility index (DI) at different timepoints throughout the operation. Clinical outcomes were measured up to 2 years after treatment.
Results
Crural closure and fundoplication resulted in a significant increase in balloon pressure and decrease in DI when compared to initial measurements as well as measurements taken after hernia reduction. After 1 year, patients with a final DI < 2.0 mm2/mmHg reported significantly more gas bloat and dysphagia than those with a final DI ≥ 2.0 mm2/mmHg (p = 0.040 and p = 0.025, respectively). This disparity became even more dramatic at 2 years (p = 0.006 and p = 0.004, respectively), with a final DI < 2.0 mm2/mmHg being significantly associated with higher prevalence of daily gas bloat (43.8% vs. 12.0%; p = 0.03). Additionally, patients with a final DI between 2.0 and 3.5 mm2/mmHg reported significantly lower Reflux Symptom Index scores at one year compared to those with a final DI < 2.0 or > 3.5 mm2/mmHg (p = 0.042).
Conclusion
EndoFLIP™ measurements correlate well with patient outcomes, with a final DI between 2 and 3.5 mm2/mmHg potentially being ideal. The EndoFLIP™ can be a useful adjunct in the operating room by providing objective measurements of esophageal distensibility after crural closure and fundoplication.






Similar content being viewed by others

References
Richter JE, Rubenstein JH (2018) Presentation and epidemiology of gastroesophageal reflux disease. Gastroenterology 154:267–276
Dodds WJ, Dent J, Hogan WJ, Helm JF, Hauser R, Patel GK, Egide MS (1982) Mechanisms of gastroesophageal reflux in patients with reflux esophagitis. N Engl J Med 307:1547–1552
Mehta S, Bennett J, Mahon D, Rhodes M (2006) Prospective trial of laparoscopic nissen fundoplication versus proton pump inhibitor therapy for gastroesophageal reflux disease: seven-year follow-up. J Gastrointest Surg 10:1312–1316 (discussion 1316)
Dallemagne B, Weerts J, Markiewicz S, Dewandre JM, Wahlen C, Monami B, Jehaes C (2006) Clinical results of laparoscopic fundoplication at ten years after surgery. Surg Endosc 20:159–165
Humphries LA, Hernandez JM, Clark W, Luberice K, Ross SB, Rosemurgy AS (2013) Causes of dissatisfaction after laparoscopic fundoplication: the impact of new symptoms, recurrent symptoms, and the patient experience. Surg Endosc 27:1537–1545
Patterson EJ, Herron DM, Hansen PD, Ramzi N, Standage BA, Swanström LL (2000) Effect of an esophageal bougie on the incidence of dysphagia following nissen fundoplication: a prospective, blinded, randomized clinical trial. Arch Surg 135:1055–1061 (discussion 1061)
Catarci M, Gentileschi P, Papi C, Carrara A, Marrese R, Gaspari AL, Grassi GB (2004) Evidence-based appraisal of antireflux fundoplication. Ann Surg 239:325–337
Yadlapati R, Hungness ES, Pandolfino JE (2018) Complications of antireflux surgery. Am J Gastroenterol 113:1137–1147
Richter JE (2013) Gastroesophageal reflux disease treatment: side effects and complications of fundoplication. Clin Gastroenterol Hepatol 11:465–471 (quiz e39)
Kwiatek MA, Pandolfino JE, Hirano I, Kahrilas PJ (2010) Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc 72:272–278
Kwiatek MA, Kahrilas K, Soper NJ, Bulsiewicz WJ, McMahon BP, Gregersen H, Pandolfino JE (2010) Esophagogastric junction distensibility after fundoplication assessed with a novel functional luminal imaging probe. J Gastrointest Surg 14:268–276
Ilczyszyn A, Botha AJ (2014) Feasibility of esophagogastric junction distensibility measurement during Nissen fundoplication. Dis Esophagus 27:637–644
Belafsky PC, Postma GN, Koufman JA (2002) Validity and reliability of the reflux symptom index (RSI). J Voice 16:274–277
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 20:130–134
Pandolfino JE, Shi G, Curry J, Joehl RJ, Brasseur JG, Kahrilas PJ (2002) Esophagogastric junction distensibility: a factor contributing to sphincter incompetence. Am J Physiol Gastrointest Liver Physiol 282:G1052–G1058
Kim MP, Meisenbach LM, Chan EY (2018) Tailored fundoplication with endoluminal functional lumen imaging probe allows for successful minimally invasive hiatal hernia repair. Surg Laparosc Endosc Percutan Tech 28:178–182
DeHaan RK, Davila D, Frelich MJ, Gould JC (2017) Esophagogastric junction distensibility is greater following Toupet compared to Nissen fundoplication. Surg Endosc 31:193–198
Pandolfino JE, de Ruigh A, Nicodème F, Xiao Y, Boris L, Kahrilas PJ (2013) Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP™) in achalasia patients. Neurogastroenterol Motil 25:496–501
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Michael B. Ujiki is a speaker for Medtronic, consultant for Olympus, on the Boston Scientific advisory board, a consultant and speaker for Apollo Medical Devices and a speaker for Gore Medical. Dr. Bailey Su, Ms. Stephanie Novak, Dr. Zachary M. Callahan, Ms. Kristine Kuchta and Ms. JoAnn Carbray have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Su, B., Novak, S., Callahan, Z.M. et al. Using impedance planimetry (EndoFLIP™) in the operating room to assess gastroesophageal junction distensibility and predict patient outcomes following fundoplication. Surg Endosc 34, 1761–1768 (2020). https://doi.org/10.1007/s00464-019-06925-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06925-5